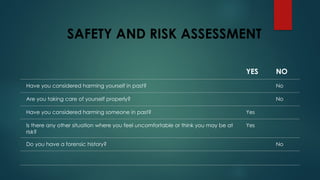
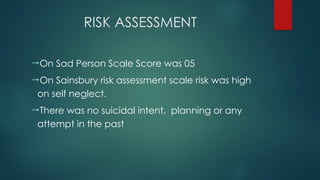
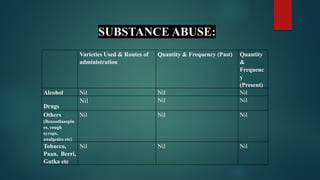
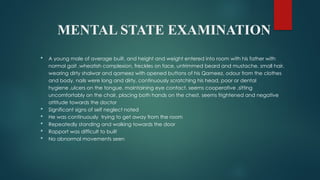
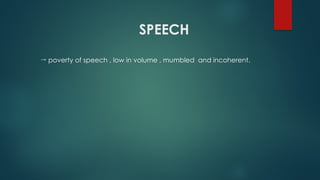
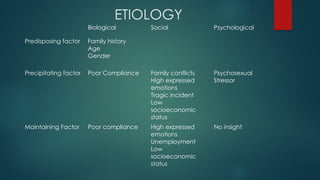
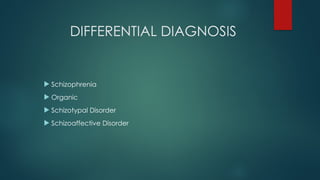
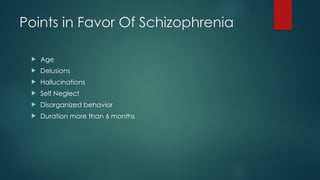
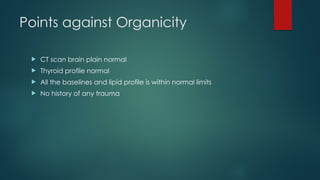
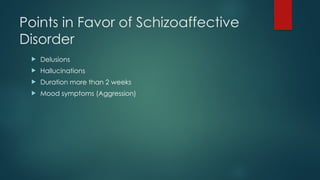
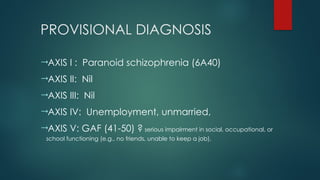
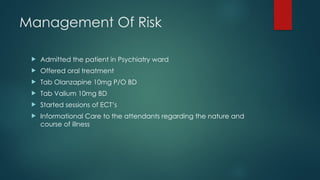
The document presents a detailed case study of a 23-year-old male, Mr. Sadam Hussain, who has been admitted for psychiatric evaluation and treatment due to symptoms of paranoid schizophrenia, including aggression, self-neglect, and delusions. His psychiatric history includes previous treatments with limited compliance, resulting in a recurrence of symptoms. The management plan includes hospitalization, medications, and family therapy, with a mixed prognosis influenced by family support and individual circumstances.