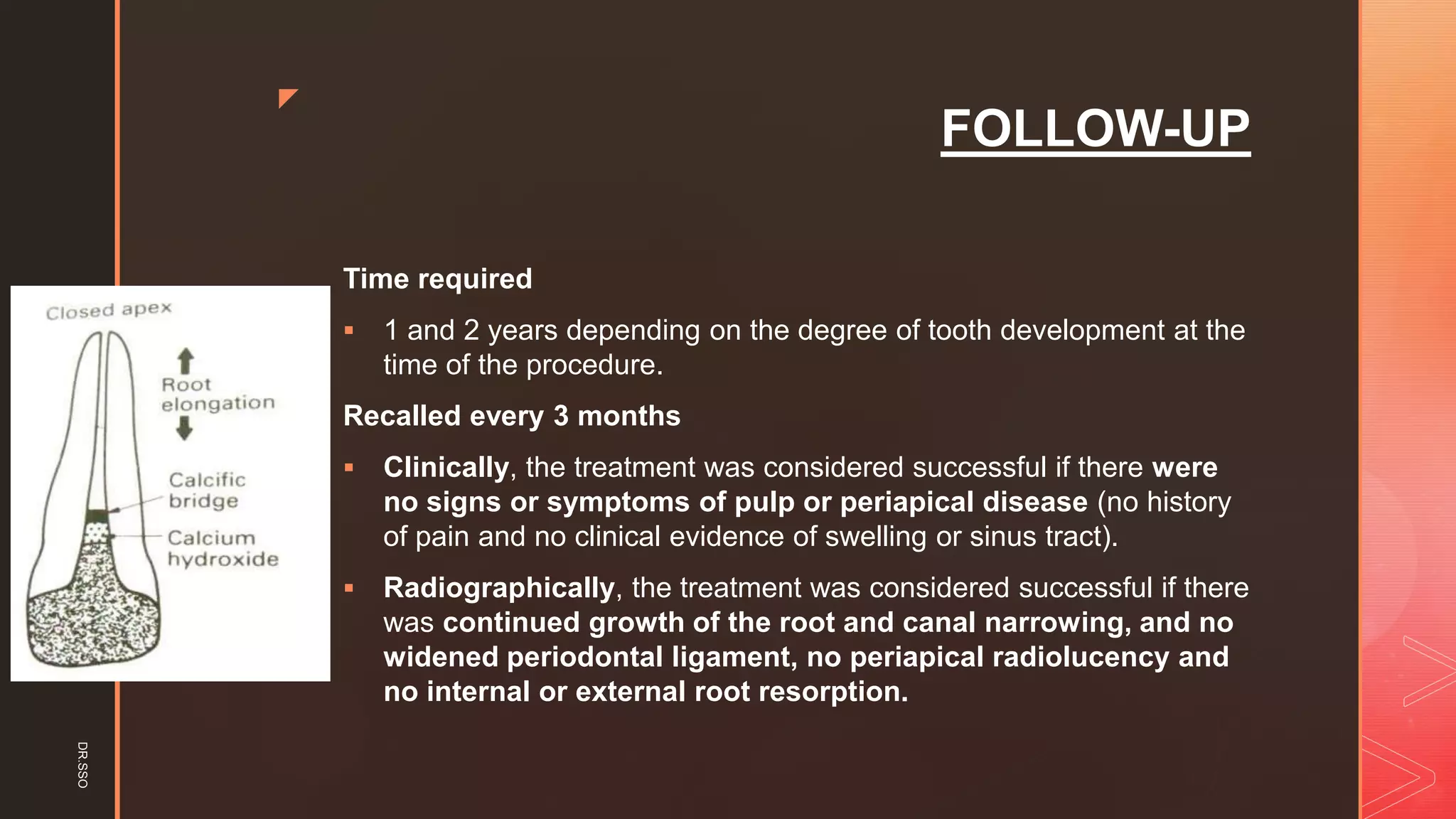
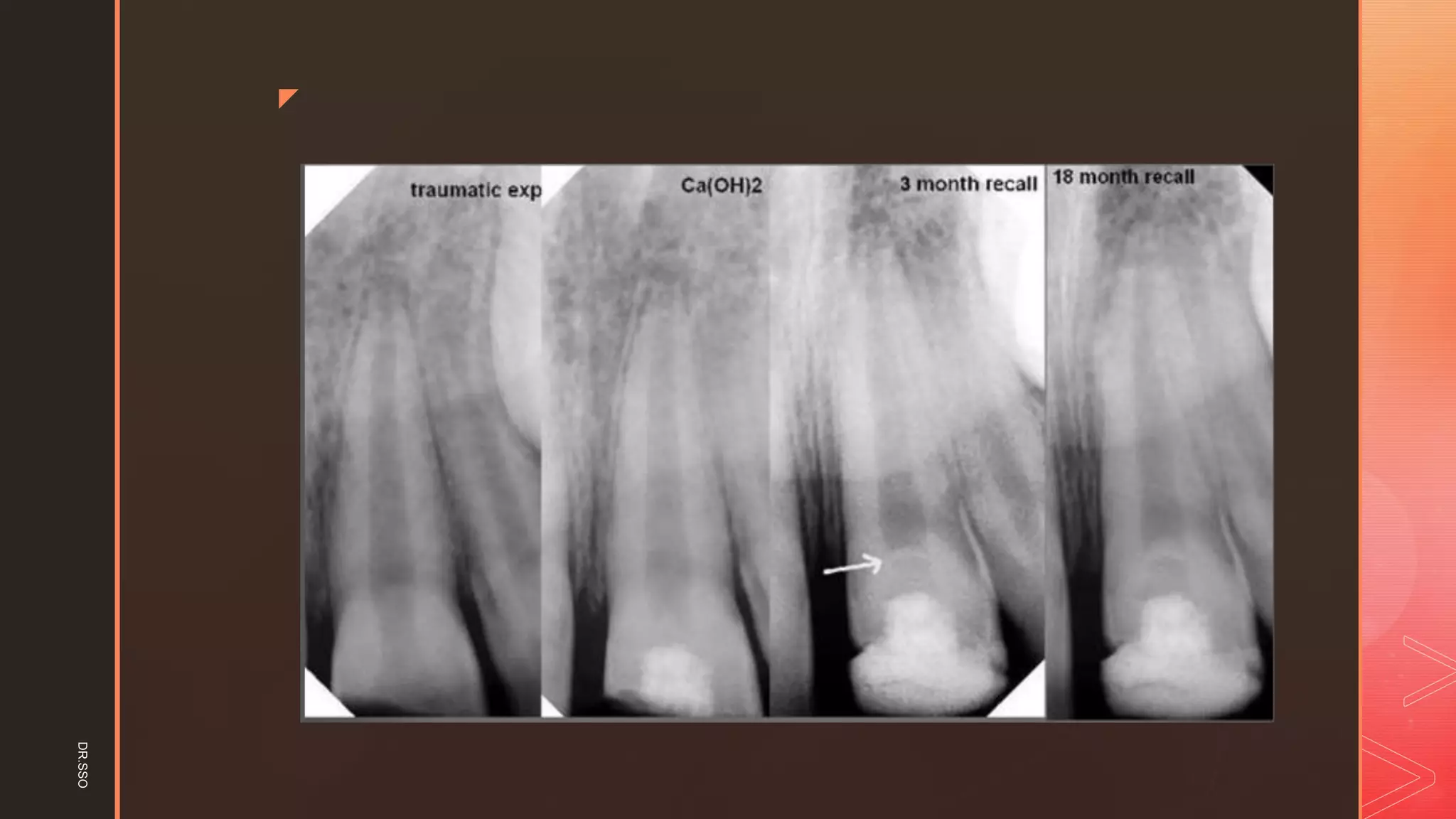
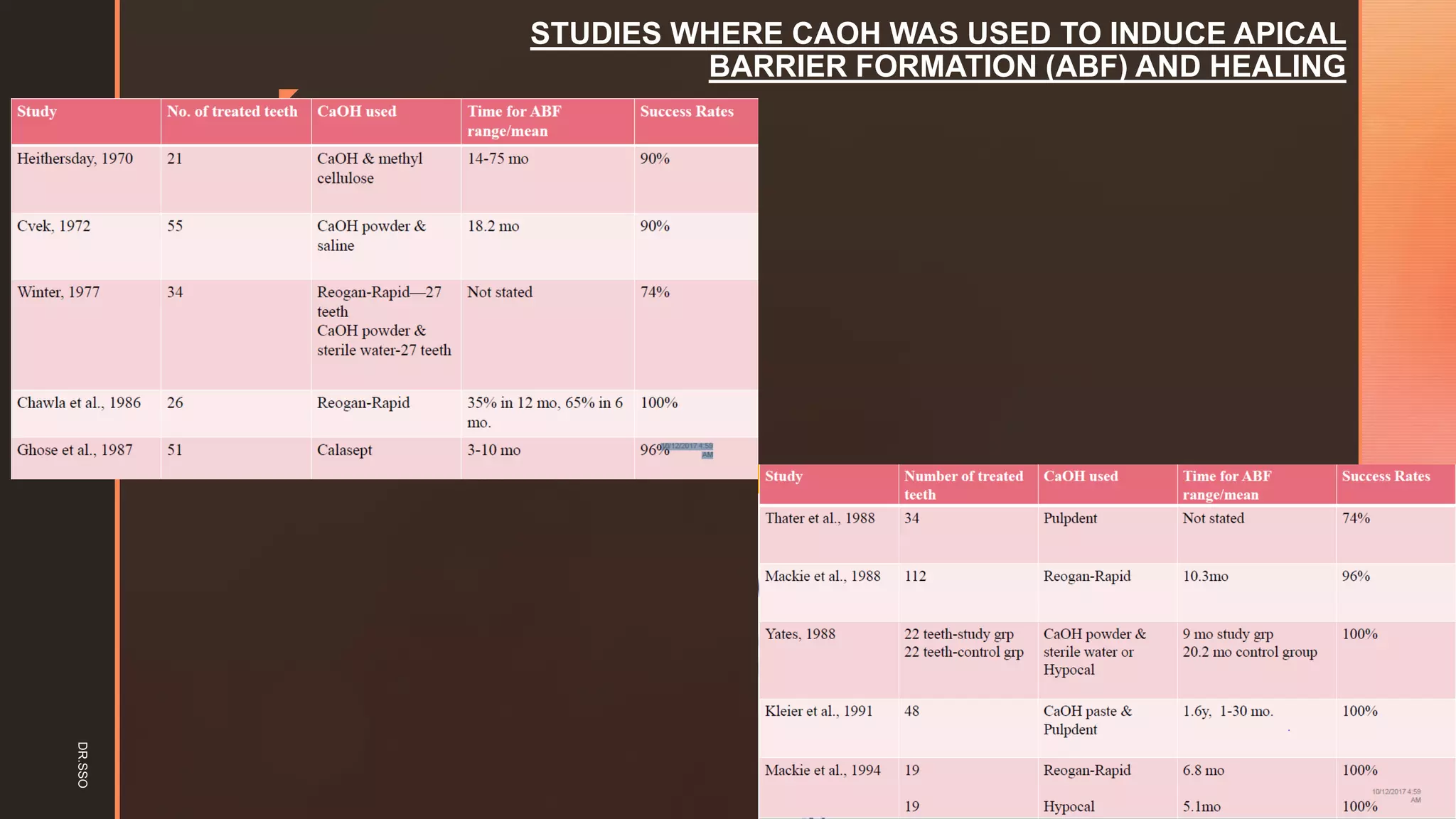
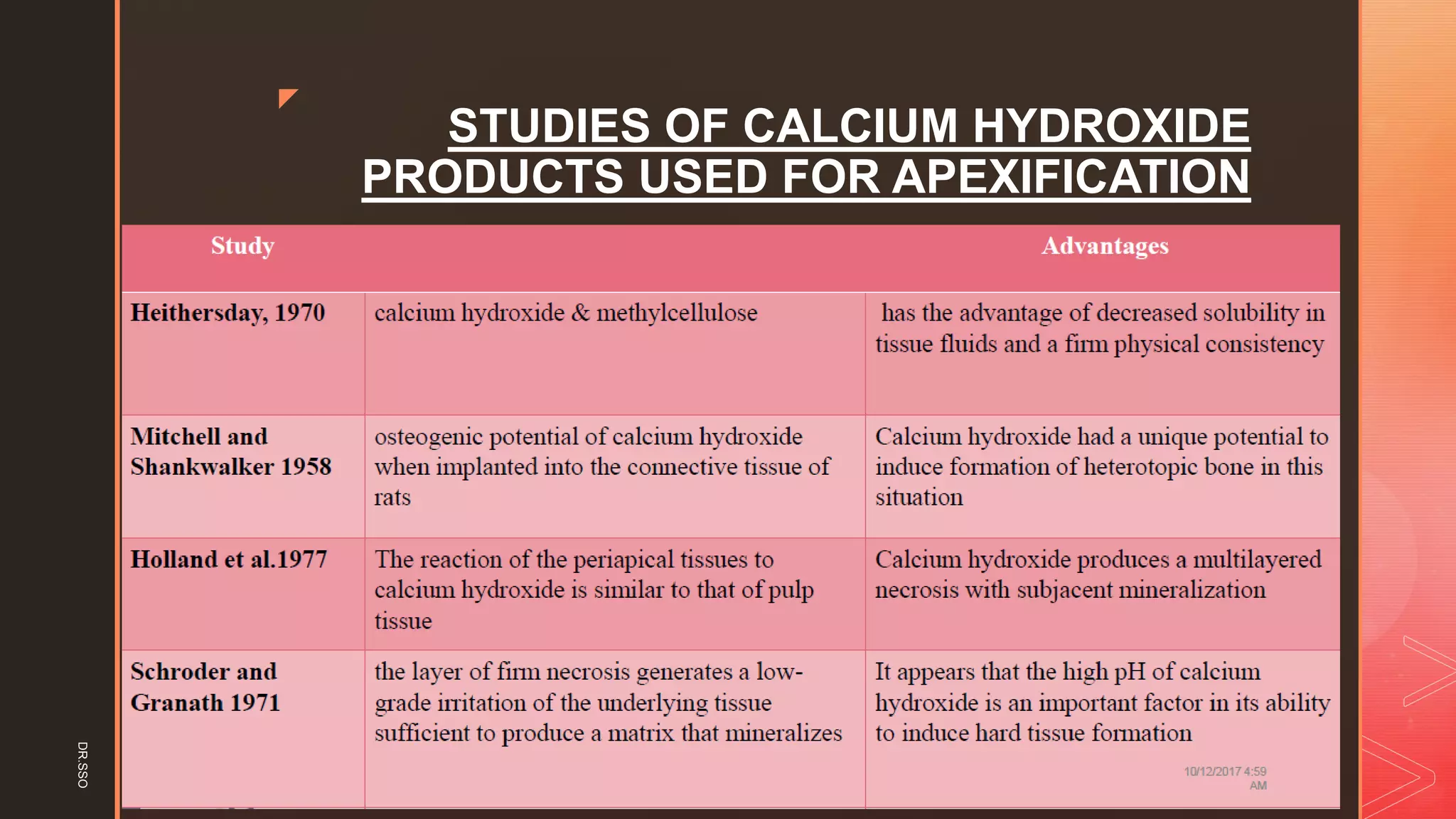
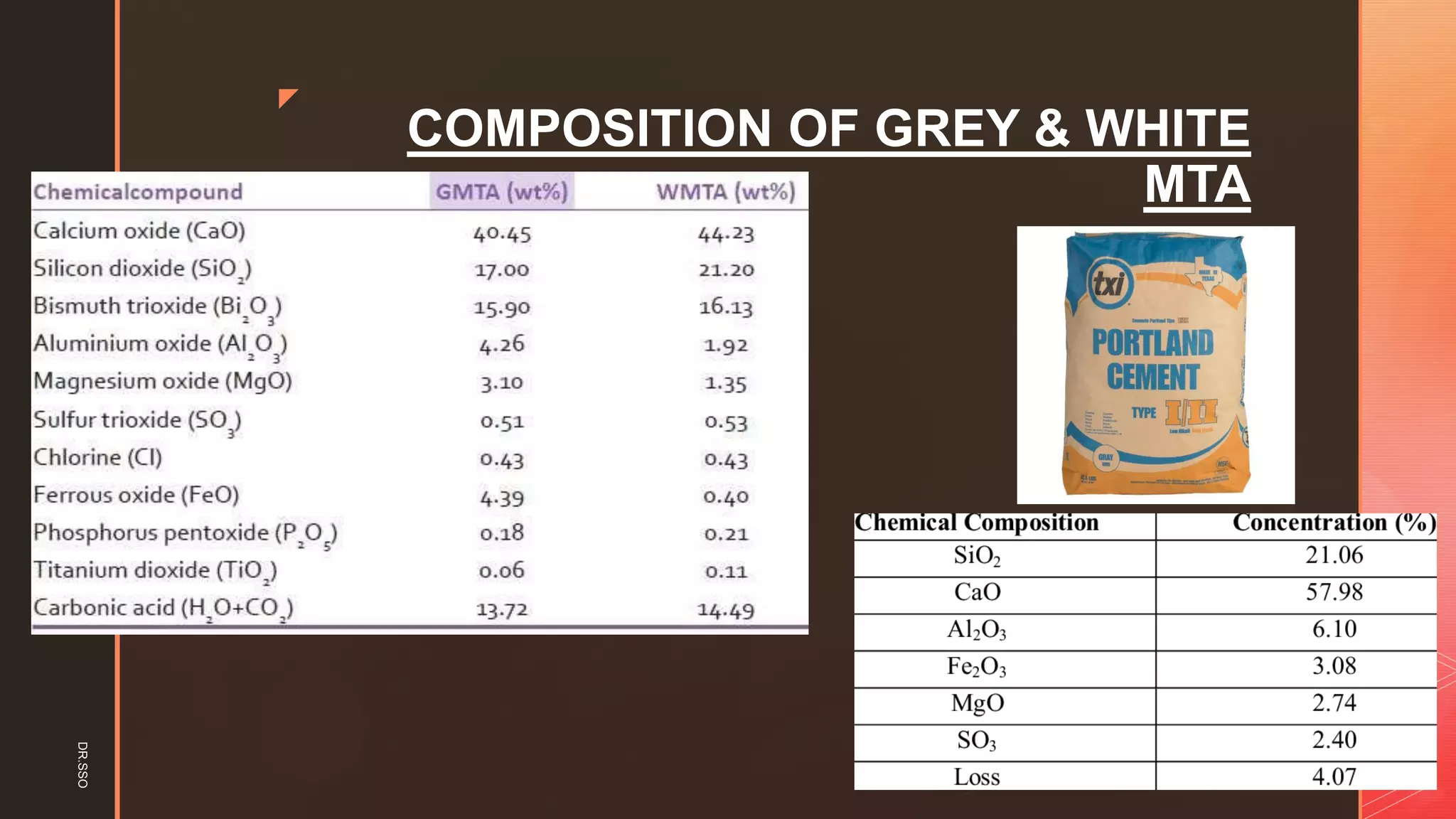
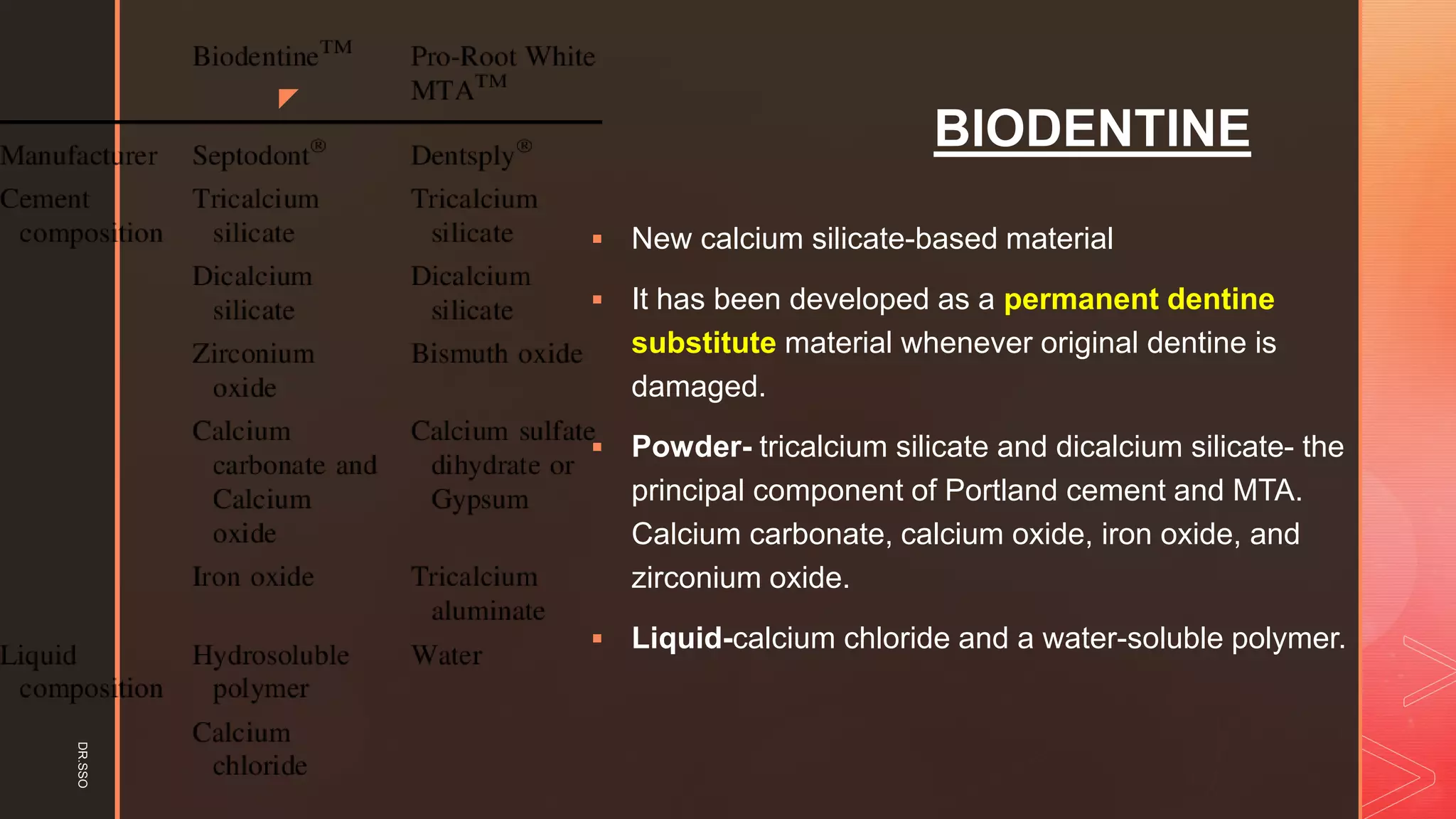
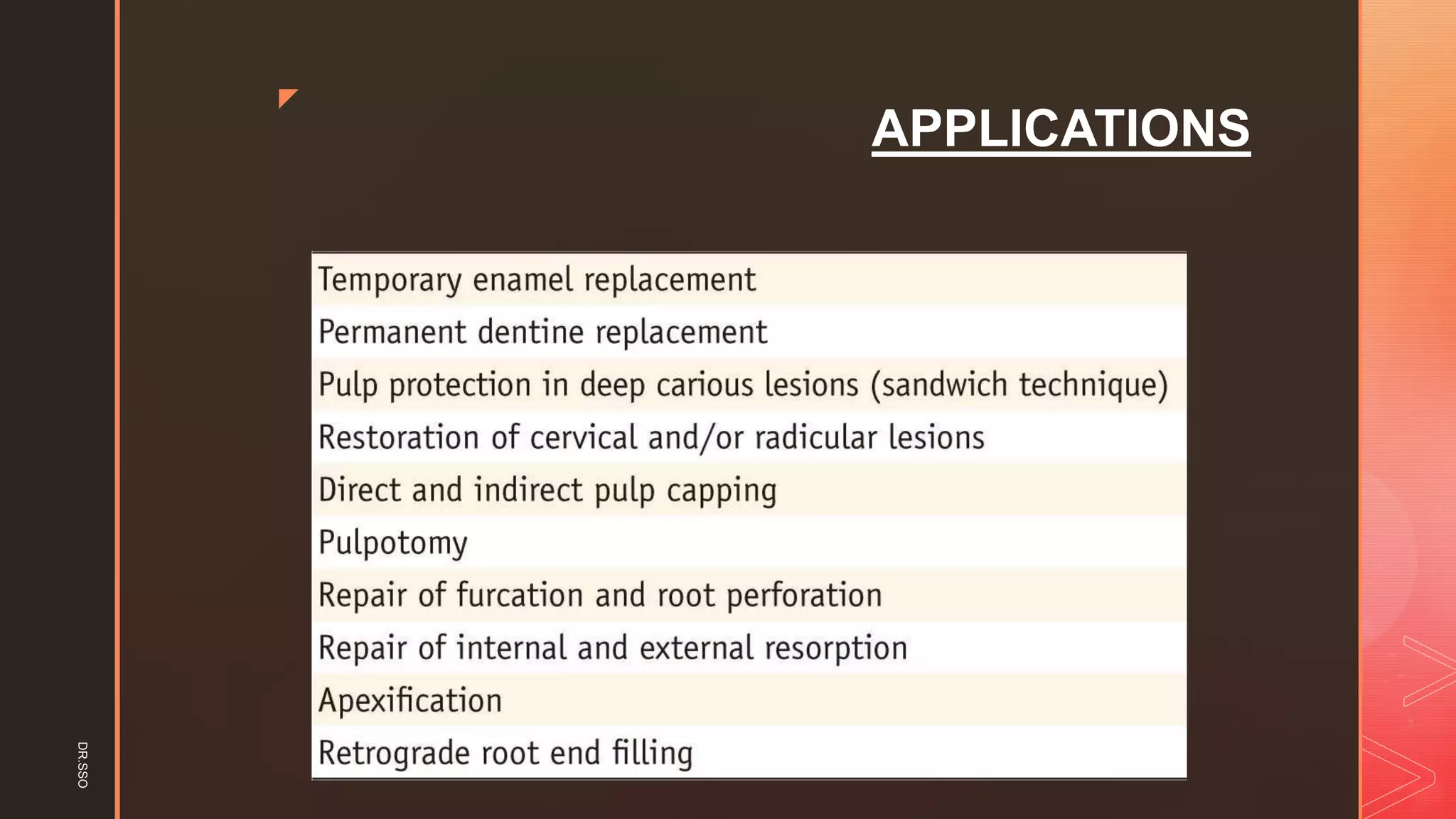
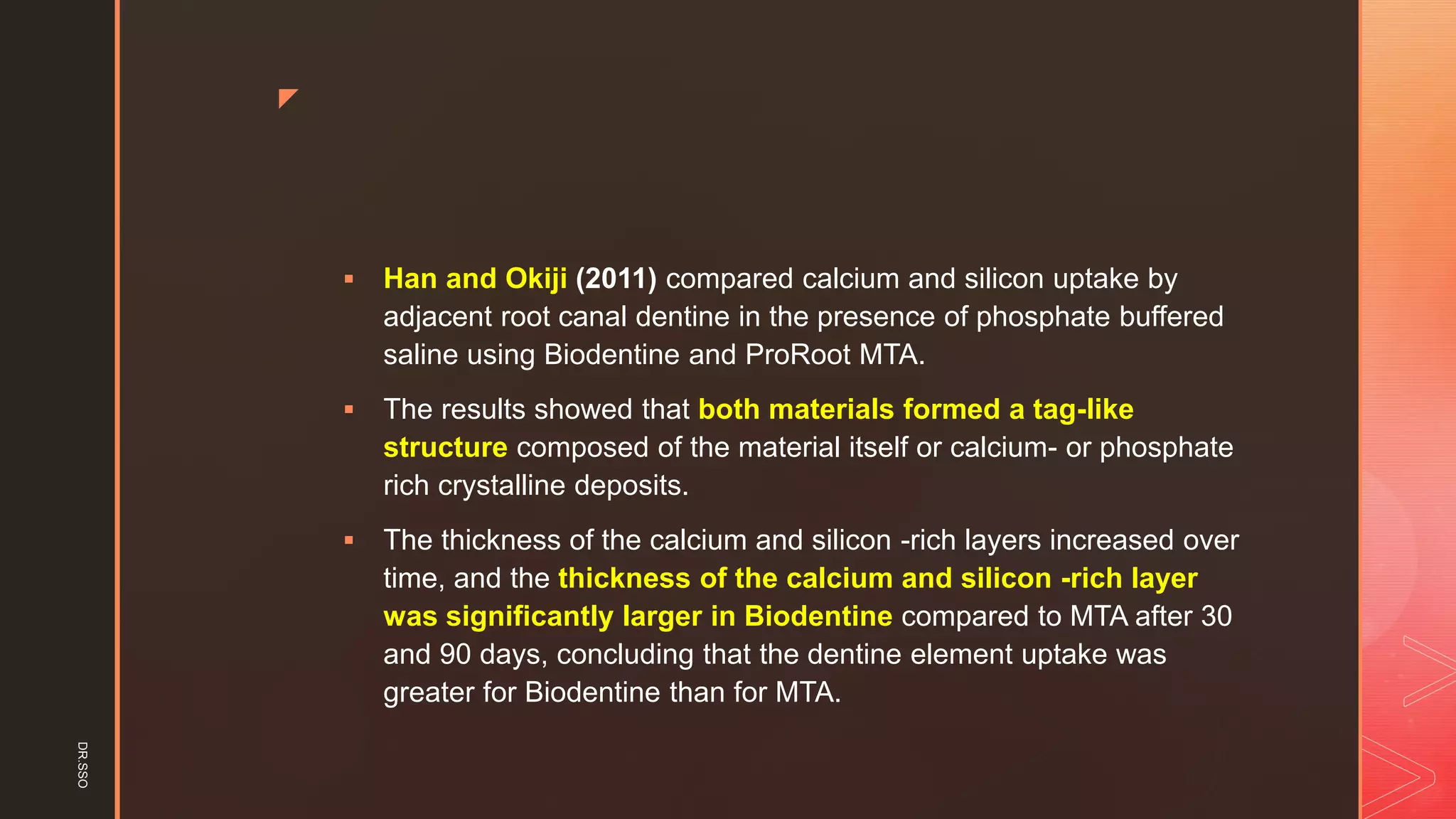
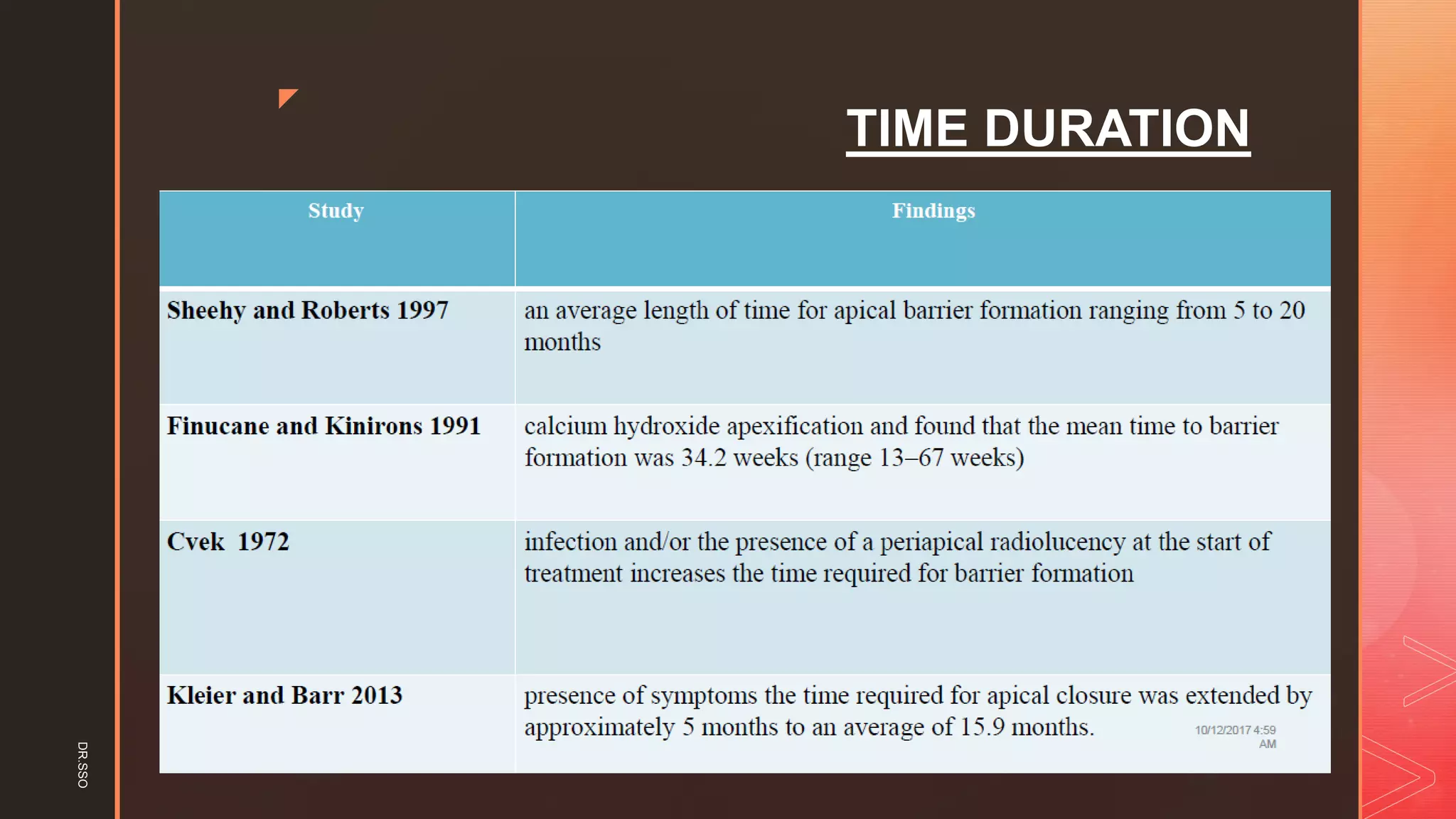
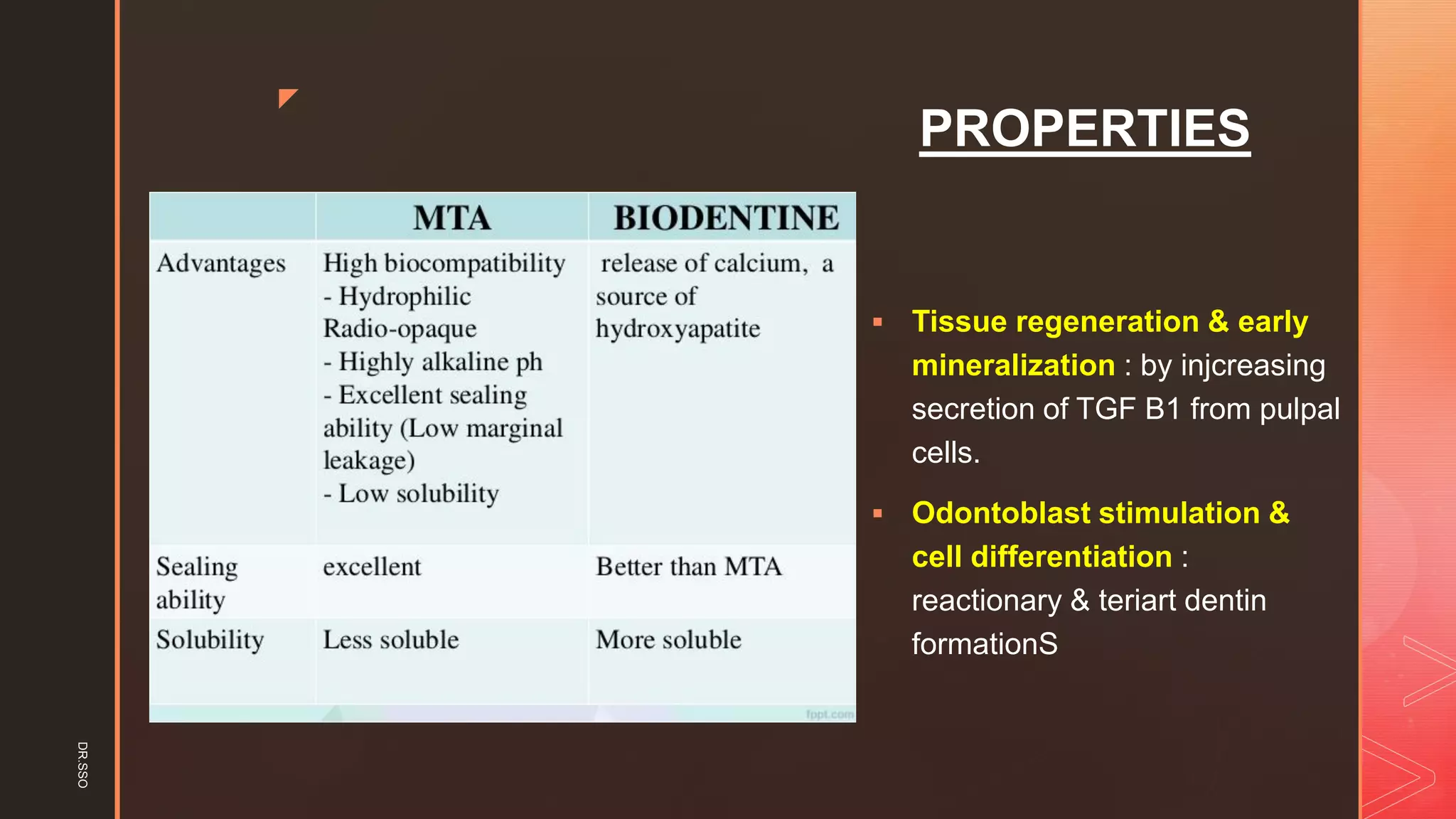
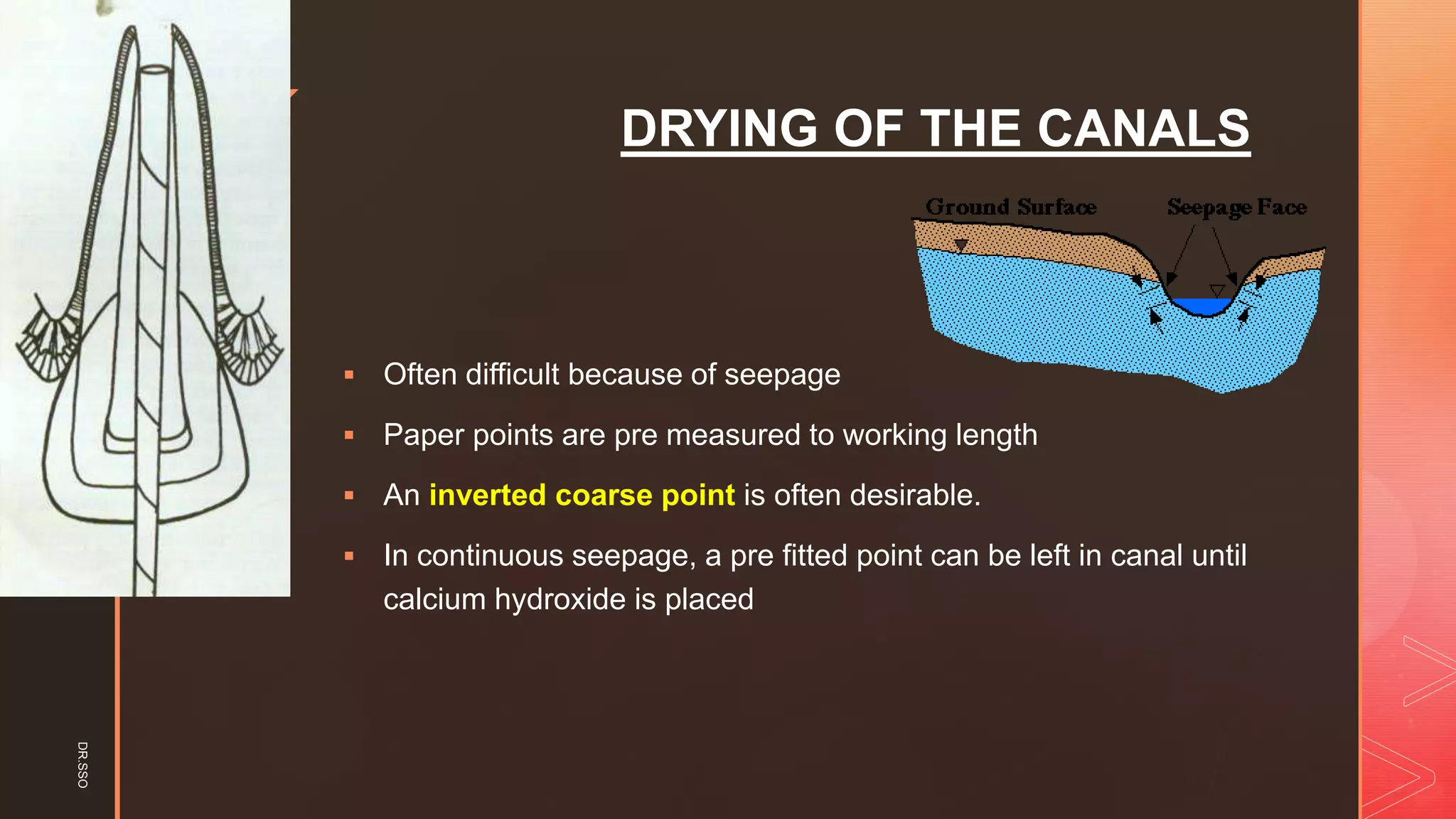
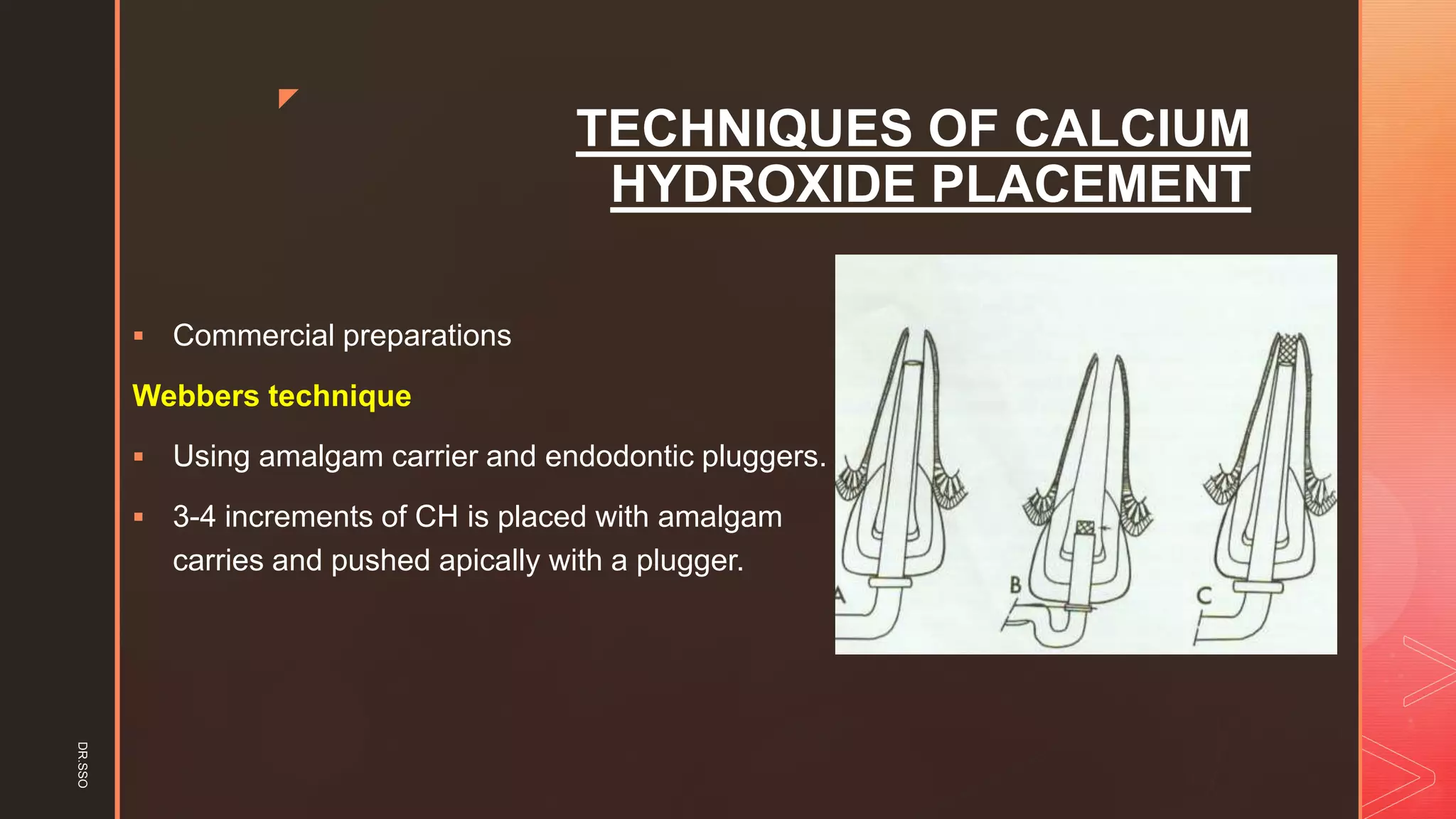
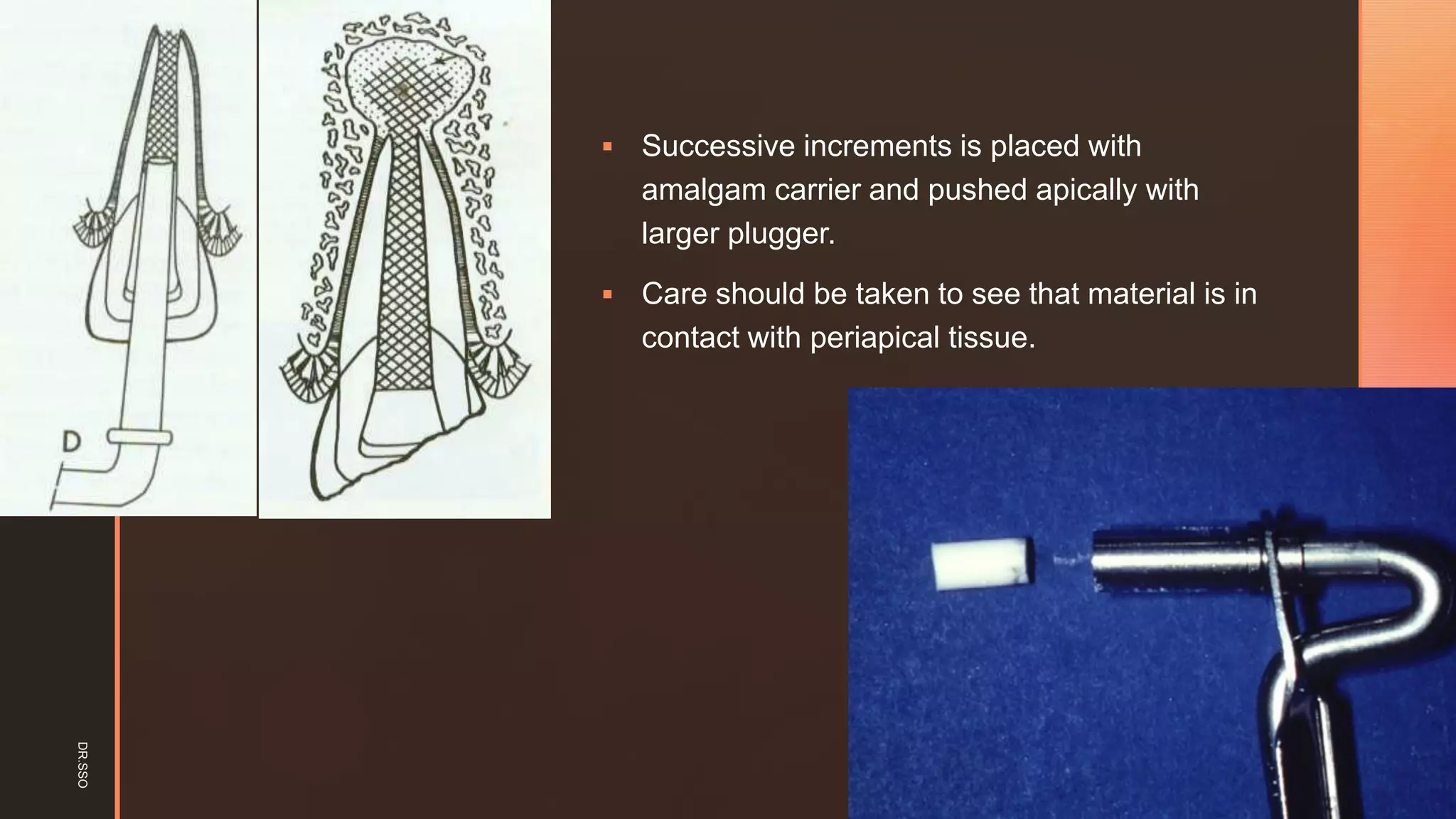
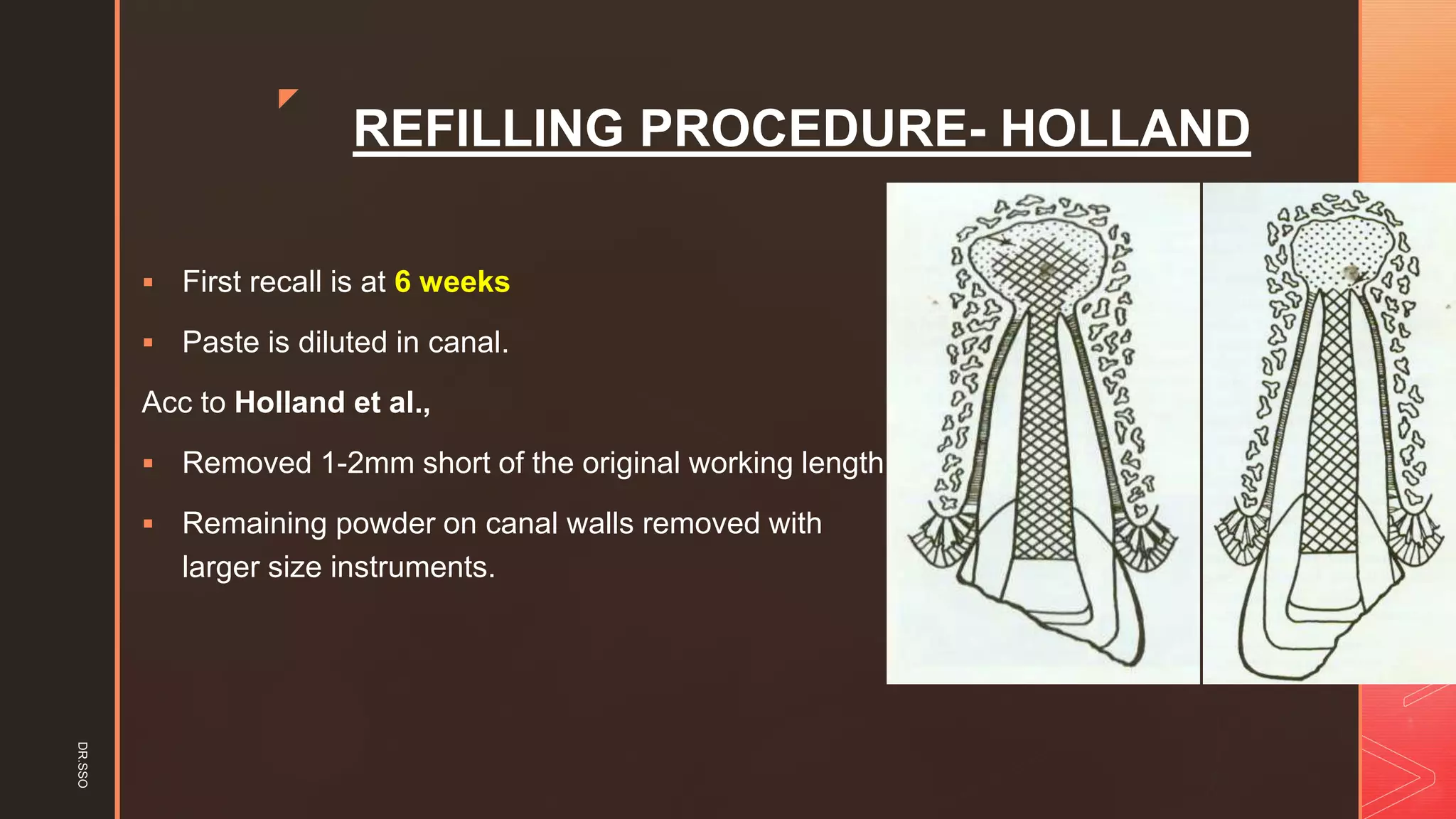
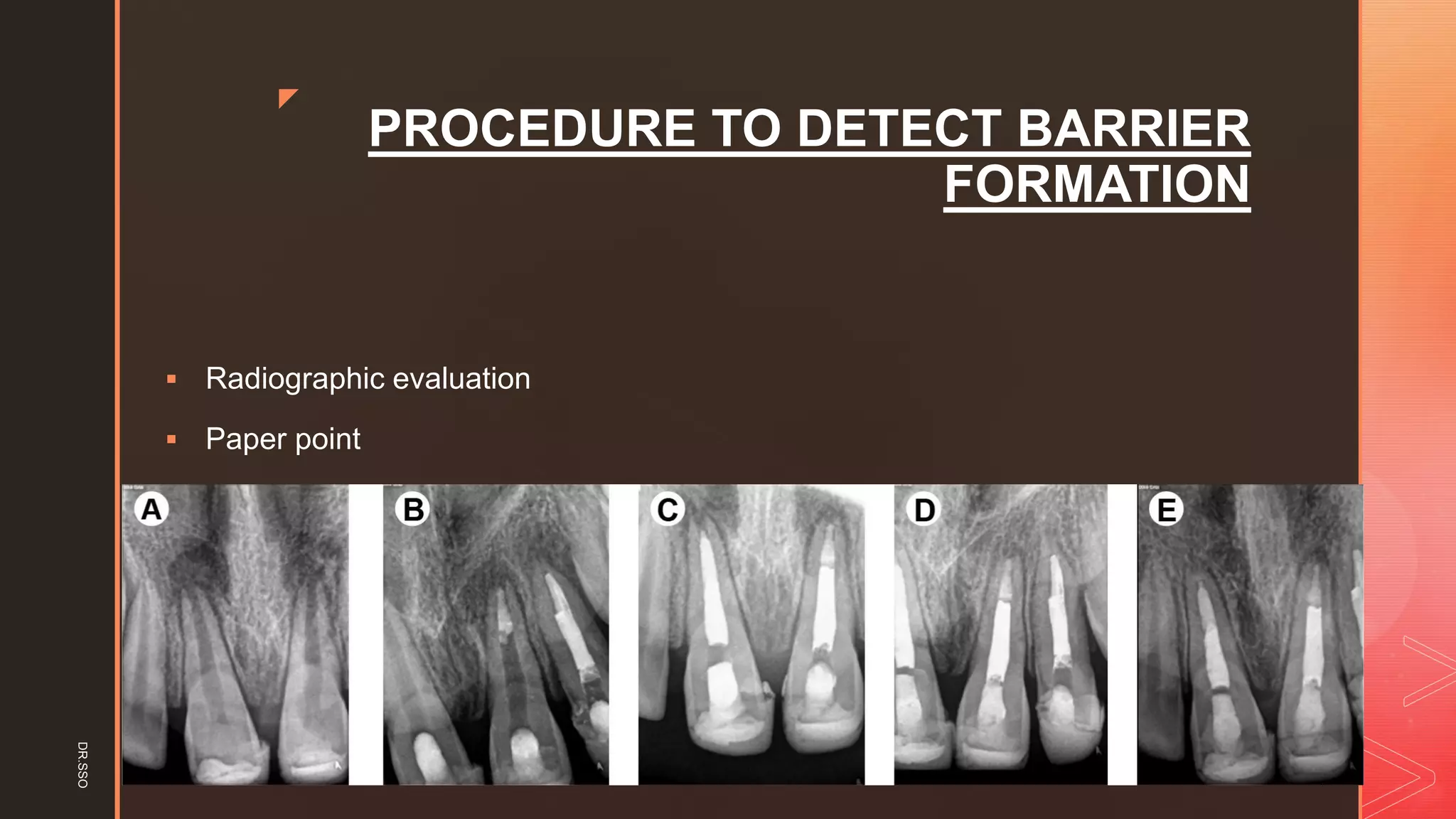
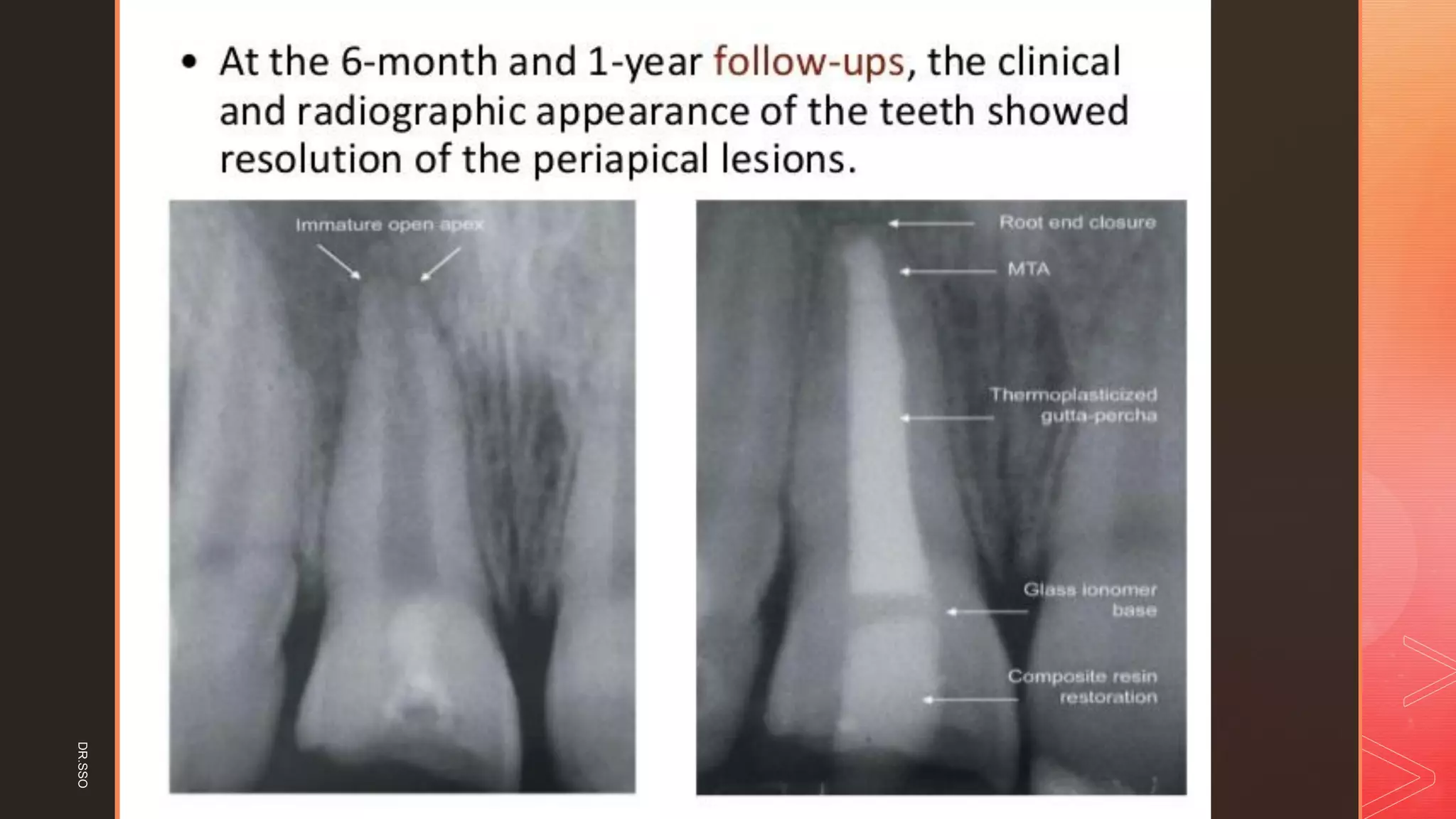
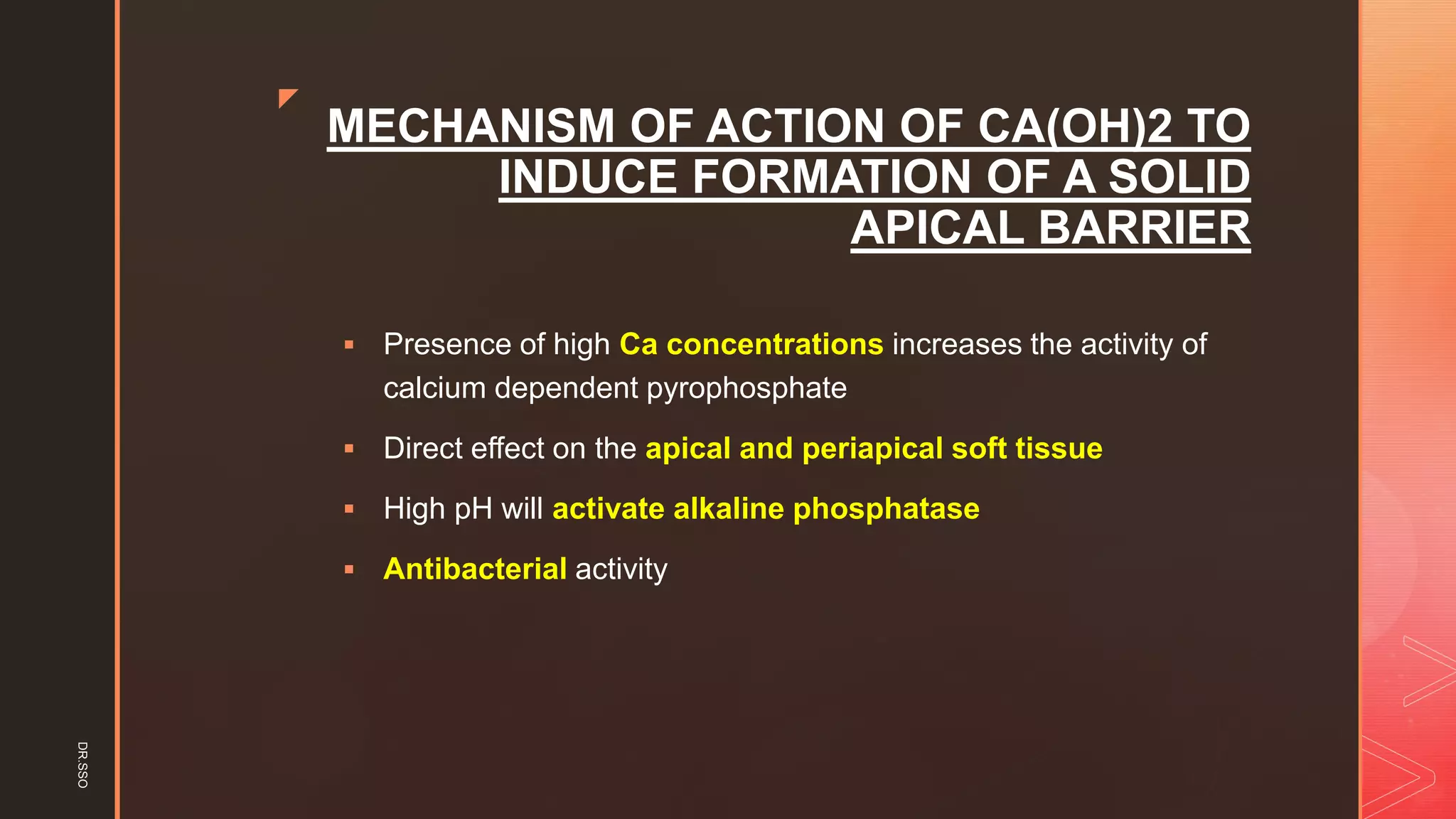
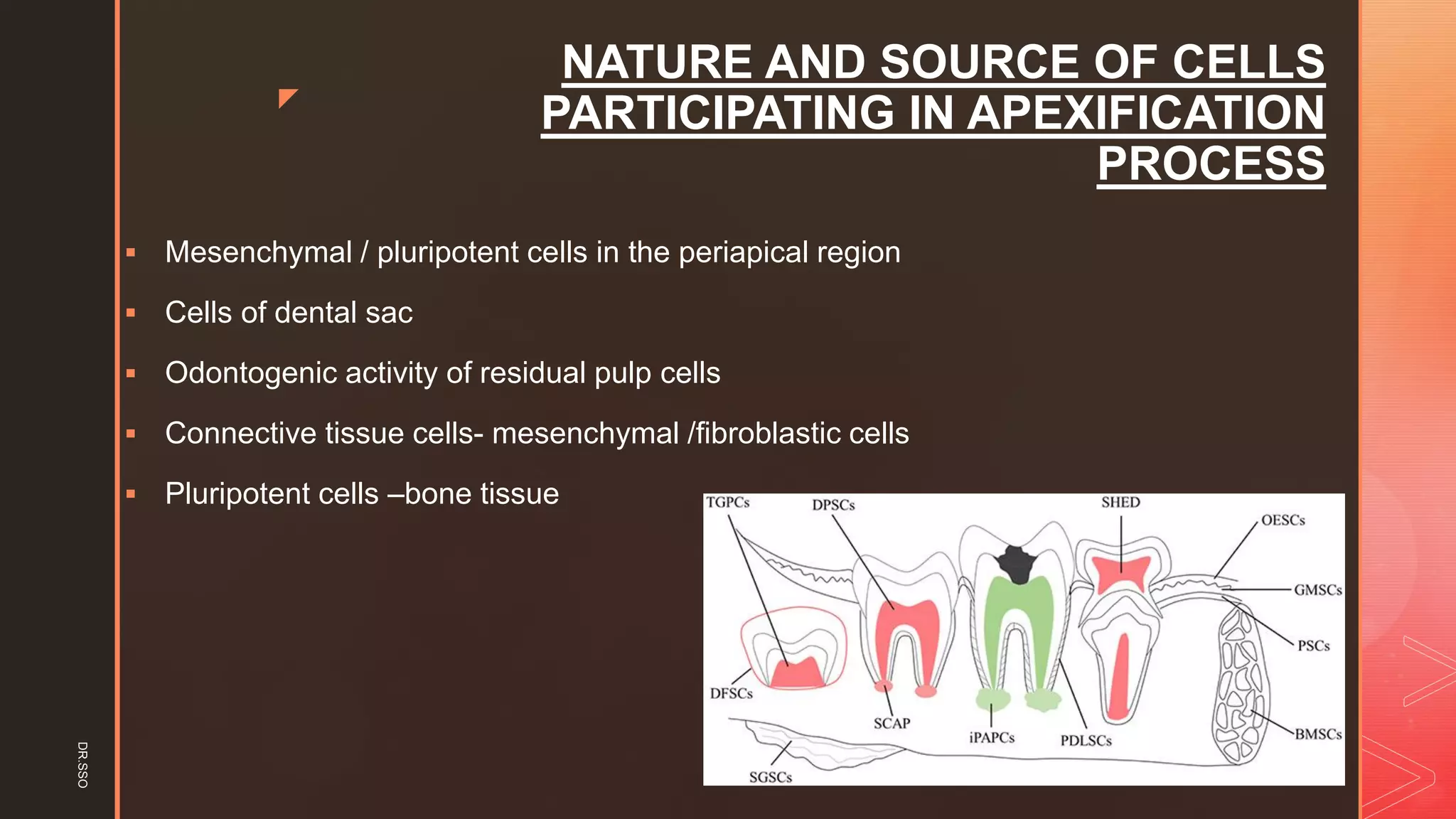
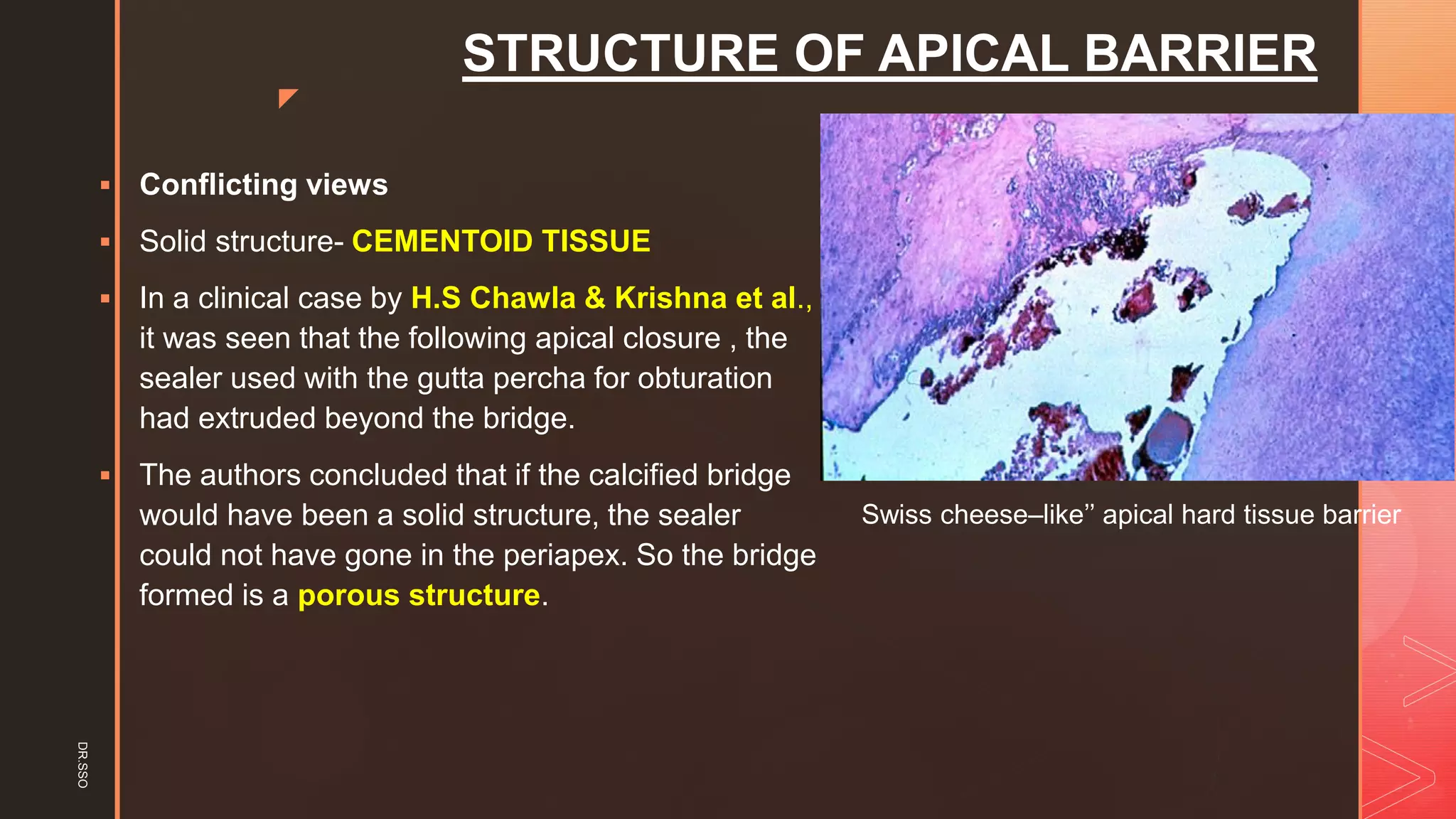
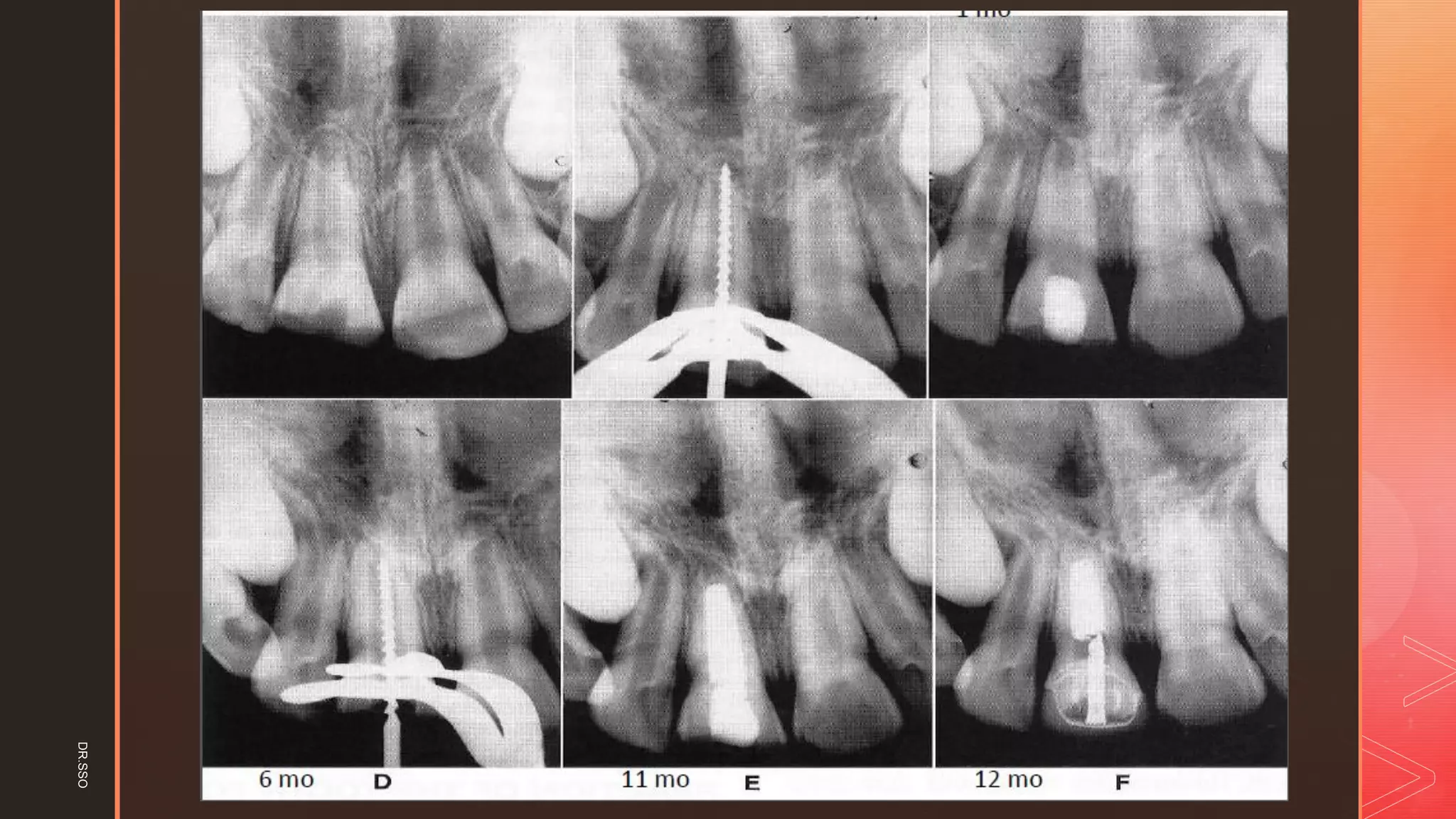
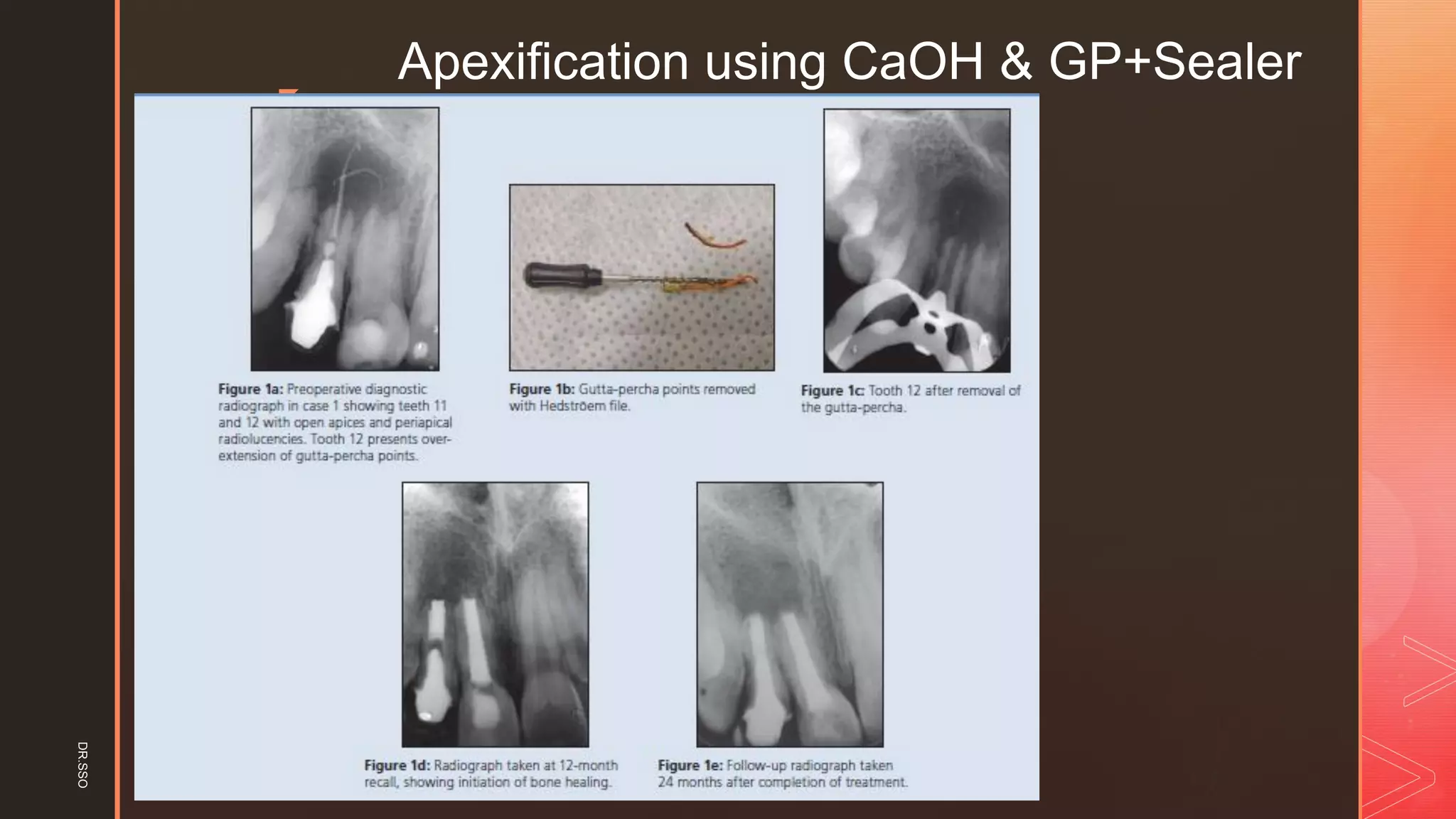
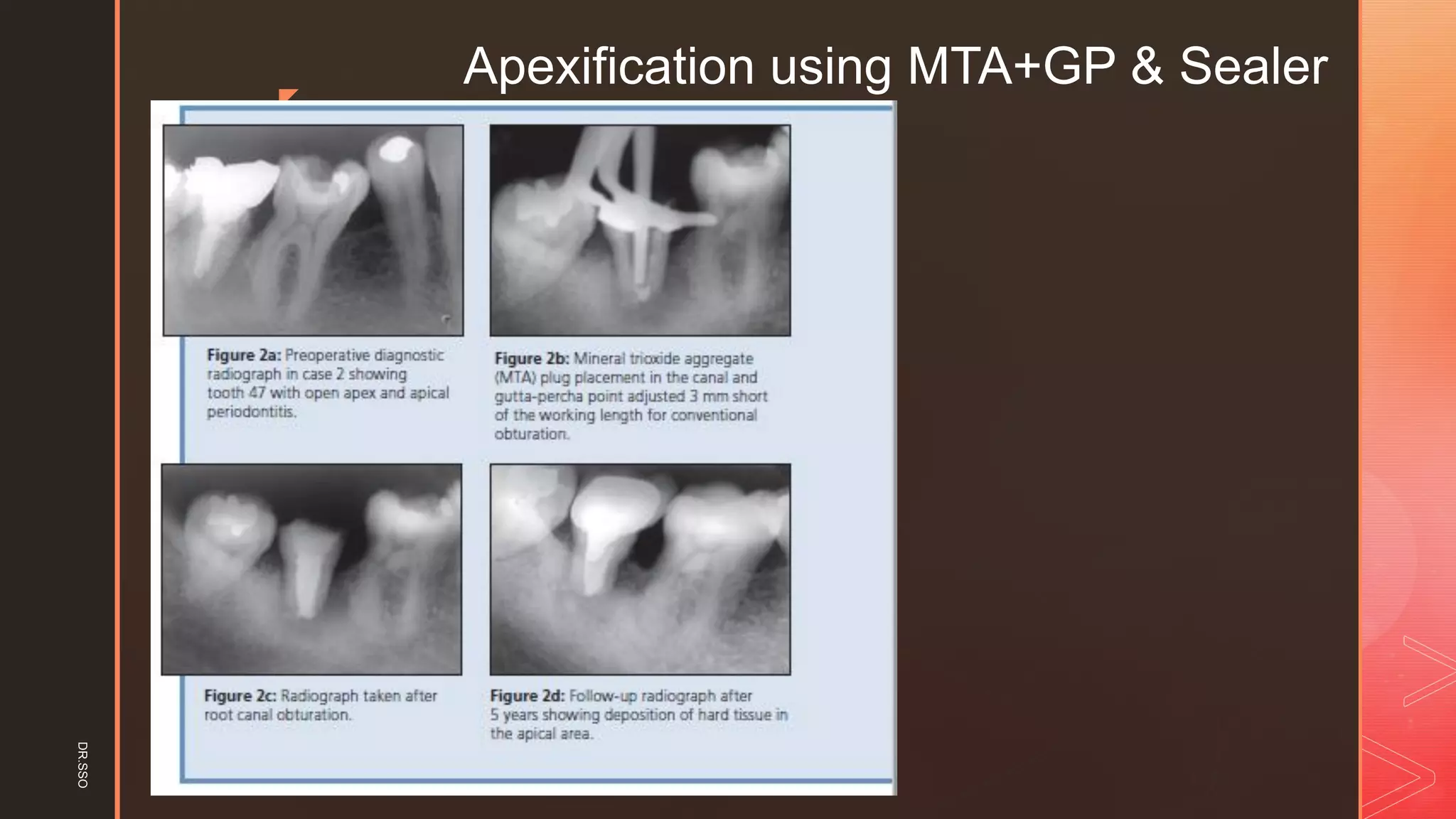
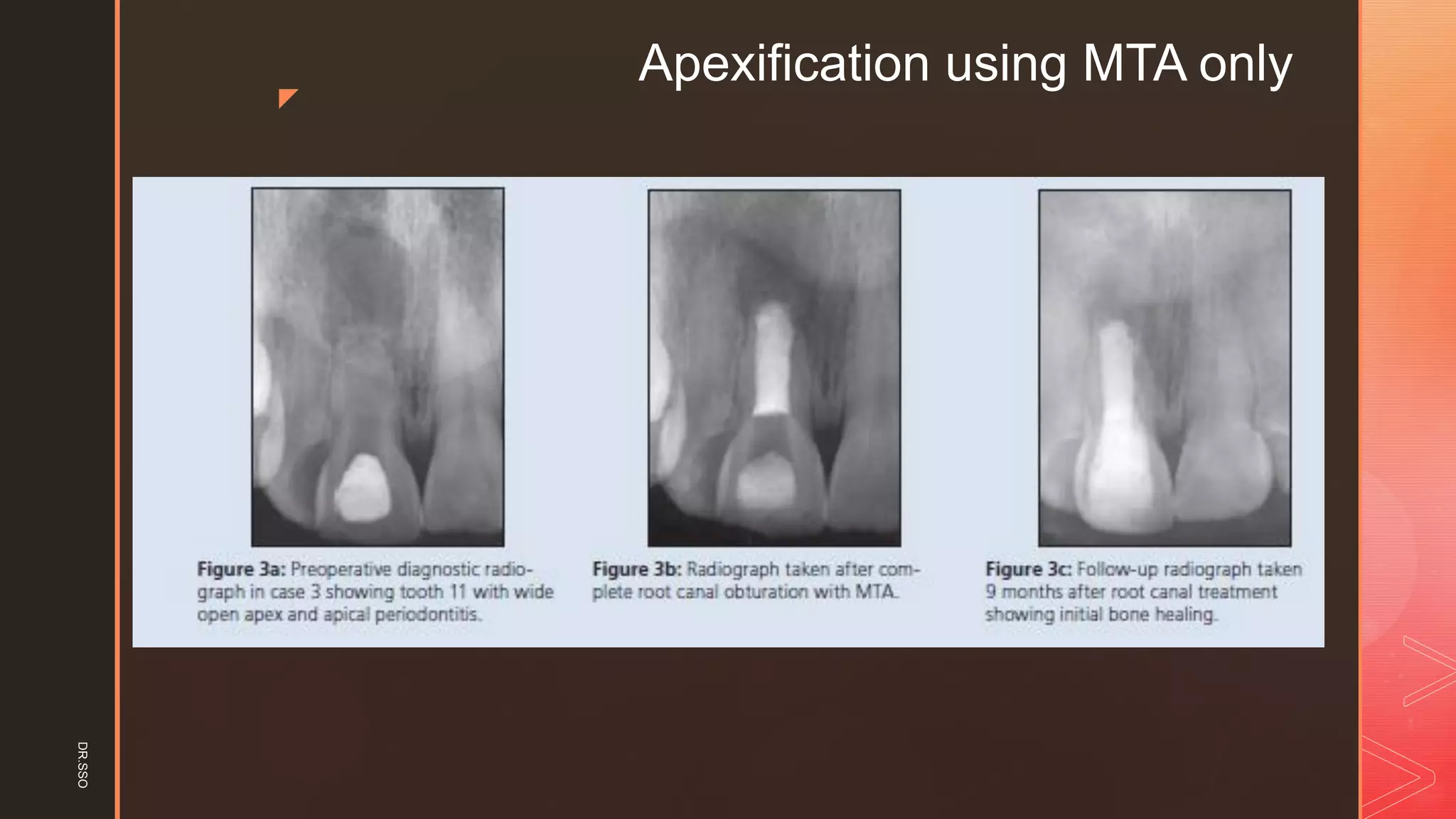
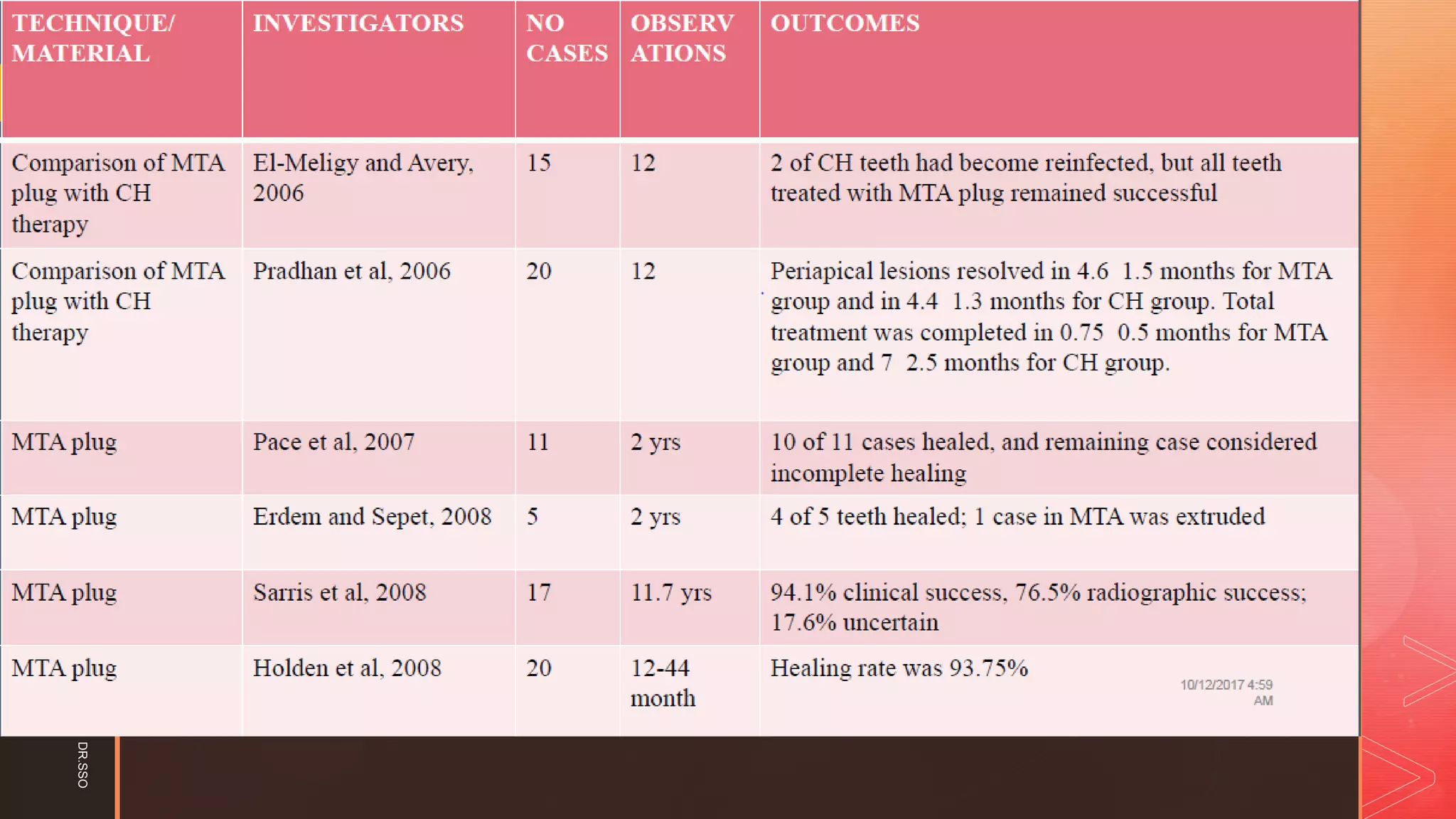
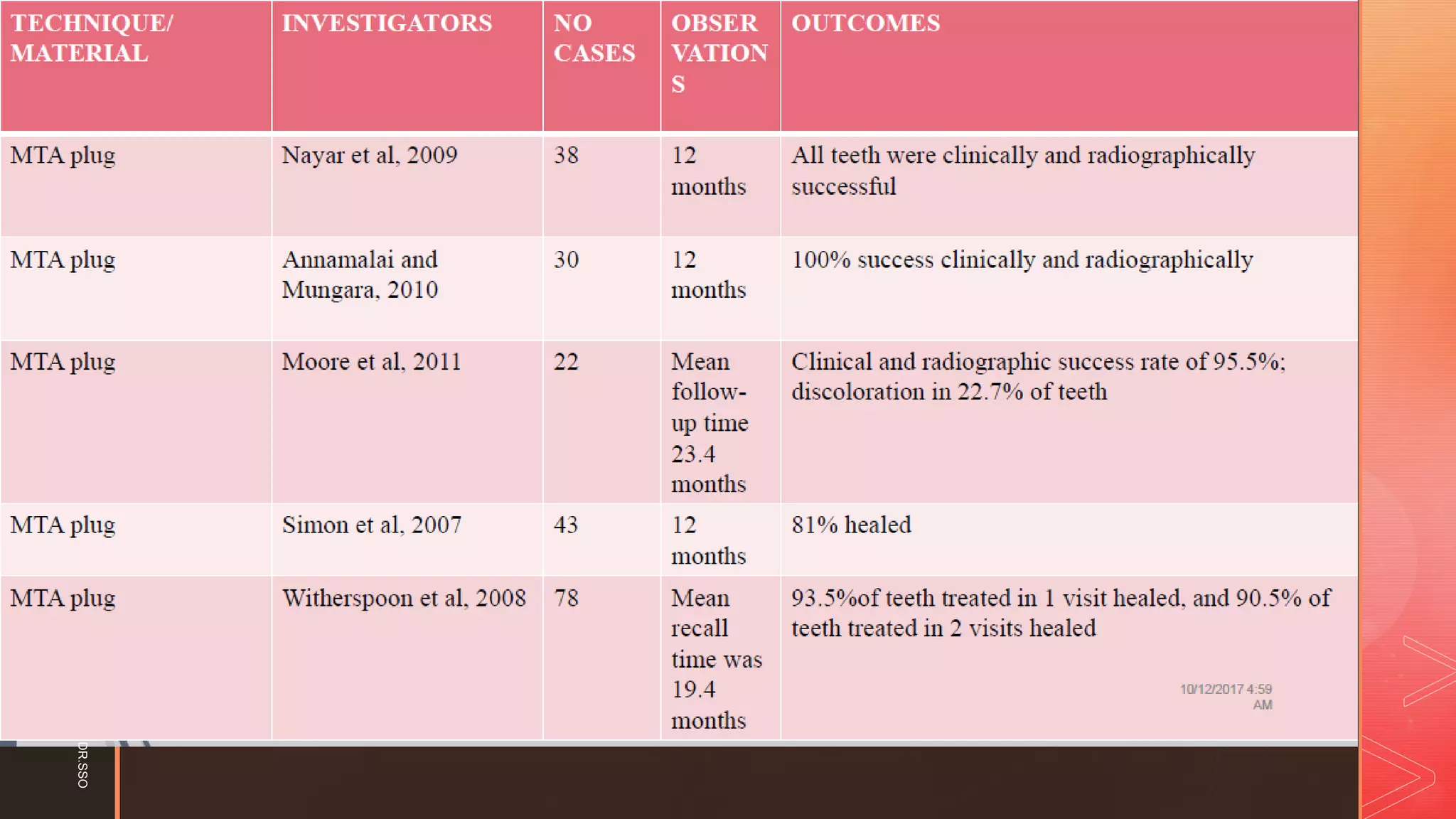
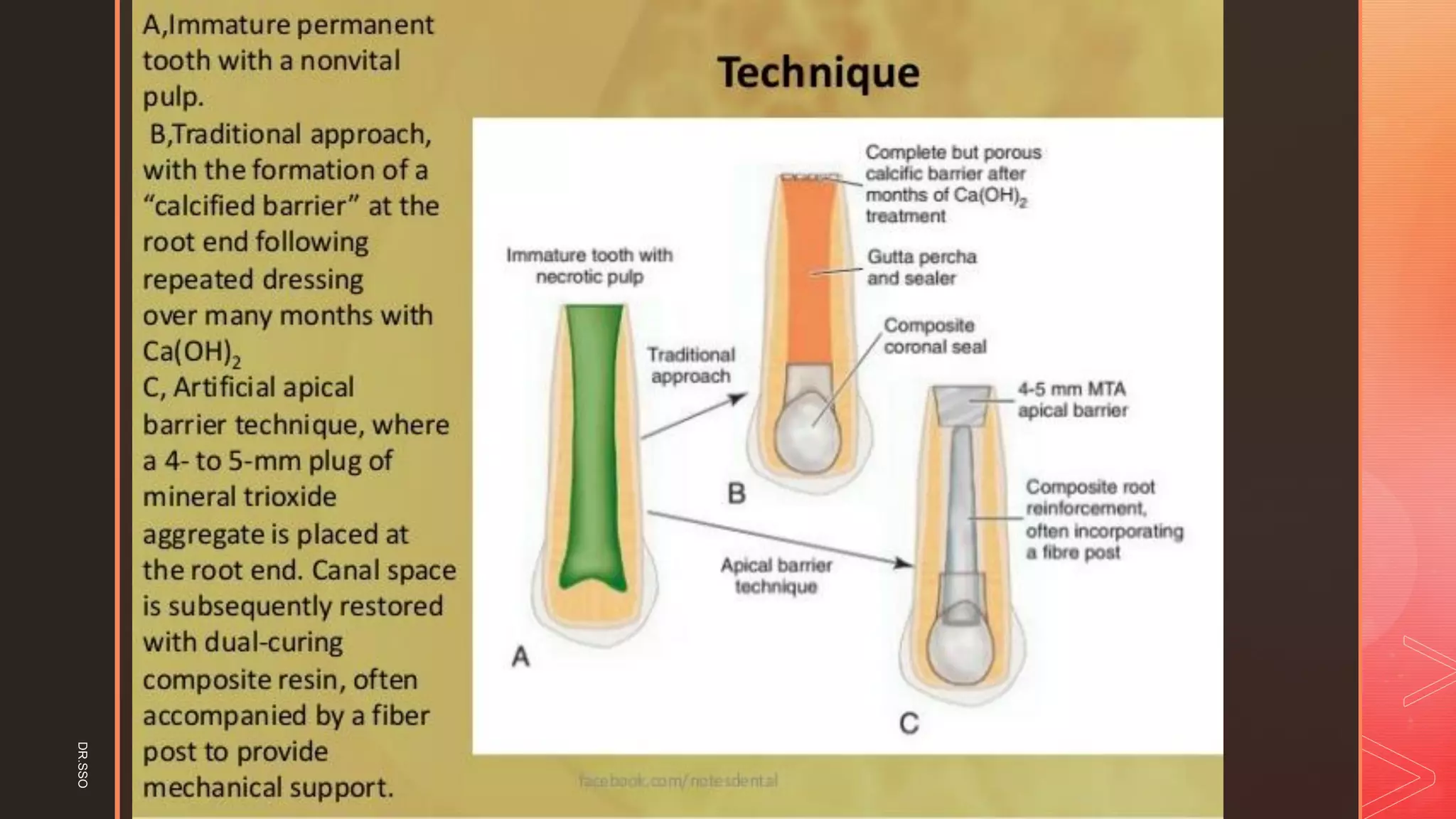
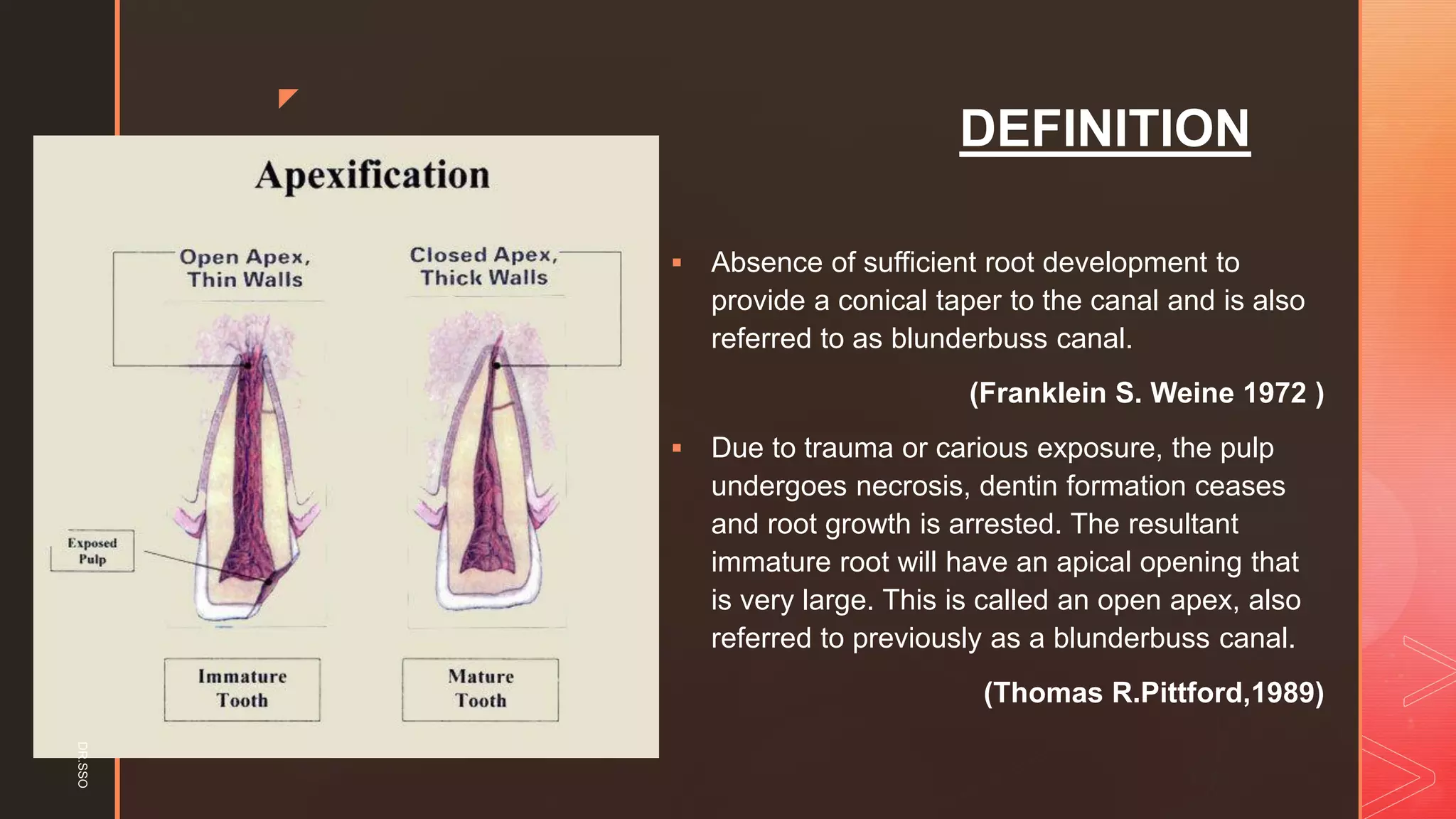
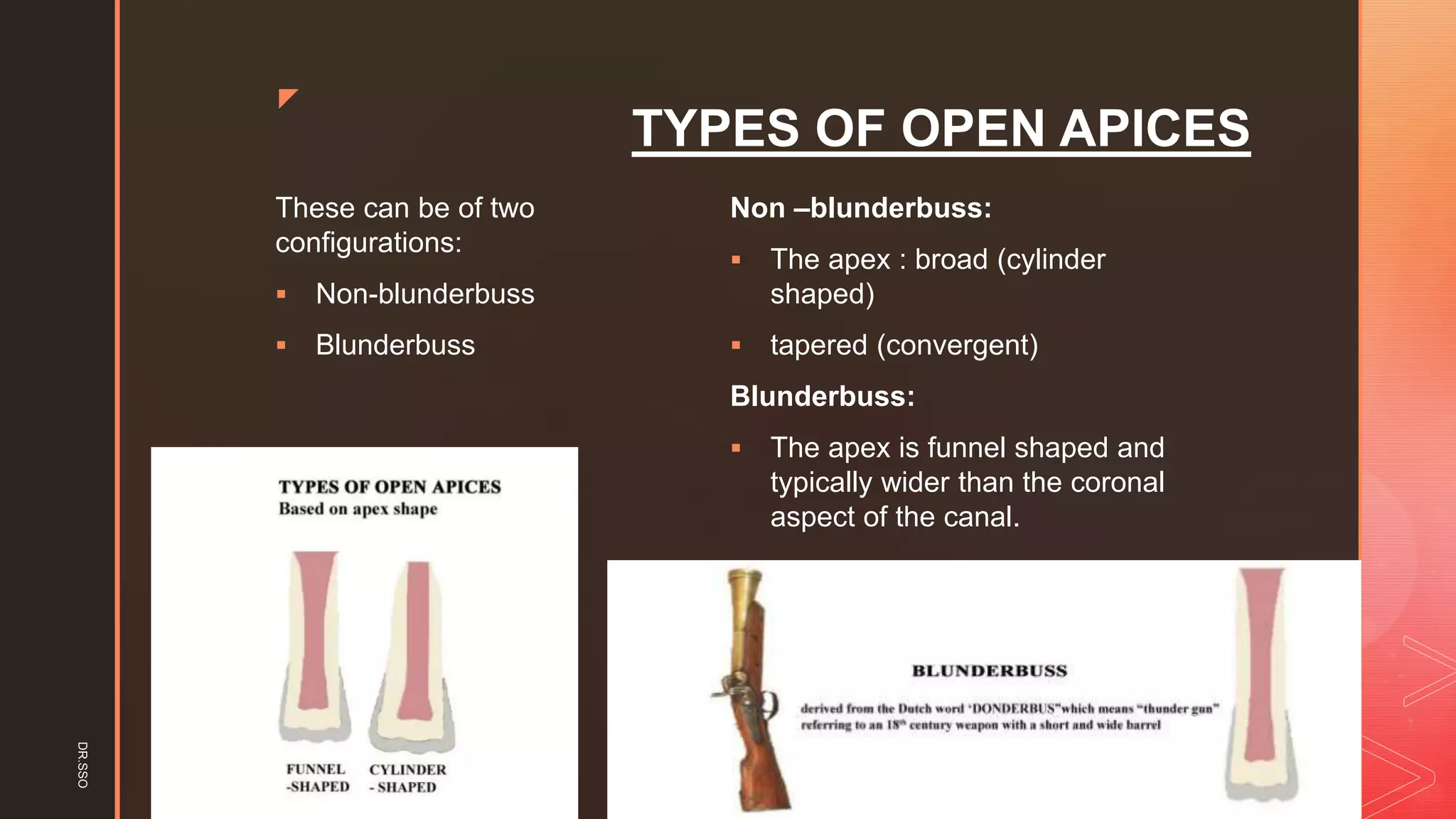
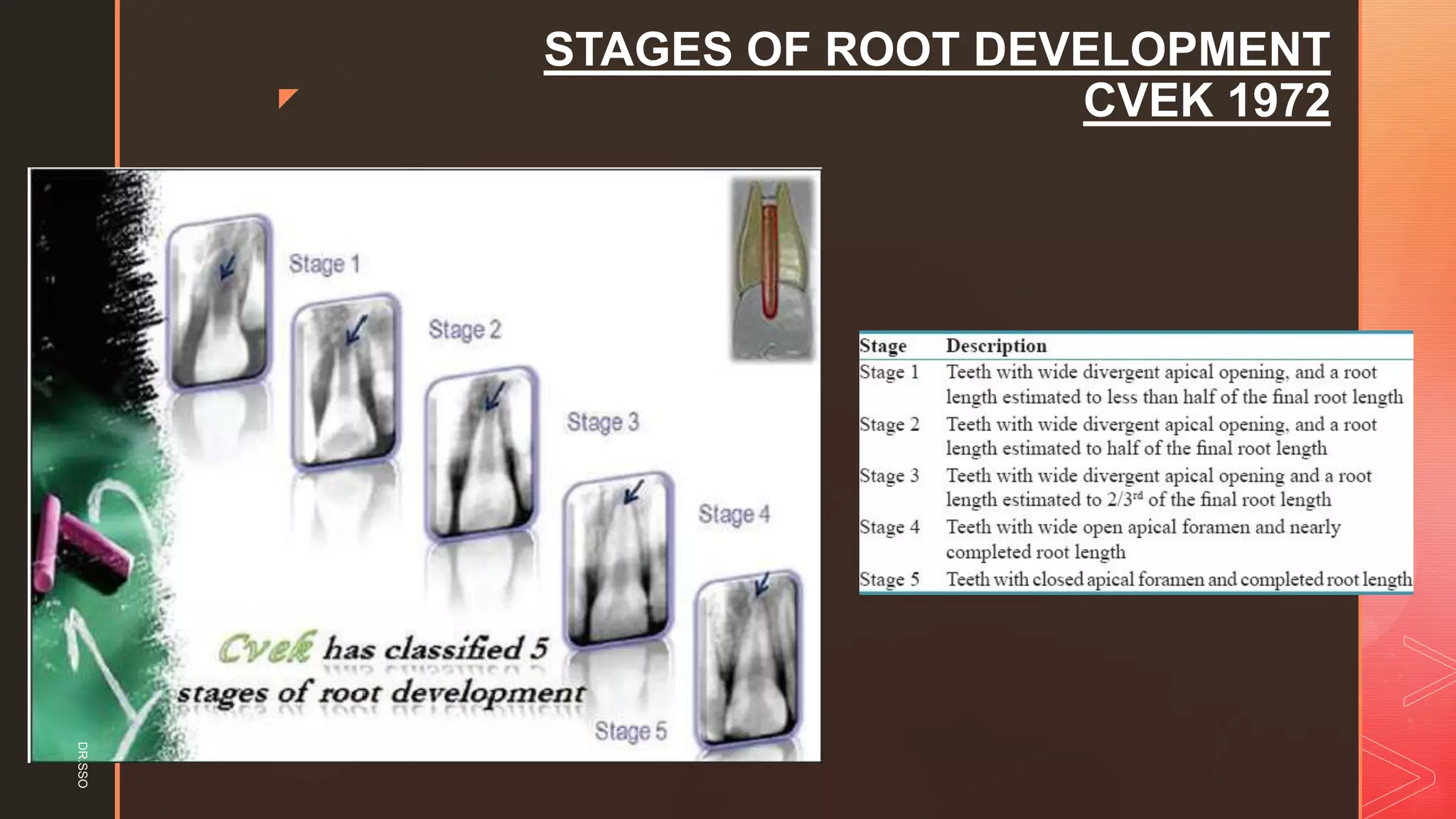
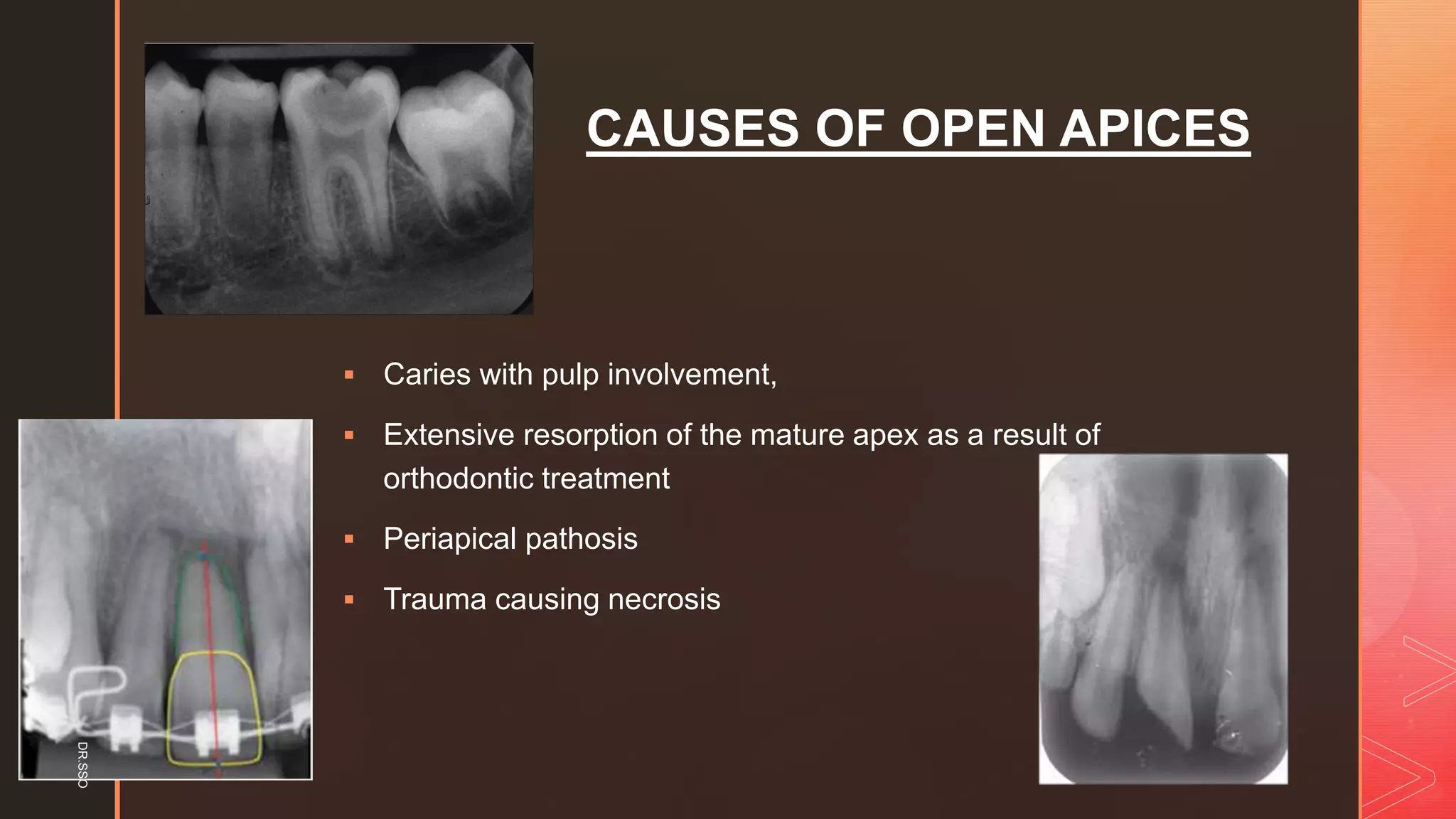
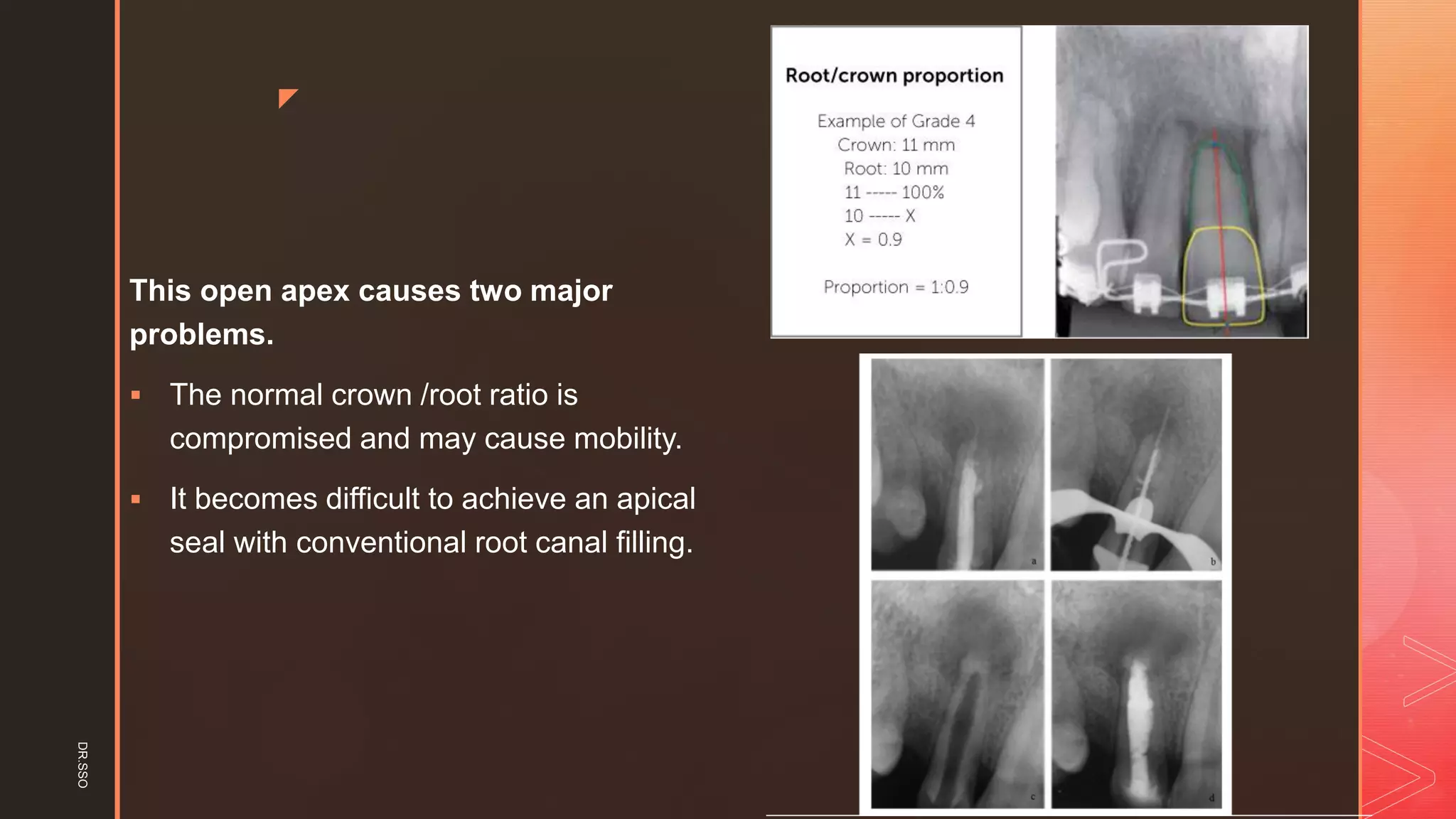
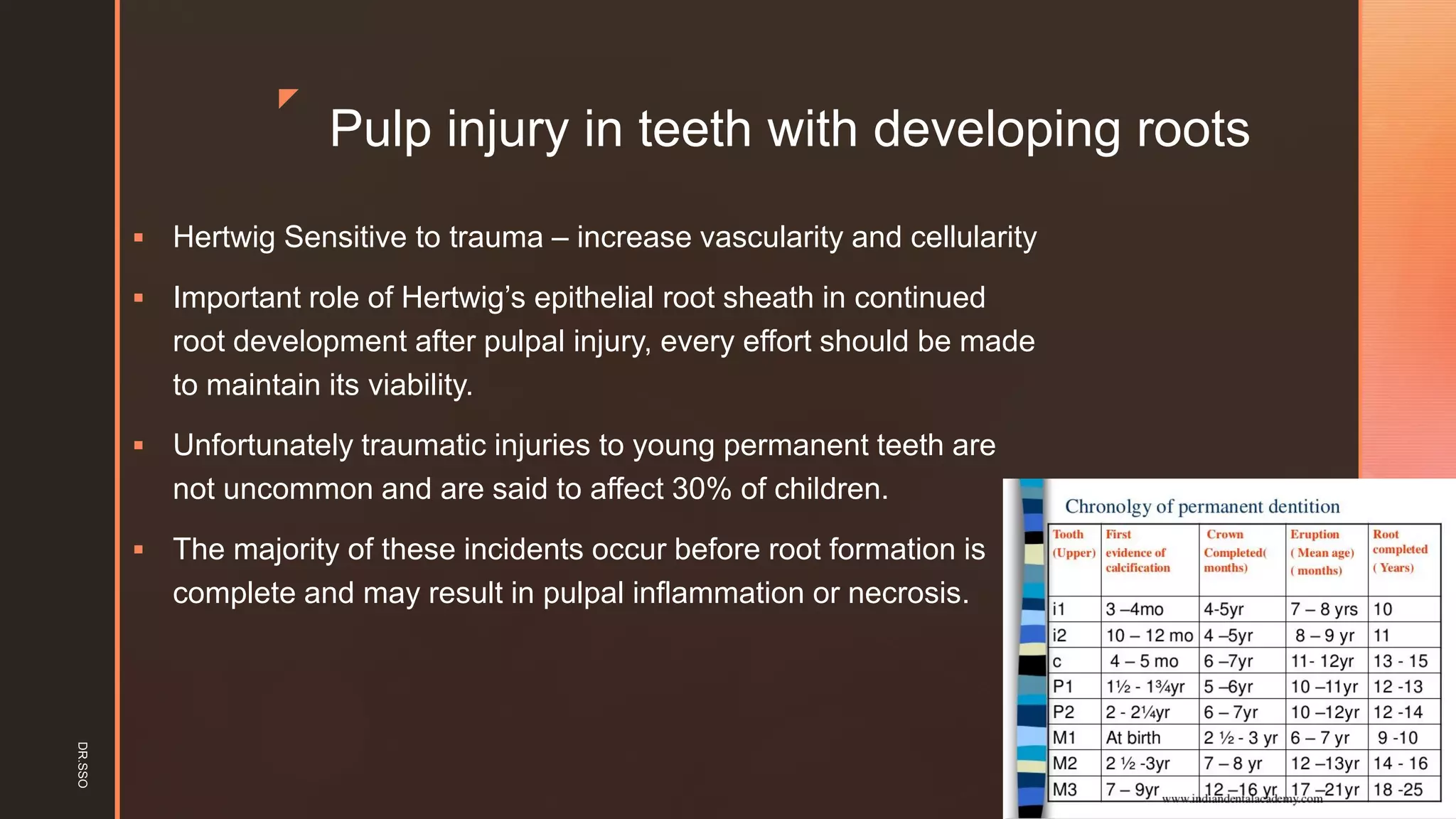
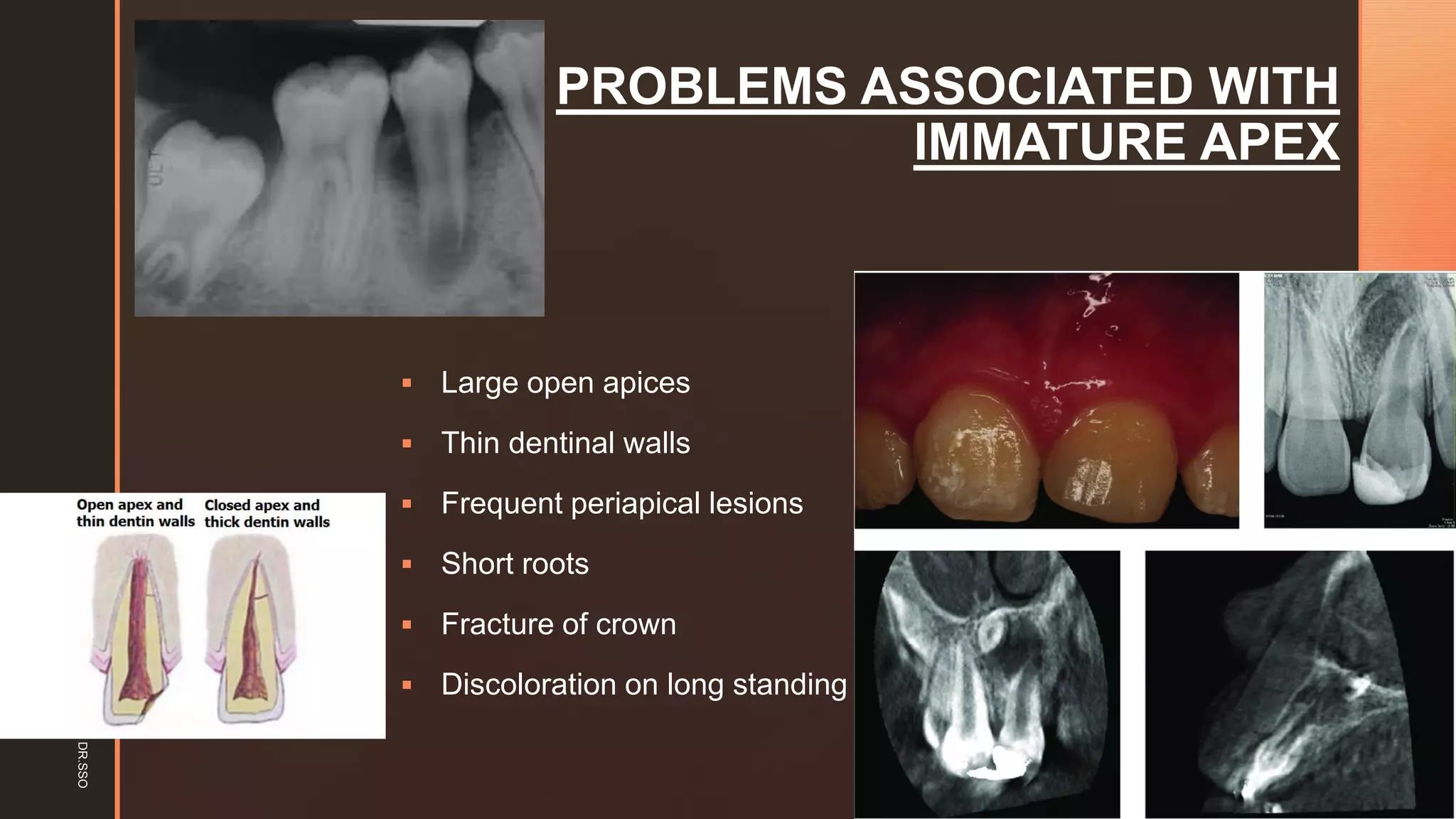
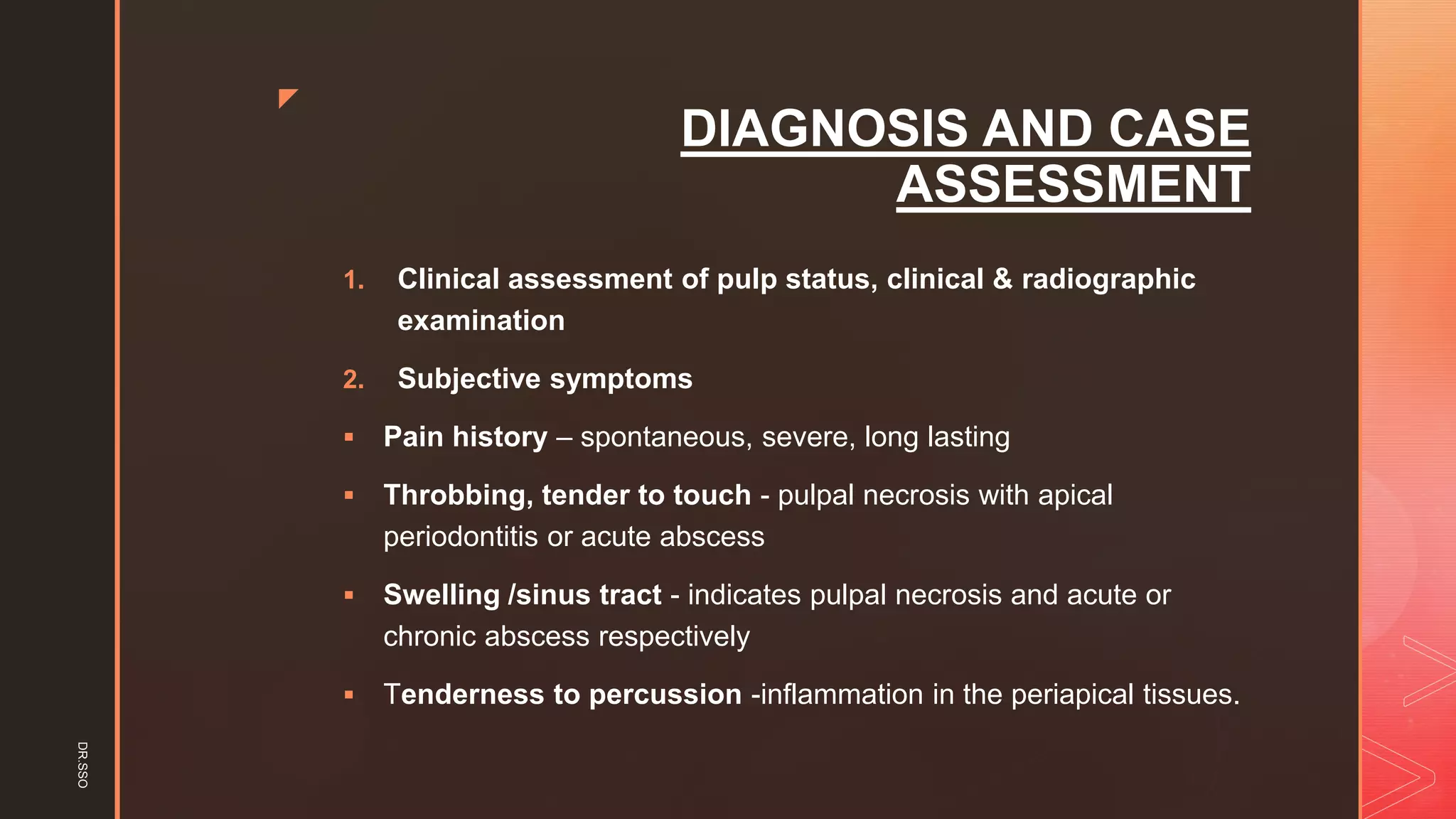
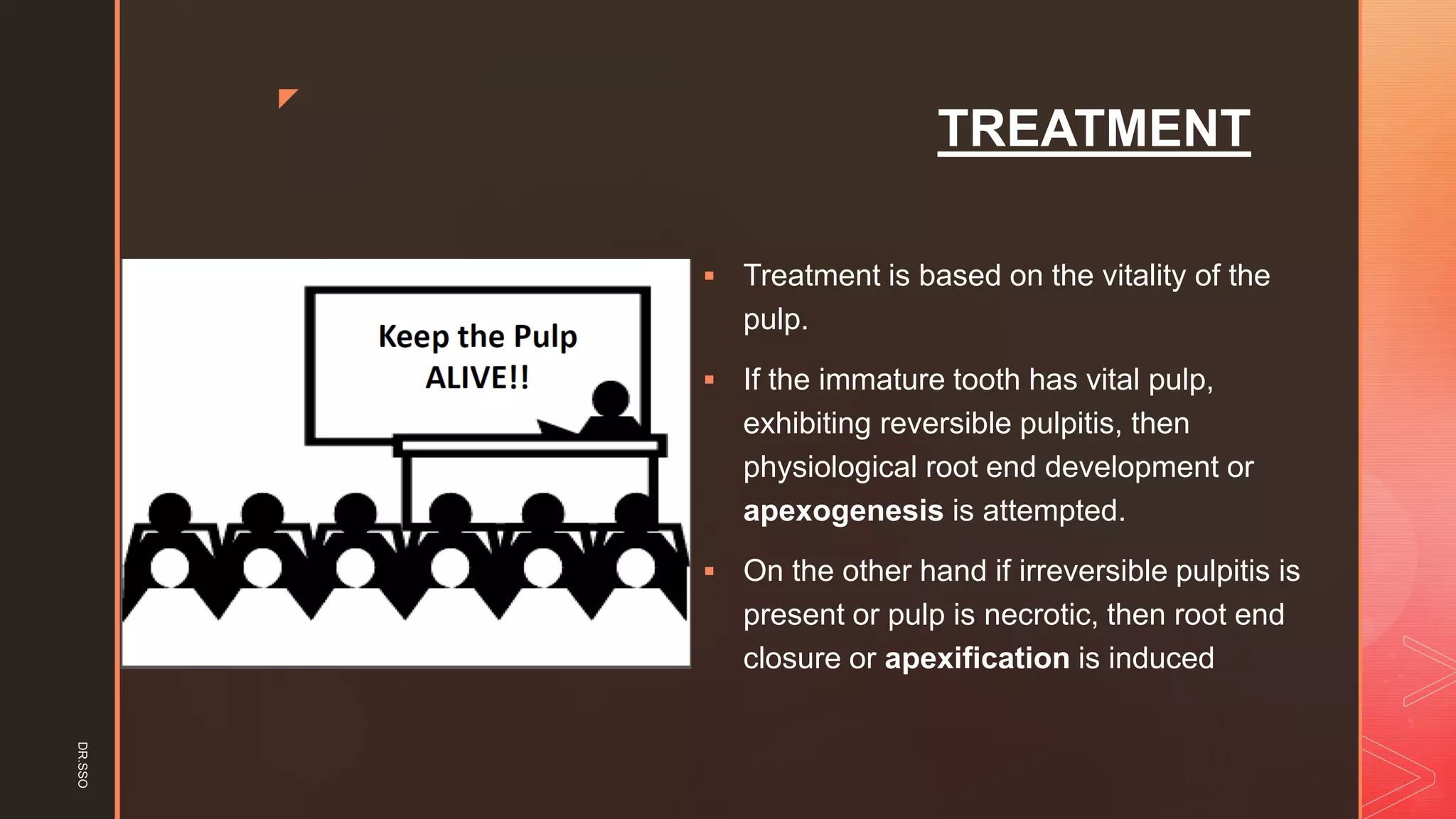
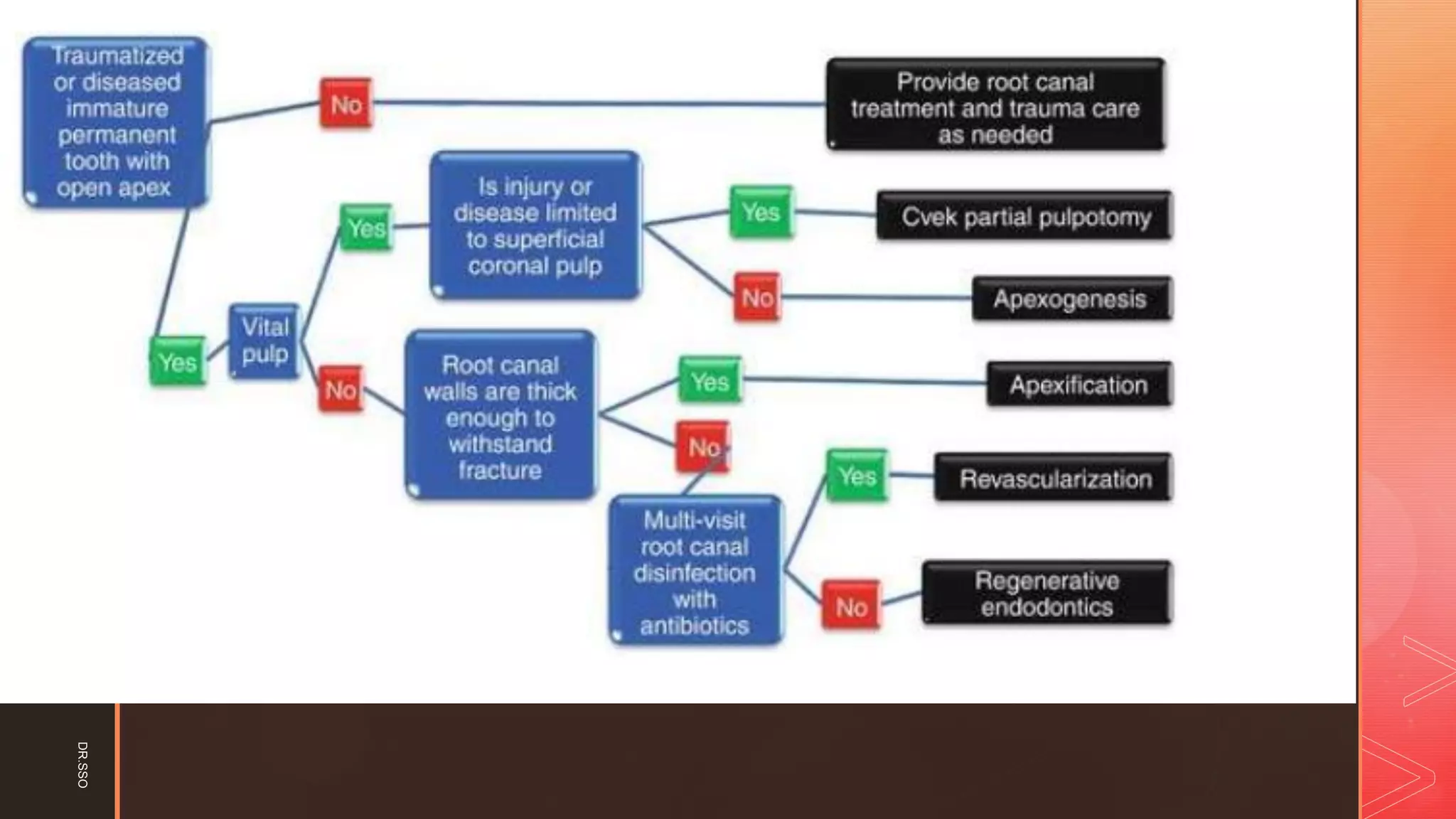
This document discusses open apex and apexification treatment. It defines open apex as an immature root with incomplete development and a large apical opening. Treatment depends on pulp vitality - apexogenesis aims to encourage continued root development if the pulp is vital, while apexification induces apical closure if the pulp is necrotic. The document outlines the stages of root development, causes of open apex, complications, diagnosis, and various treatment options and materials used for apexogenesis and apexification such as calcium hydroxide, MTA, and Biodentine.
![z
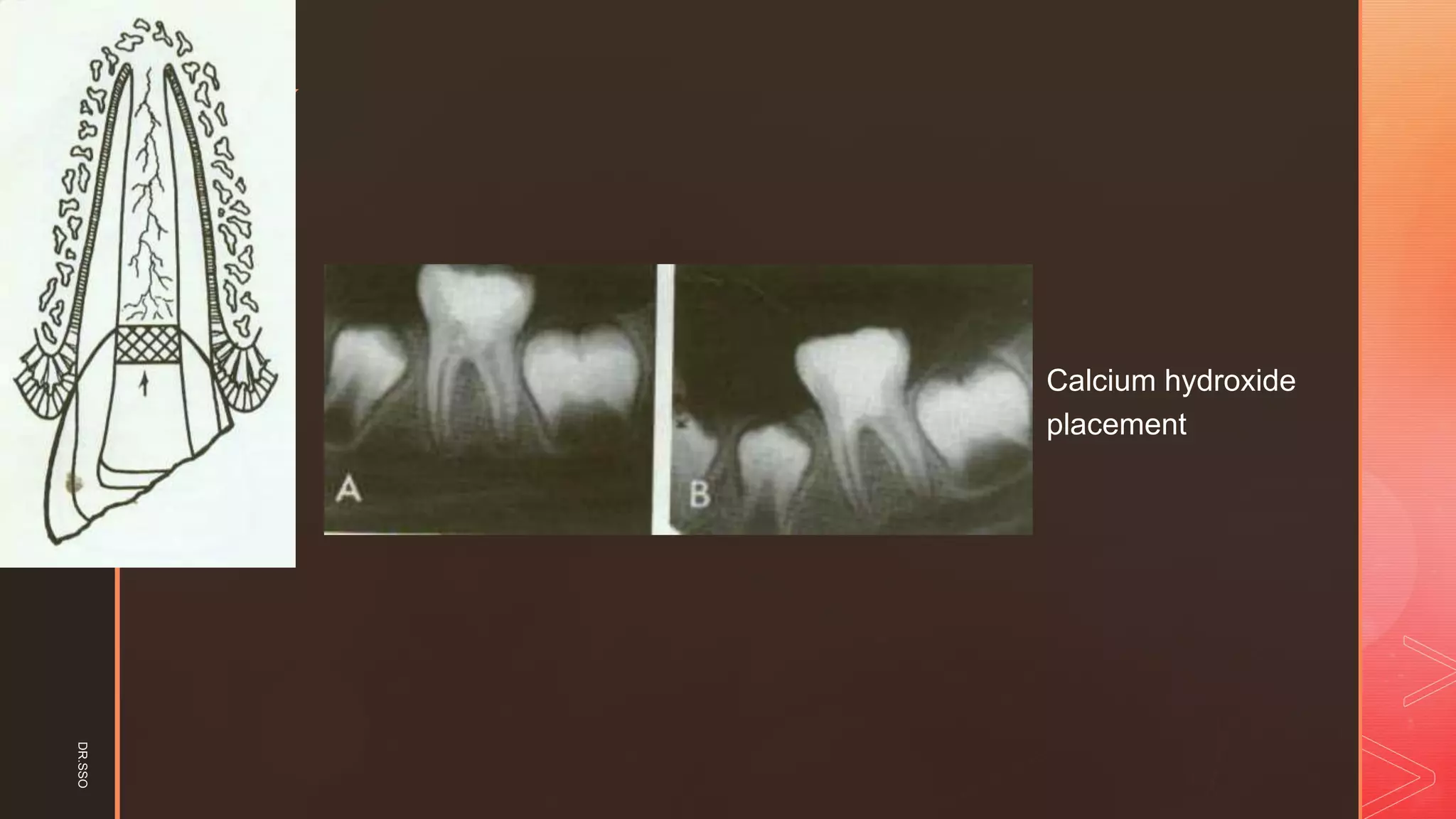
▪ Bleeding of the pulp stump was controlled with
saline on a cotton pellet applied with gentle
pressure.
▪ [Ca(OH)2]: Calcium hydroxide powder was
mixed with saline to a thick consistency. The
paste was carefully placed on the pulp stump
surface 1 to 2 mm thick.
Removal of coronal pulp
Haemostasis
DR.SSO](https://image.slidesharecdn.com/openapex-200815073253/75/Open-apex-its-Management-22-2048.jpg)