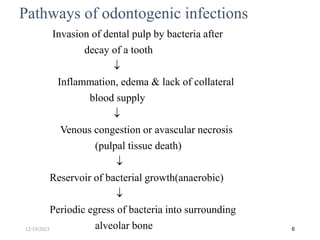
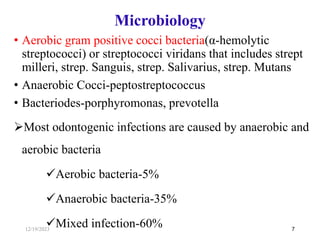
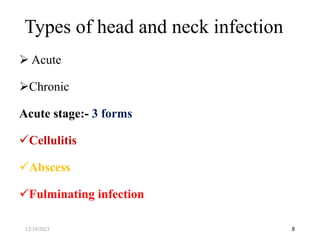
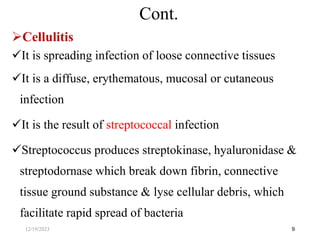
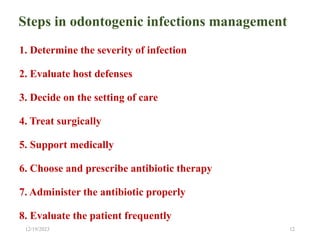
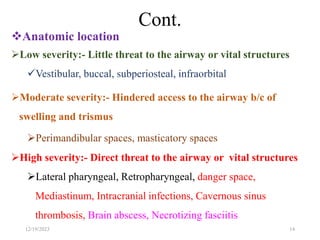
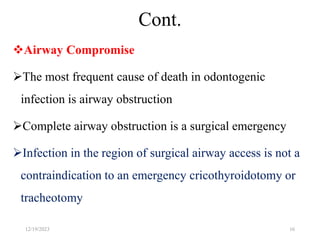
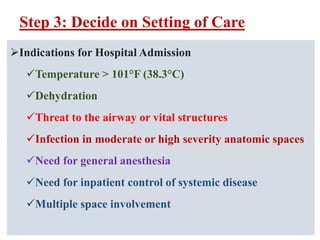
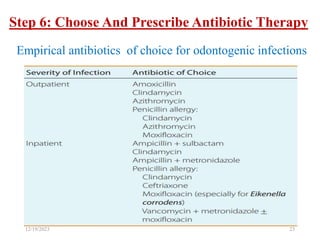
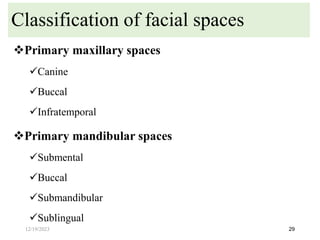
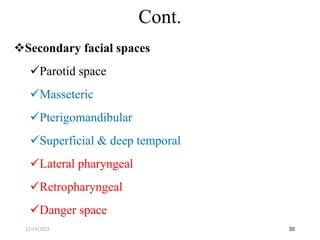
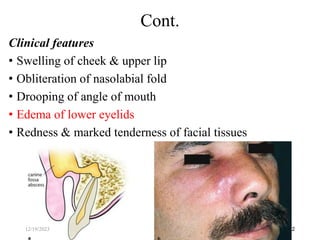
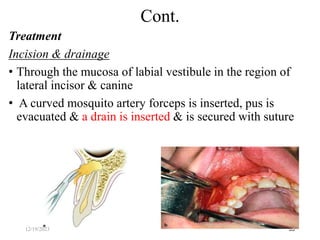
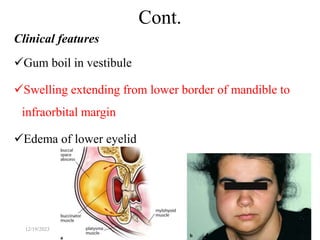
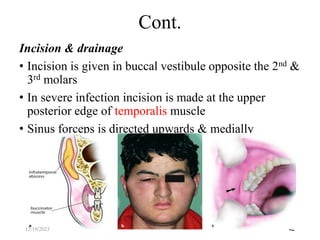
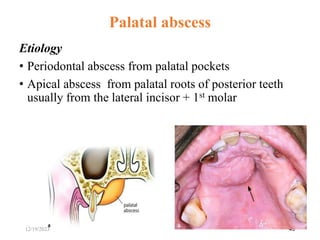
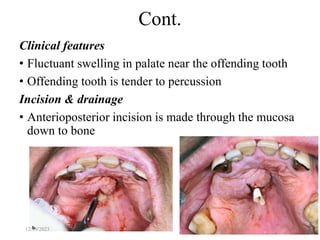
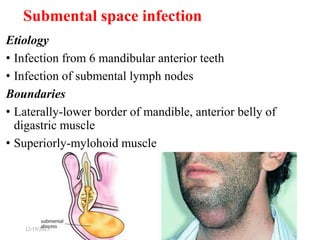
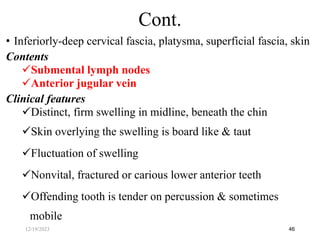
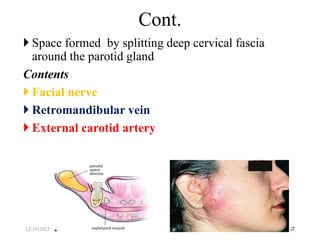
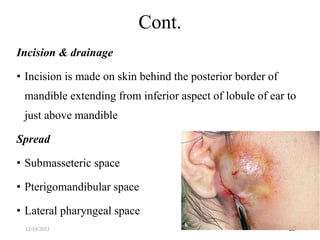
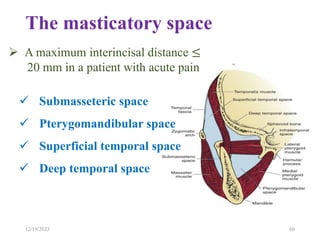
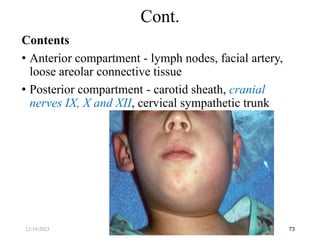
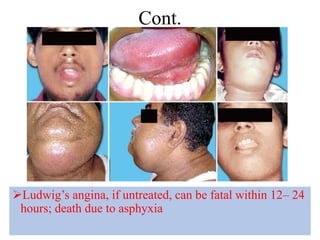
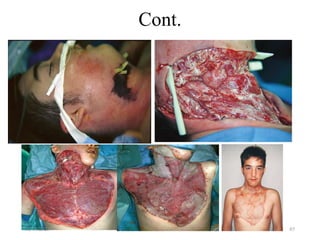
The document discusses head and neck space infections, including their etiology, microbiology, classification of facial spaces, and principles of management. It provides details on specific spaces like the canine, buccal, infratemporal, and submental spaces. Guidelines are presented on determining the severity of infection, evaluating the patient, surgical and antibiotic treatment, and monitoring for treatment response.