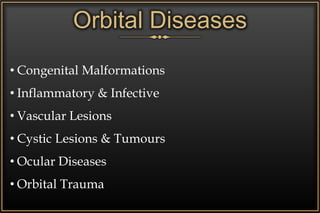
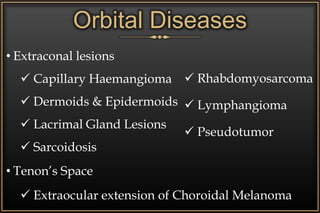
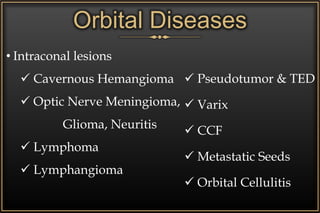
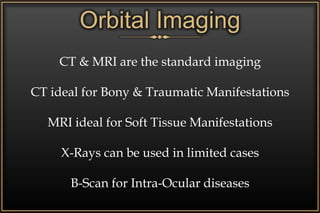
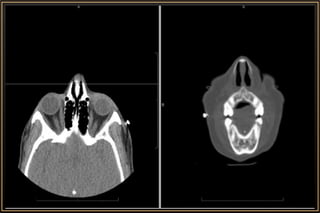
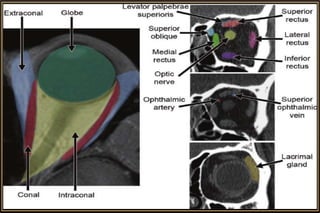
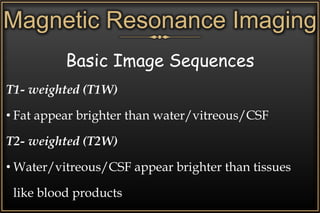
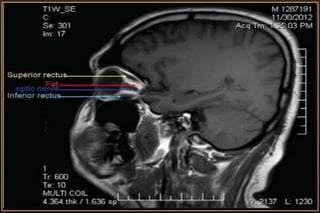
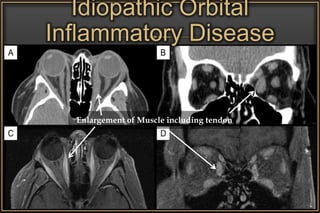
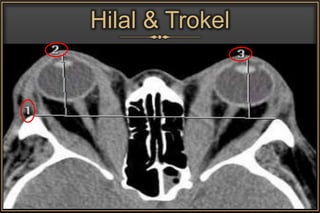
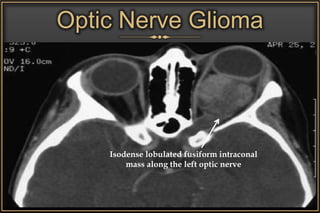
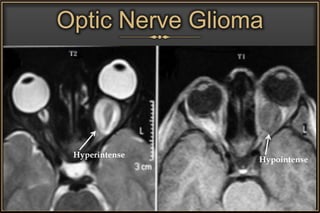
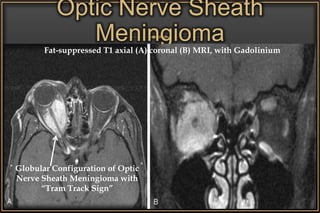
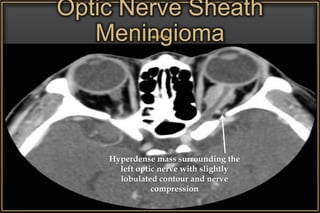
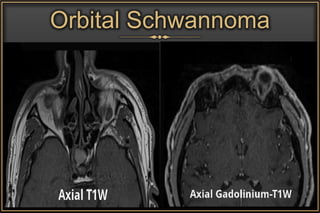
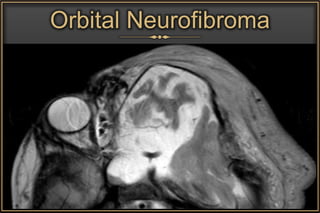
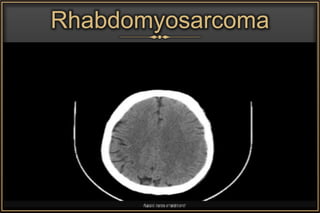
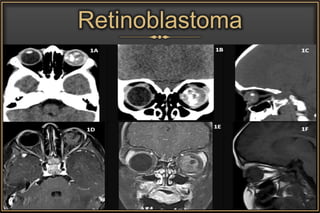
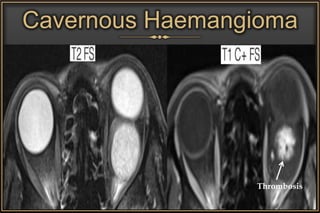
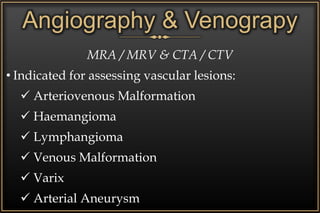
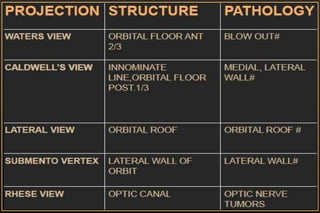
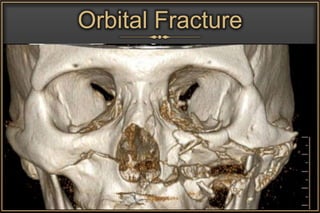
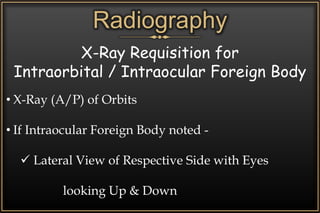
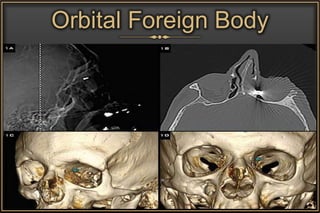
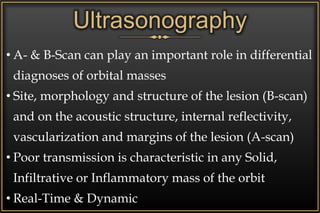
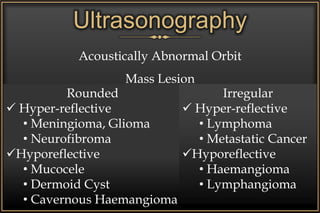
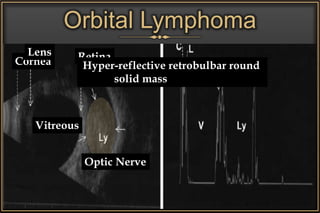
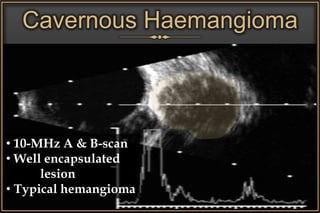
The document discusses imaging in orbital diseases, covering modalities such as radiography, ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI). It highlights various orbital diseases, their anatomical considerations, and detailed imaging characteristics useful for diagnosis. CT is favored for bony manifestations, while MRI is preferred for soft tissue, with advanced imaging techniques available for complex lesions.