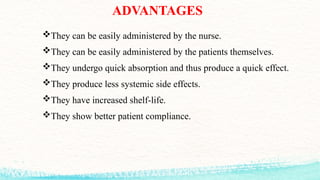
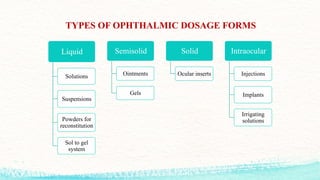
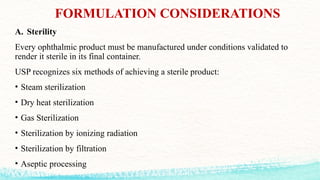
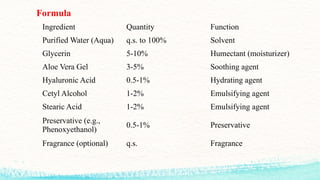
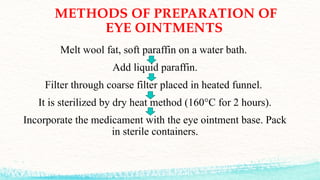
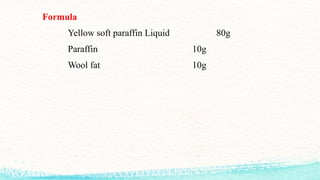
The document provides a comprehensive overview of ophthalmic preparations, detailing their characteristics, advantages, disadvantages, types, formulation considerations, and quality control measures. It covers various dosage forms such as eye drops, eye lotions, and ointments, along with their preparation processes and packaging requirements. Important aspects like sterility, ocular toxicity, preservatives, and testing for quality control are also discussed to ensure effective and safe ophthalmic products.