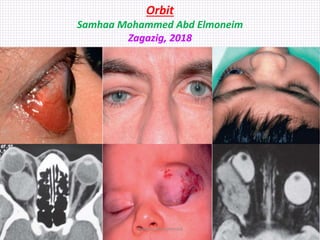
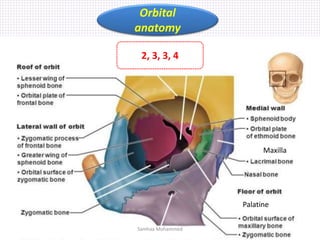
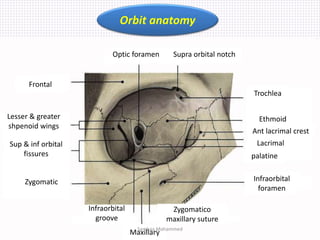
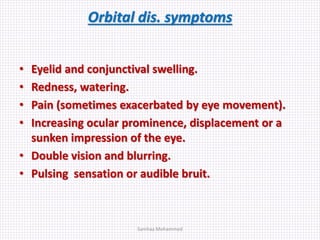
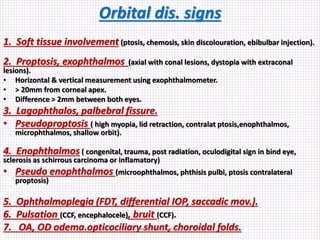
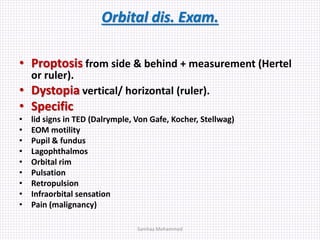
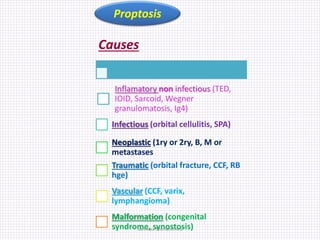
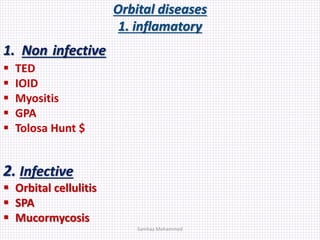
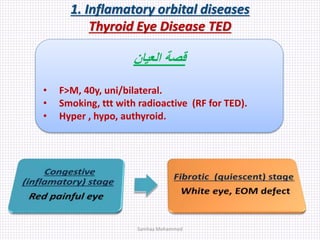
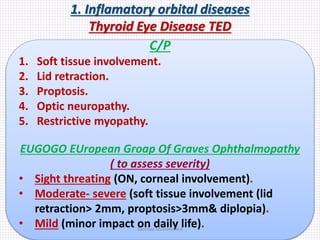
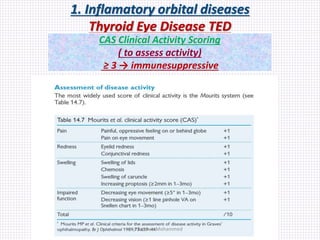
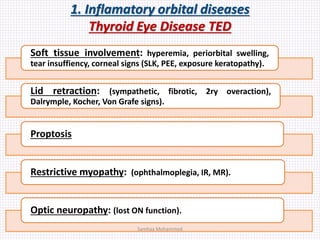
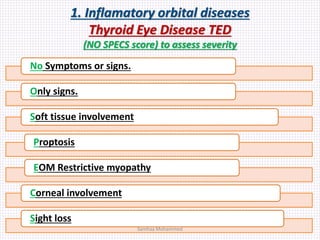
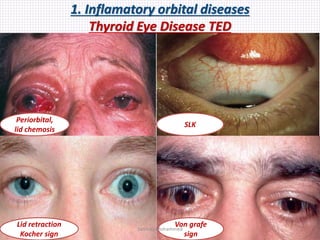
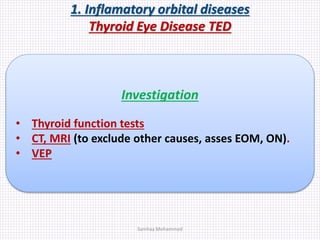
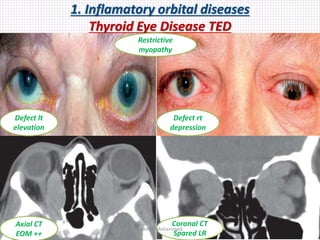
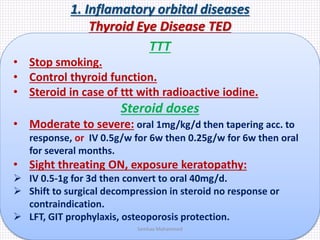
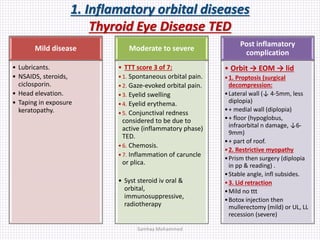
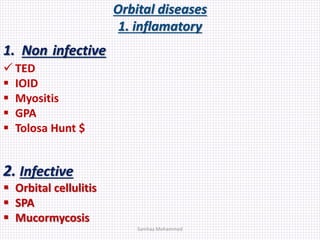
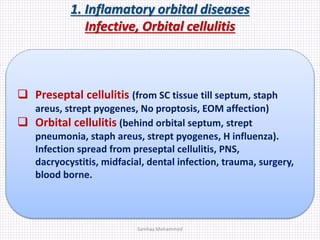
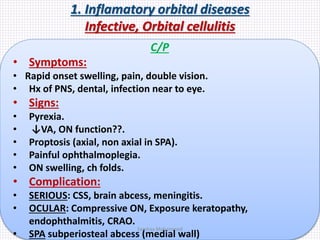
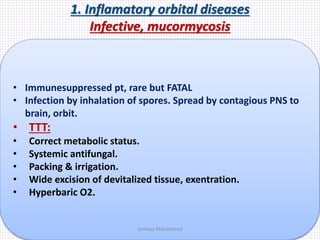
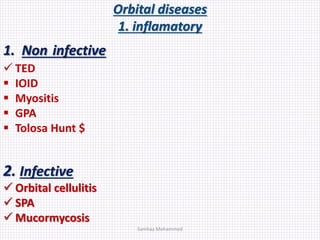
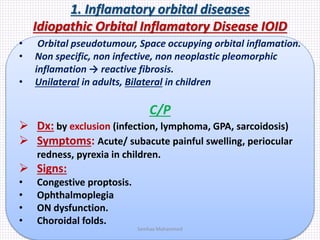
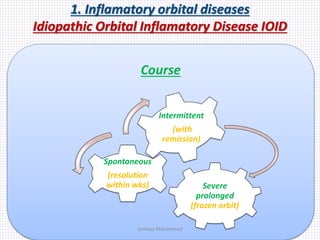
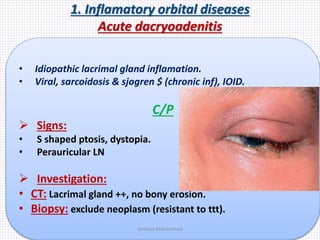
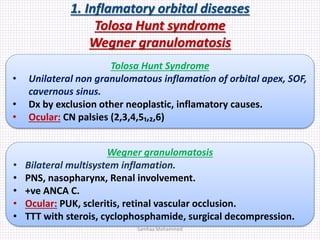
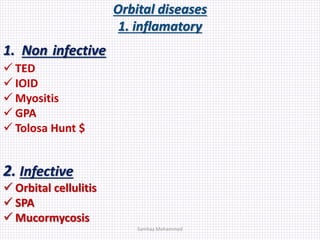
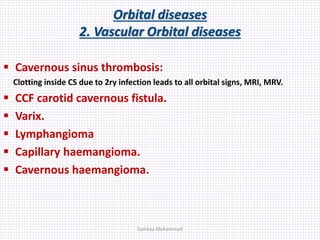
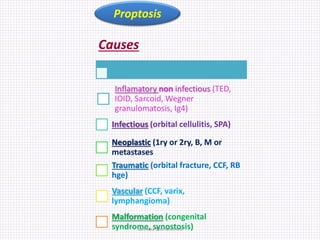
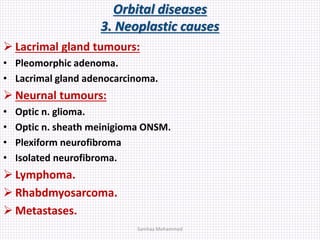
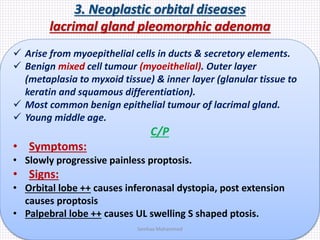
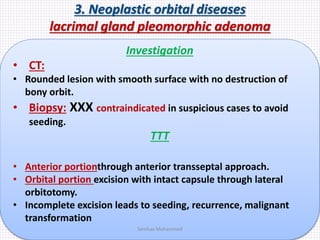
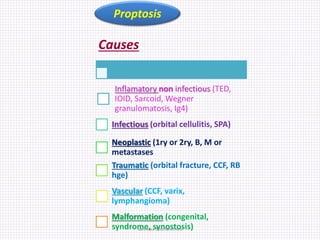
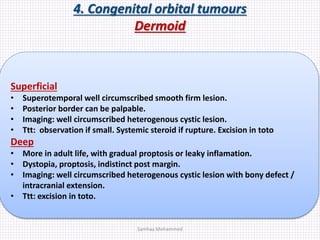
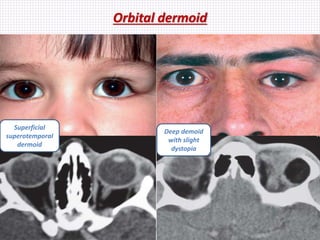
This document summarizes orbital anatomy and various orbital diseases. It describes the anatomy of orbital structures like bones, foramina and fissures. It then discusses symptoms, signs, investigations and treatment of various inflammatory orbital diseases including thyroid eye disease, idiopathic orbital inflammatory disease, orbital cellulitis, subperiosteal abscess and mucormycosis. It also briefly mentions other conditions like orbital myositis, dacryoadenitis and Tolosa-Hunt syndrome.