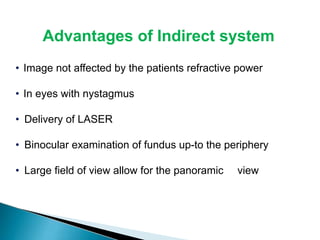
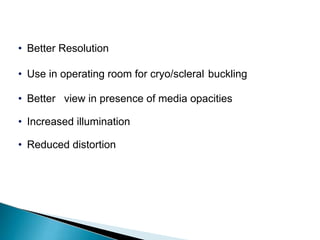
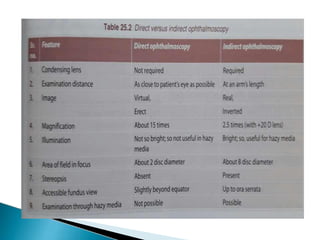
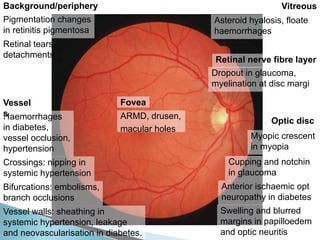
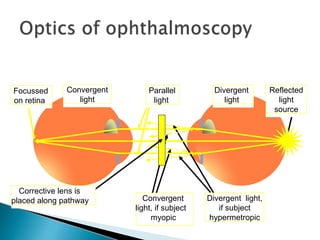
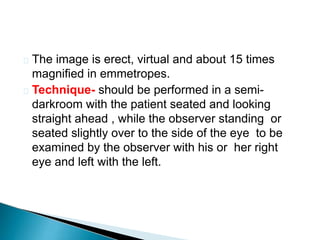
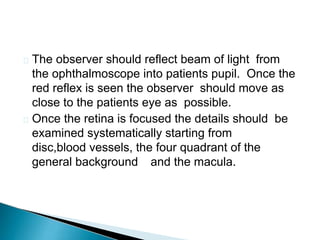
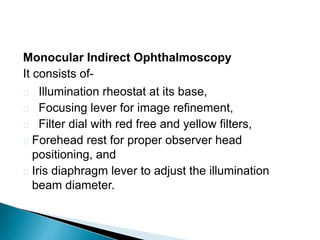
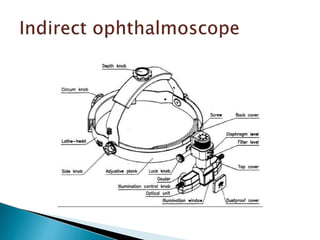
The document discusses various techniques for examining the interior of the eye including ophthalmoscopy. It describes the indirect ophthalmoscopy technique where a convex lens is used to make the eye highly myopic, allowing examination of the retina. The key steps of the technique are outlined including using a dark room, convex lens, illumination source and obtaining an inverted, magnified view of the retina between the lens and examiner's eye. Advantages of indirect ophthalmoscopy are also provided.
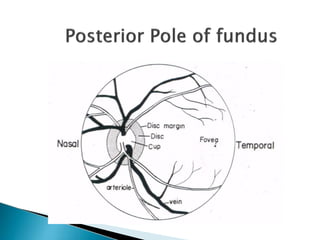
![DISC: LOCATION –nasal to geometric axis
DIAMETER – 1.5mm [1 disc diameter]
COLO
R
SHAPE
– Pale pink
– Circular
EDGES – Regular
CUP
:
TERMINATION OF
ALL LAYERS EXCEPT
NFL
C/D ratio – 0.3 to 0.5](https://image.slidesharecdn.com/opthalmoscopy-240209030514-2d3f40f8/85/OPTHALMOSCOPY-pdf-5-320.jpg)

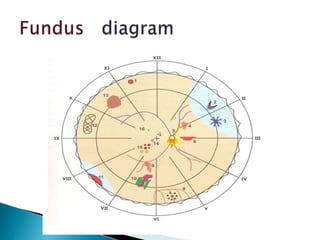
![ FUNDUS DRAWING-
The image seen with IO is vertically inverted and
laterally reversed; top of the retinal chart is placed
towards the foot end of the patient [i.e.upside down]
Fundus drawing is made on a special Amsler
chart,which has 12 clock hours marked and has
three concentric circles made on it-
Innermost circle,middle circle and outermost circle
represents to the equator,the ora serrata and,the
midpoint of pars plana respectively.](https://image.slidesharecdn.com/opthalmoscopy-240209030514-2d3f40f8/85/OPTHALMOSCOPY-pdf-37-320.jpg)