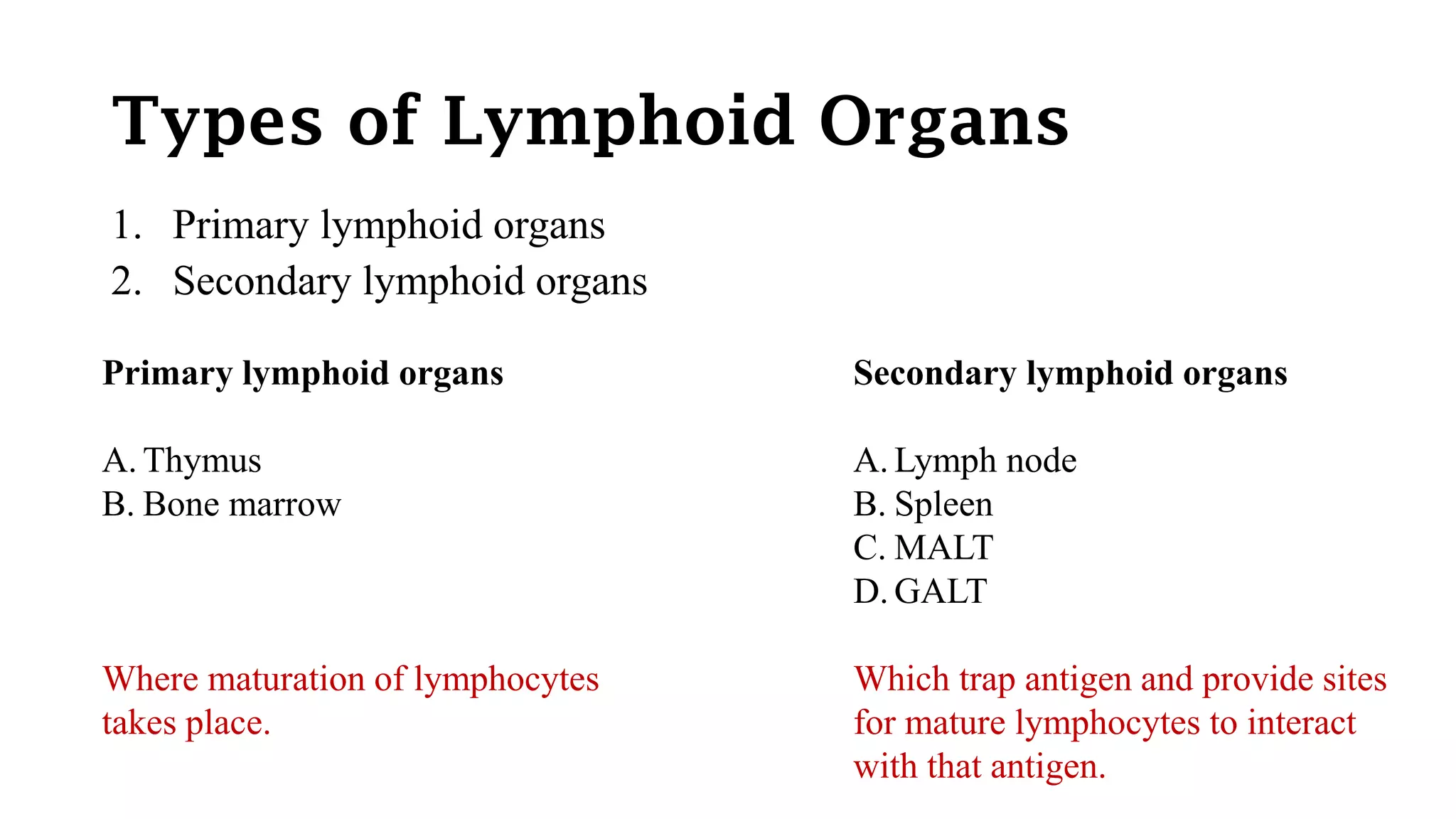
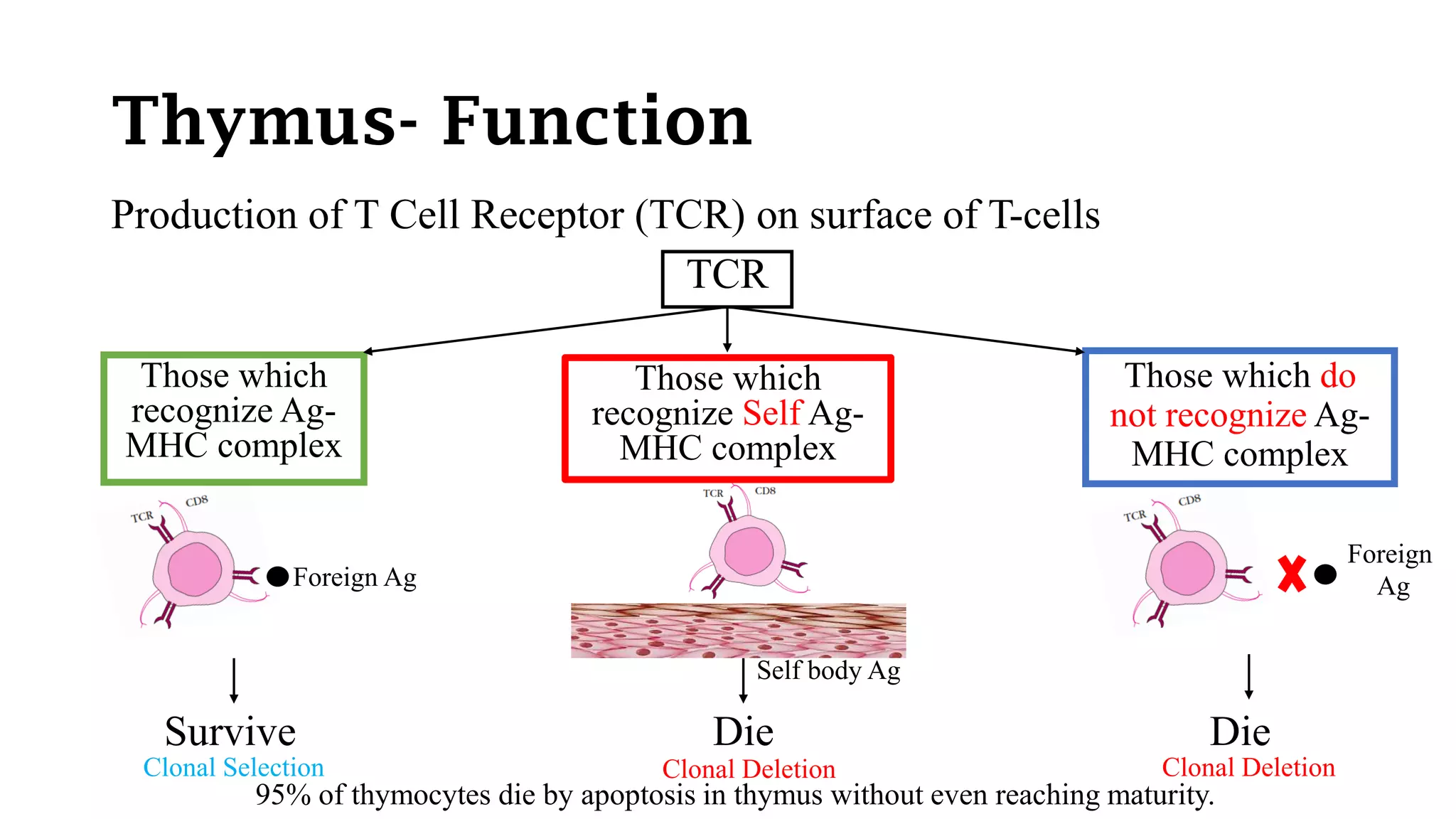
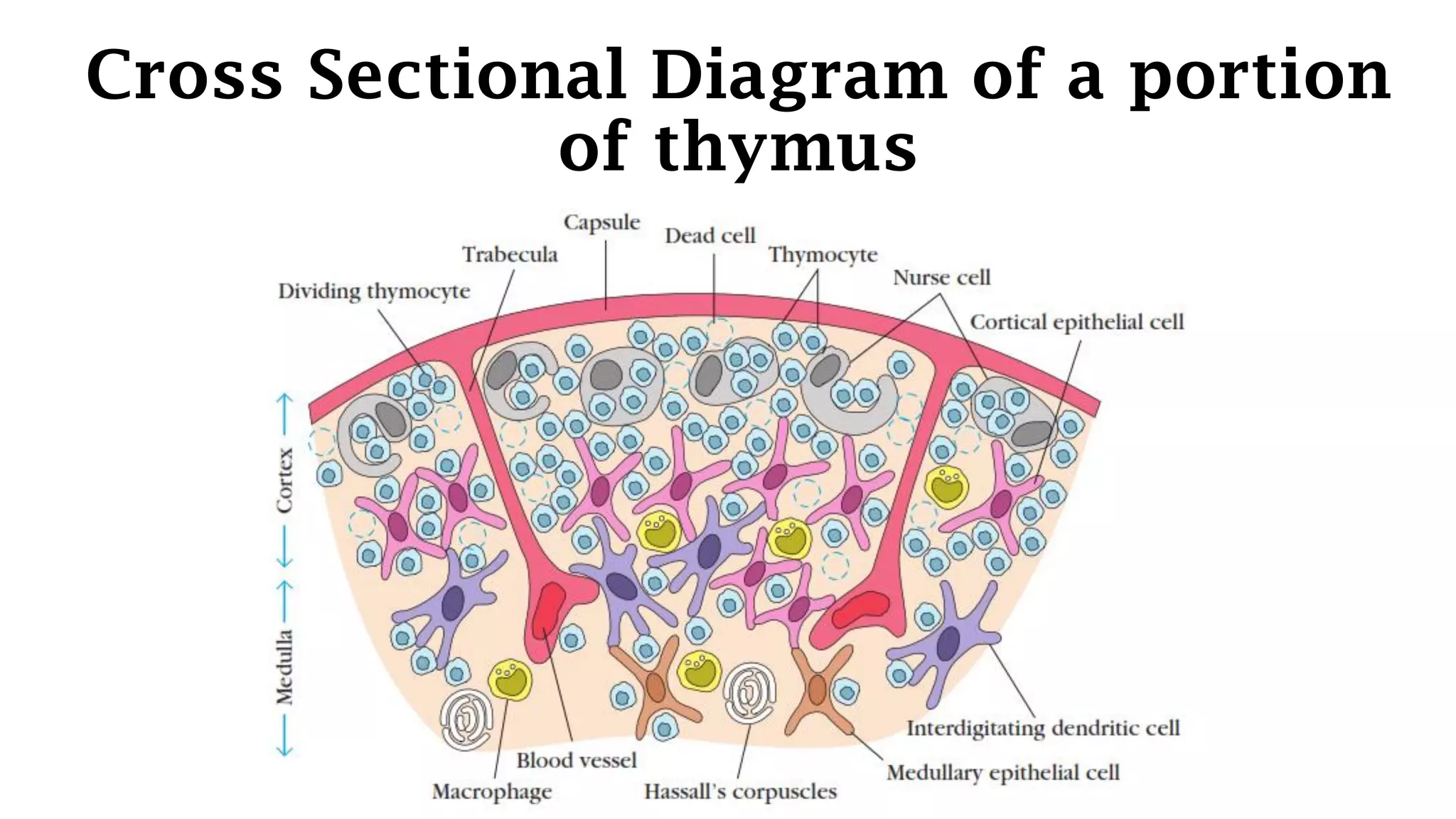
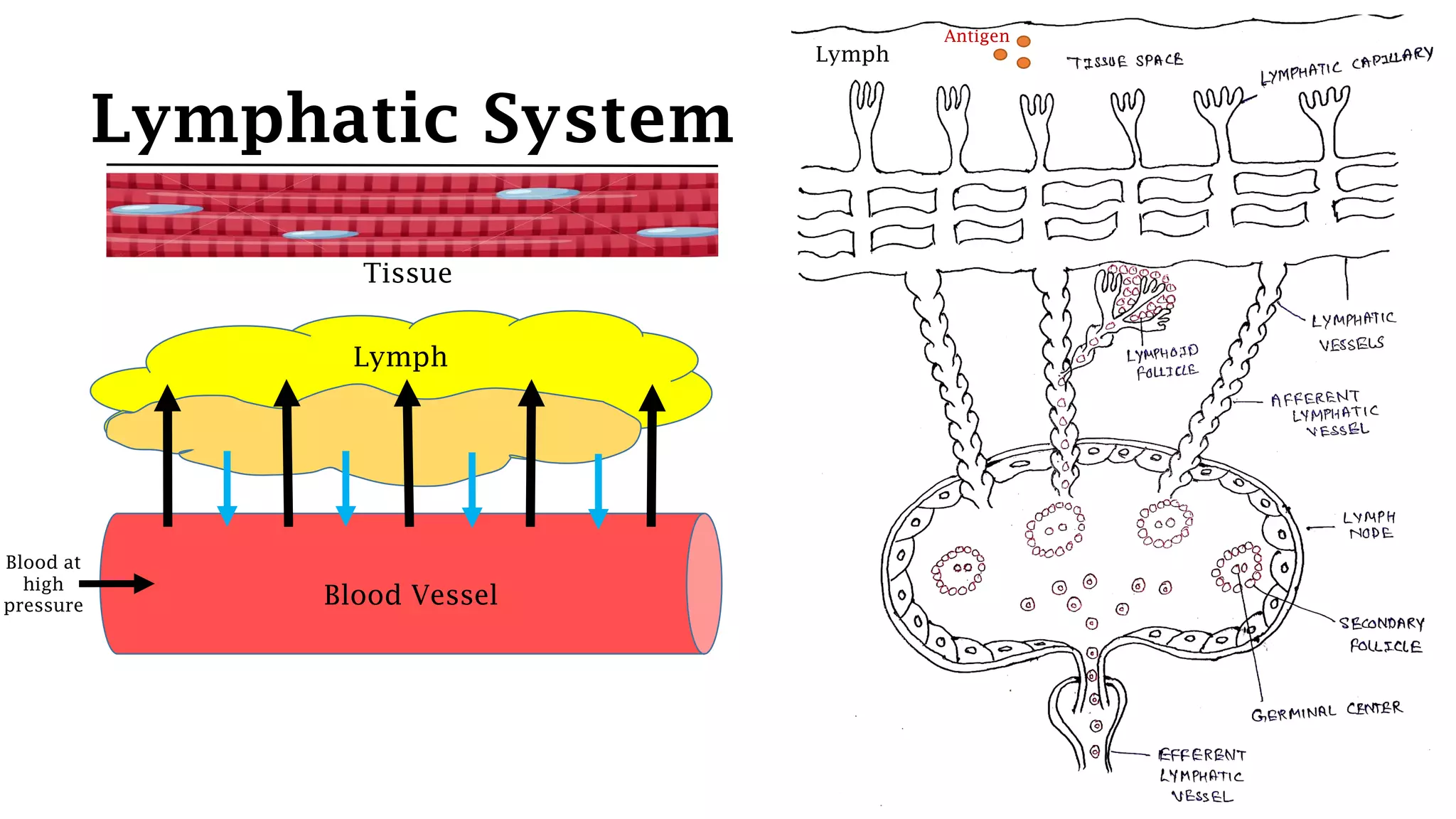
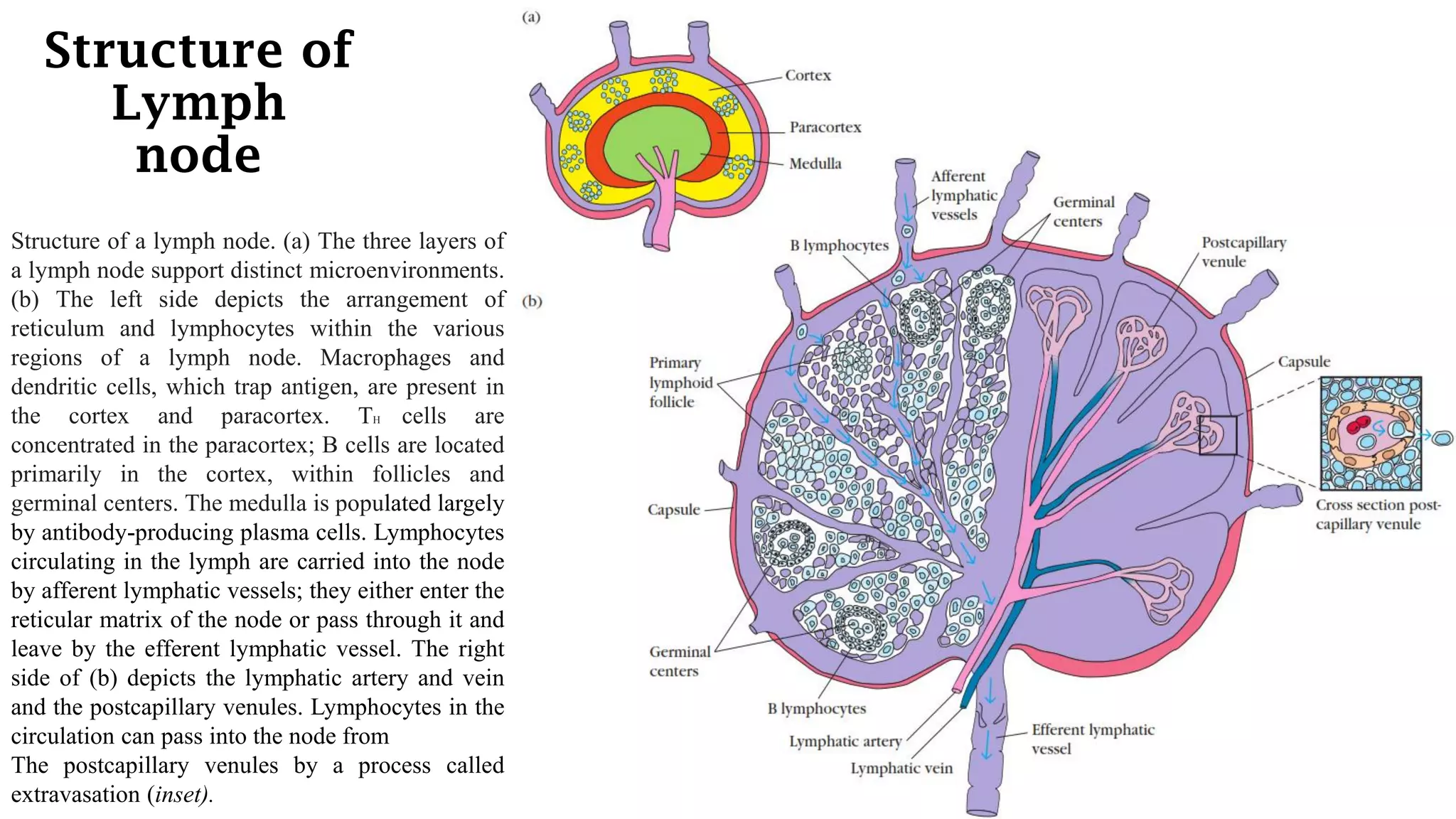
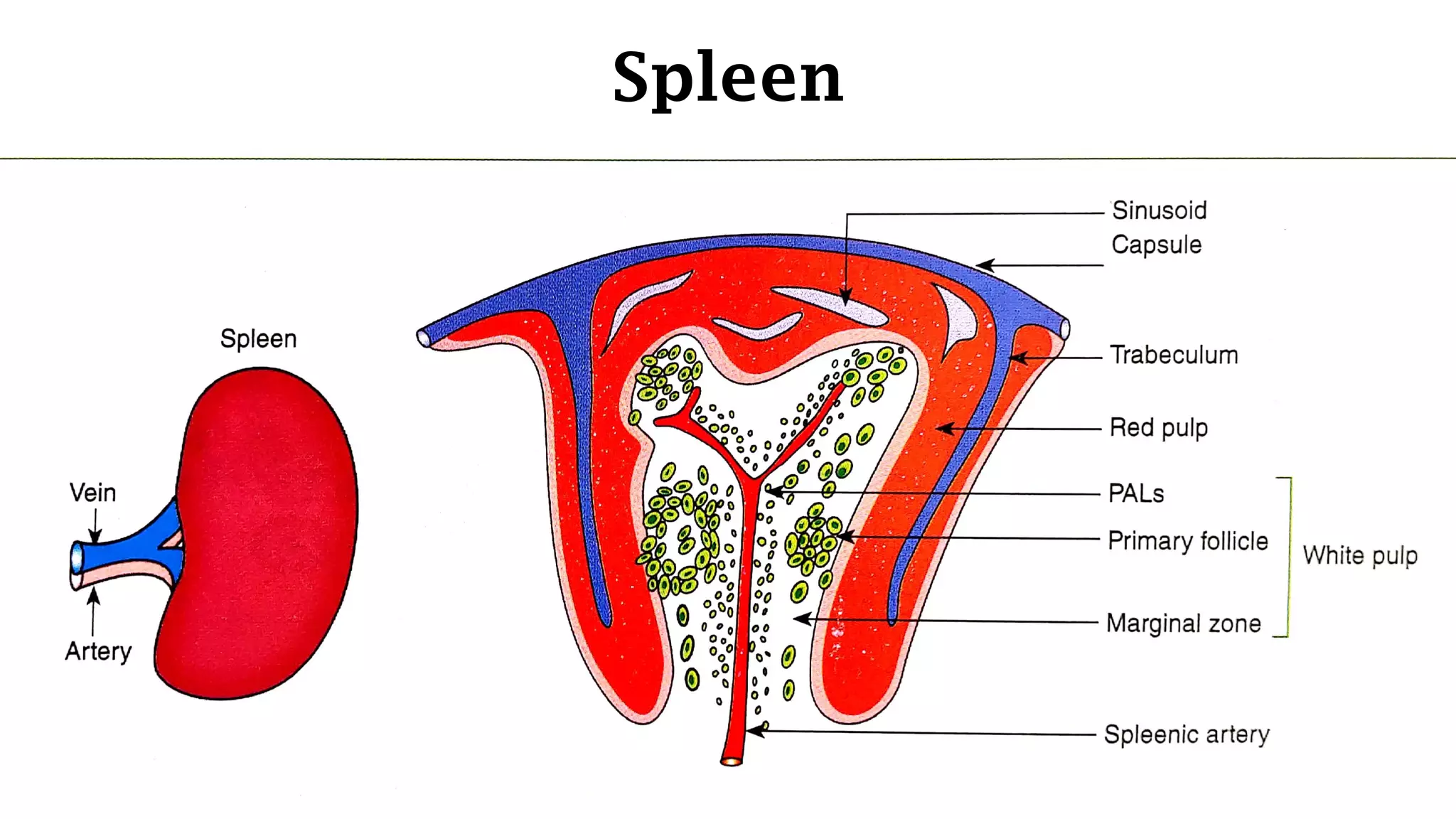
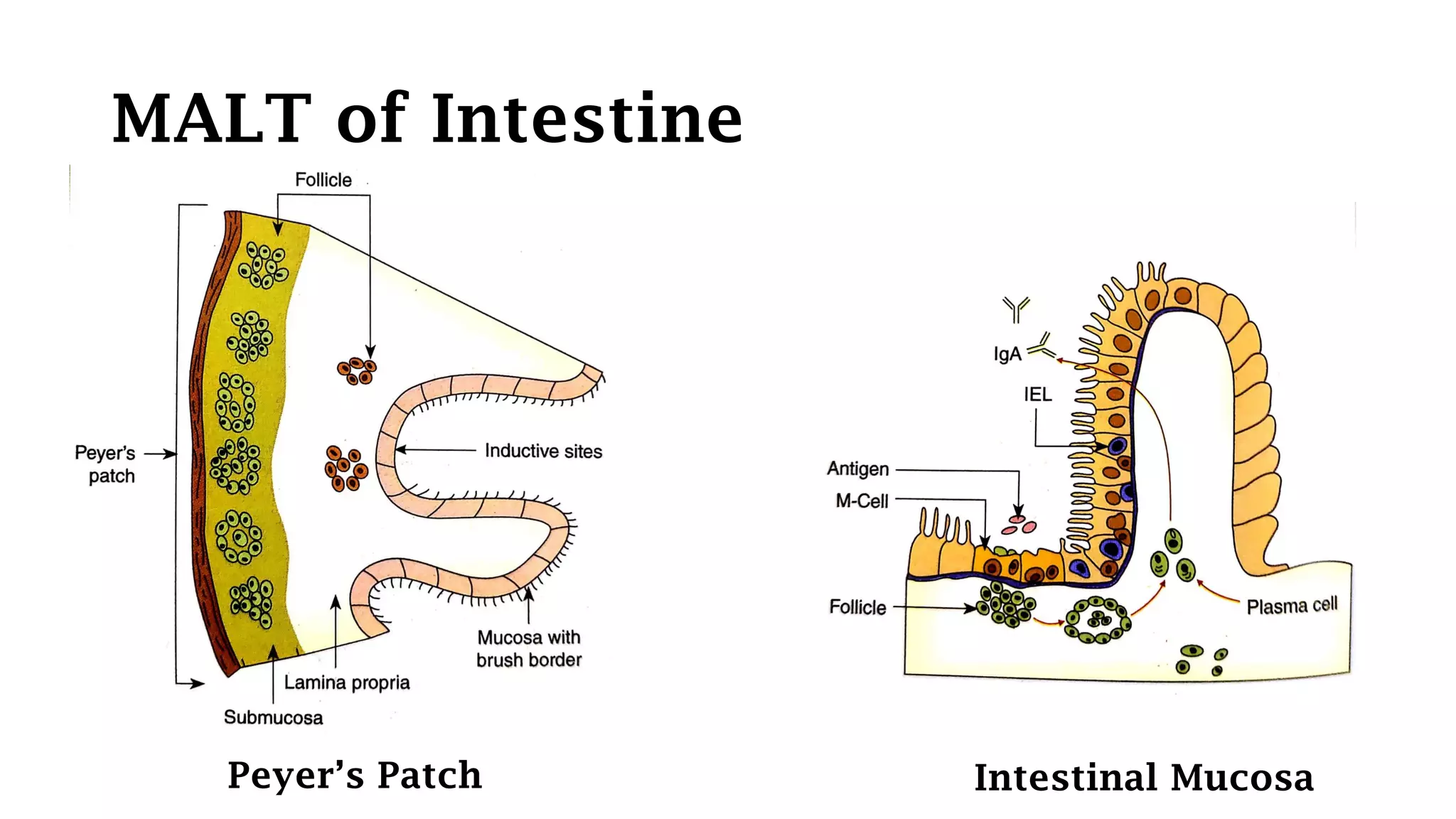
The document summarizes the major lymphoid organs of the immune system. It describes the primary lymphoid organs, the thymus and bone marrow, where lymphocyte maturation occurs. The secondary lymphoid organs, lymph nodes, spleen, MALT and GALT, trap antigens and allow interactions between lymphocytes and antigens. The thymus specifically mediates T cell maturation and selection, while lymph nodes contain B cell follicles and T cell zones to initiate adaptive immune responses to lymph-borne pathogens and antigens.