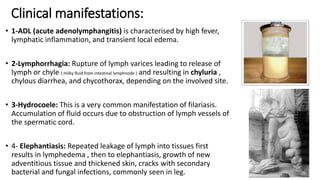
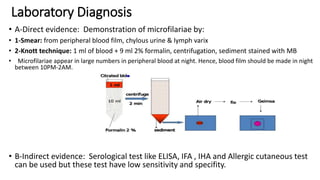
1. Filariasis is caused by Wuchereria Bancrofti and manifests as lymphatic obstruction leading to lymphedema and elephantiasis. It is diagnosed by demonstrating microfilariae in blood smears or lymph fluid.
2. Loa-Loa causes transient subcutaneous swellings as the adult worm migrates and can enter the eye. Microfilariae are found in blood during the day.
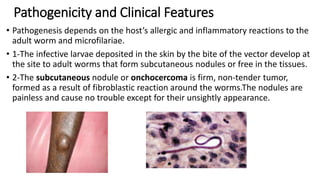
3. Onchocerca Volvulus causes skin and eye lesions from microfilariae and adults form subcutaneous nodules. It is diagnosed by finding microfilariae in skin snips or eye tissue. Mass ivermectin treatment and