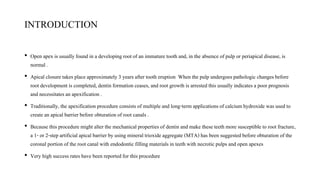
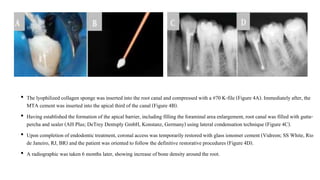
1) The document reports on two case studies where lyophilized collagen sponges were used as an apical matrix prior to placing mineral trioxide aggregate (MTA) as an apical plug in teeth with open apices and necrotic pulps. In both cases, the MTA plug demonstrated favorable outcomes with regression of periapical lesions and increase in bone density.
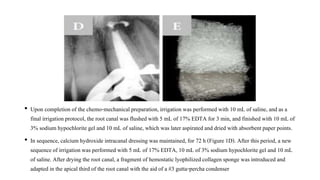
2) The use of a collagen sponge matrix allows for the hydration and setting of MTA to occur without direct contact of MTA with apical tissues, preventing inflammatory reactions. The collagen sponge is also easily handled and promotes healing.
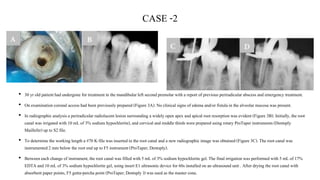
3) Placement of MTA with a collagen sponge matrix results in a safe





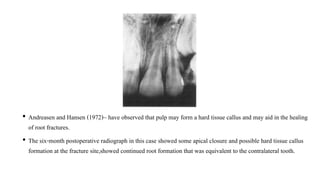

![REFERENCES
• Graziele Magro M, Carlos Kuga M, Adad Ricci W, Cristina Keine K, Rodrigues Tonetto M, Linares Lima
S, Henrique Borges A, Garcia Belizário L, Coêlho Bandeca M. Endodontic Management of Open Apex
Teeth Using Lyophilized Collagen Sponge and MTA Cement: Report of Two Cases. Iran Endod J.
2017;12(2):248-52. Doi: 10.22037/iej.2017.48
• M.Torabinejad, et al Revitalization of Tooth with Necrotic Pulp and Open Apex by Using PRP JOE —
Volume 37, Number 2, February 2011
• Nevins.A et al , hard tissue induction into pulpless open-apex teeth using collagen-calcium phosphate gel
journal of endodontics ] vol 0, no 11, november 1977](https://image.slidesharecdn.com/openapex2021-210705140459/85/OPEN-APEX-28-320.jpg)