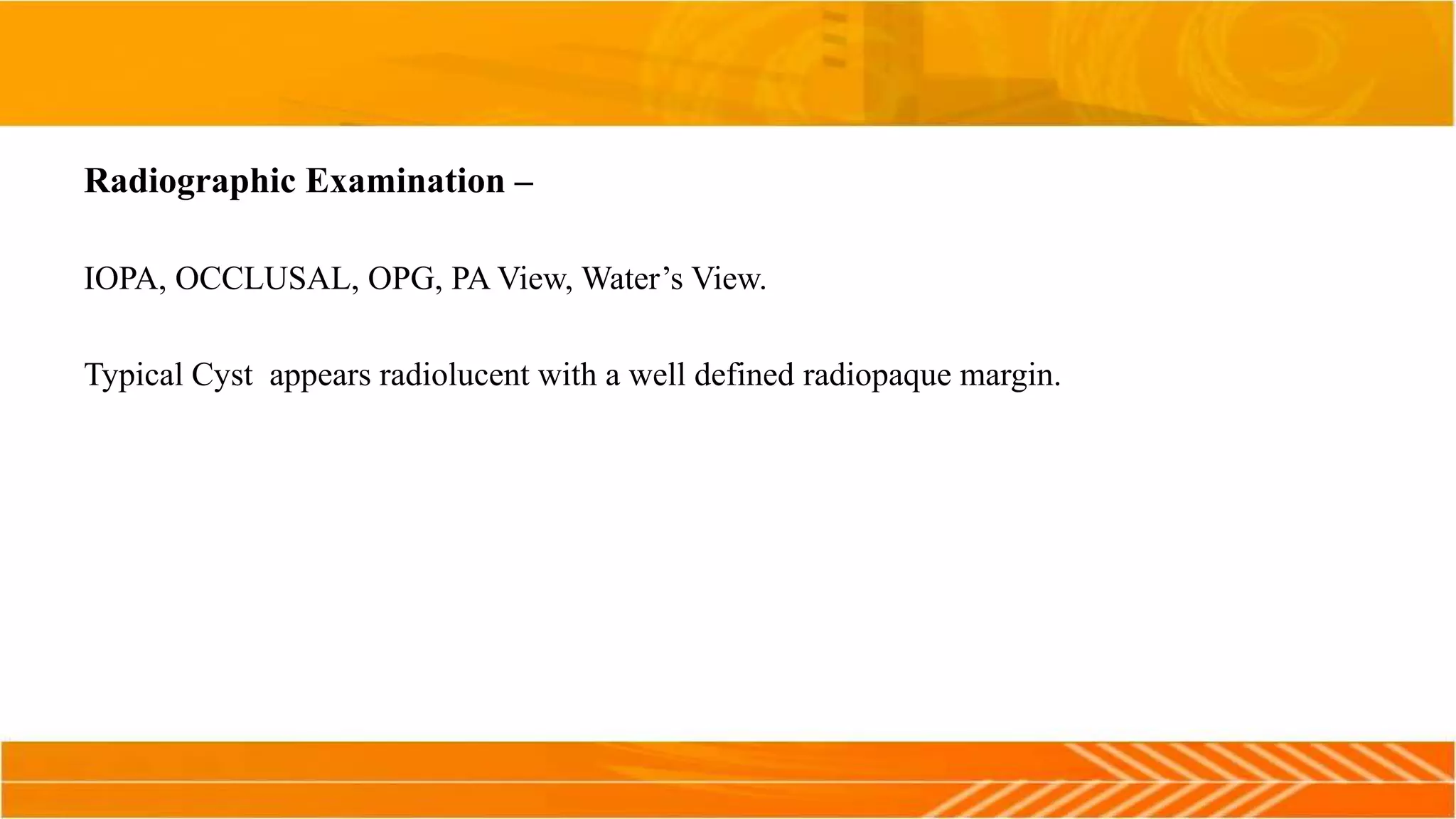
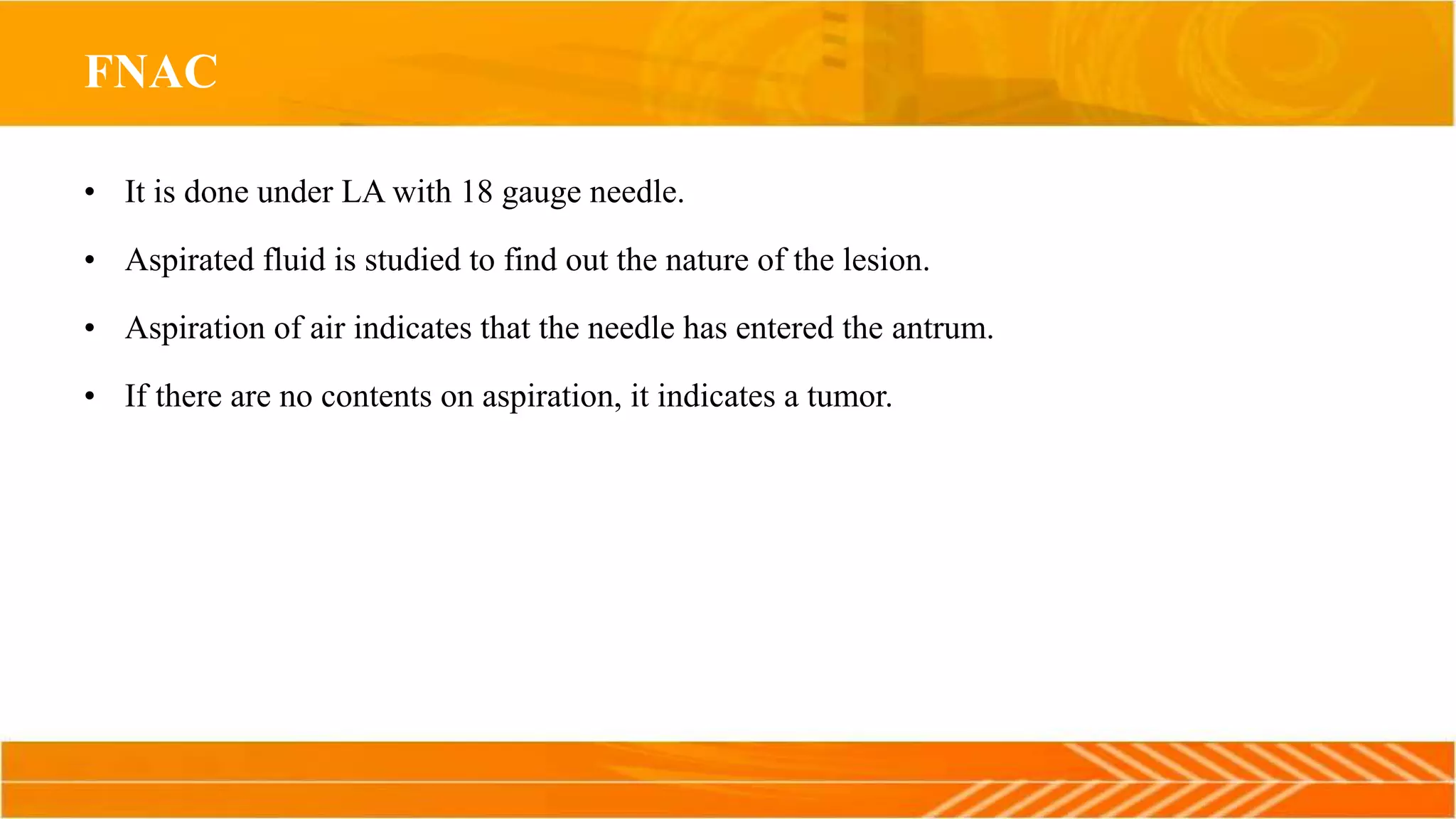
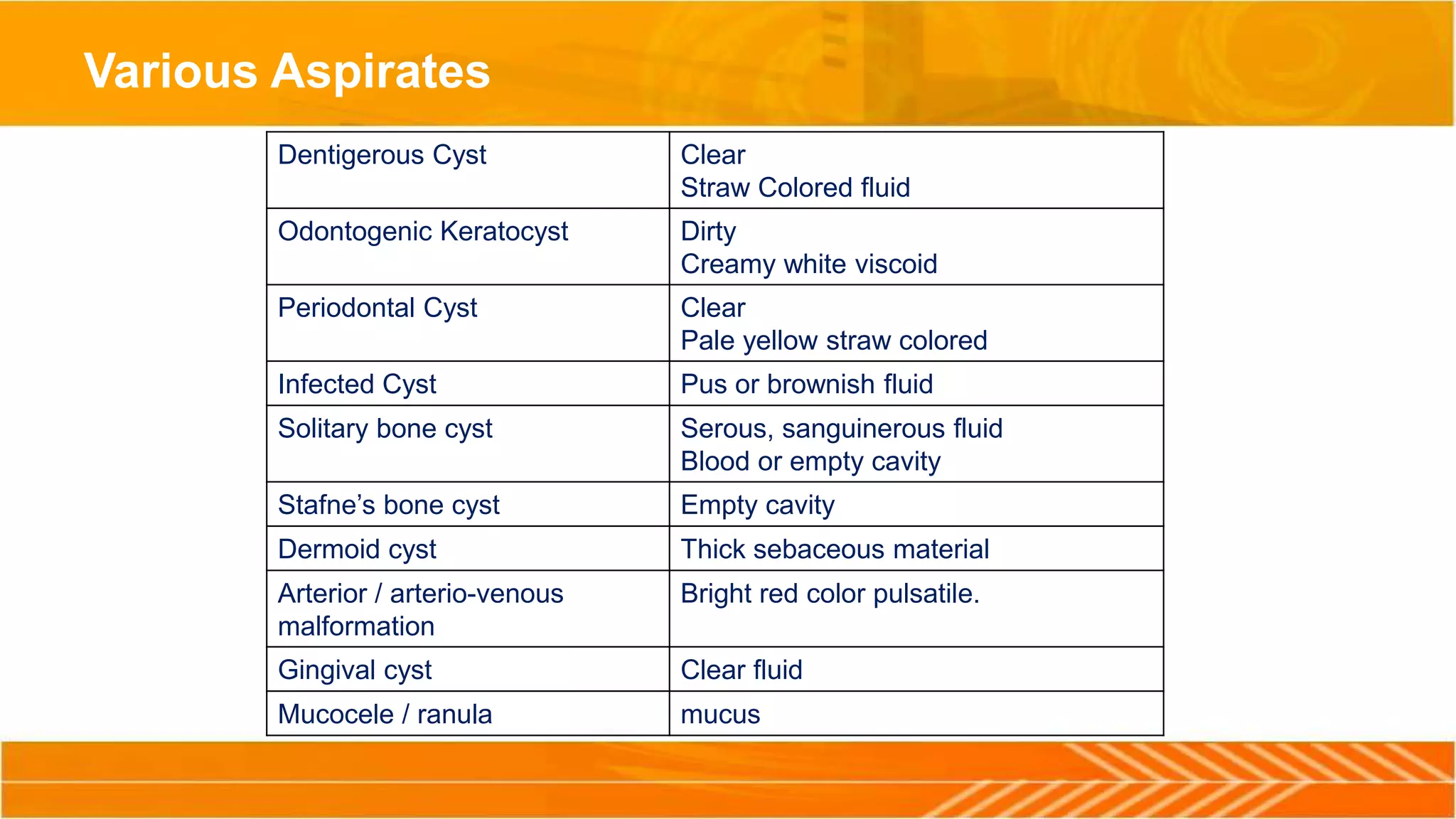
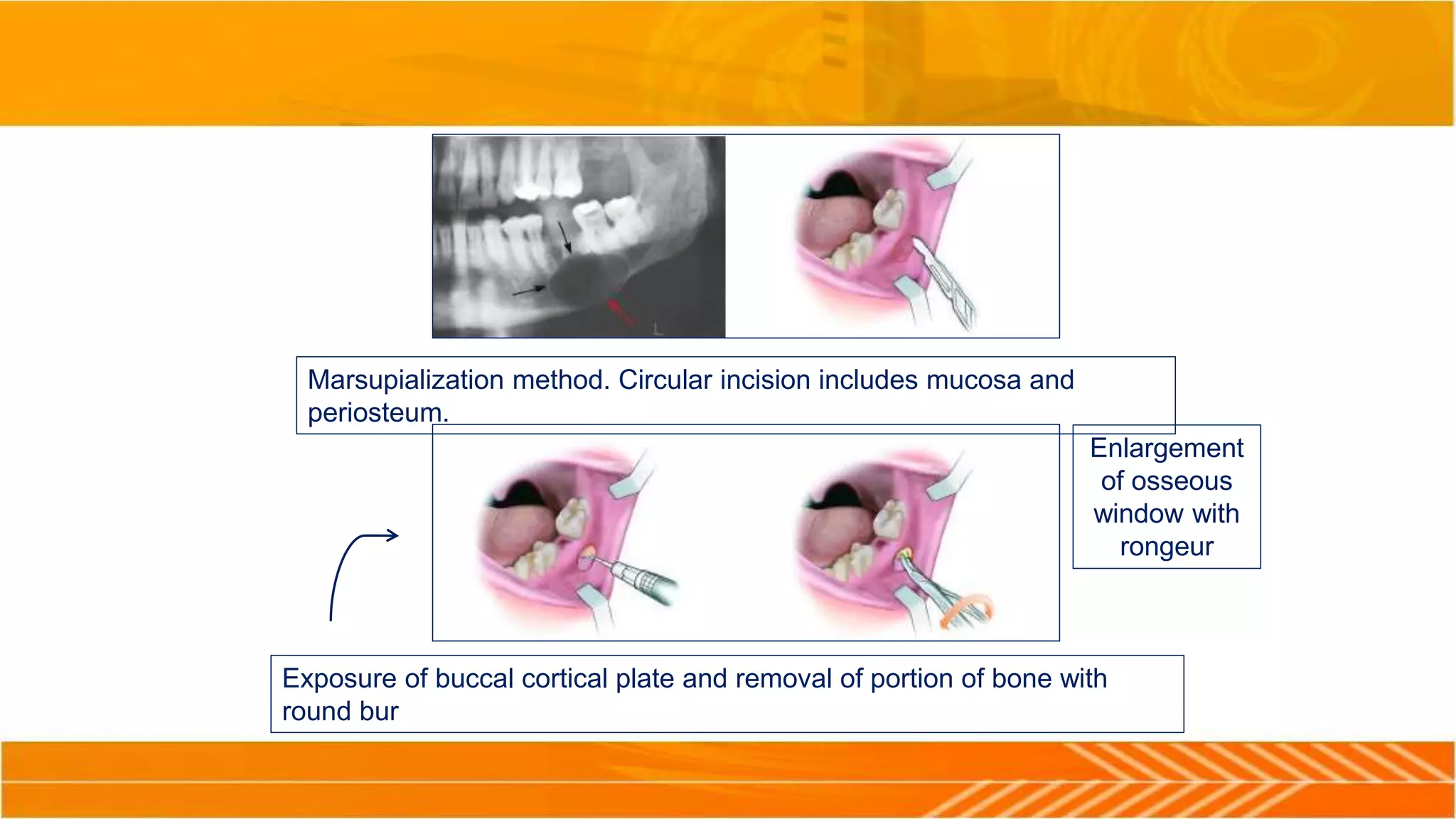
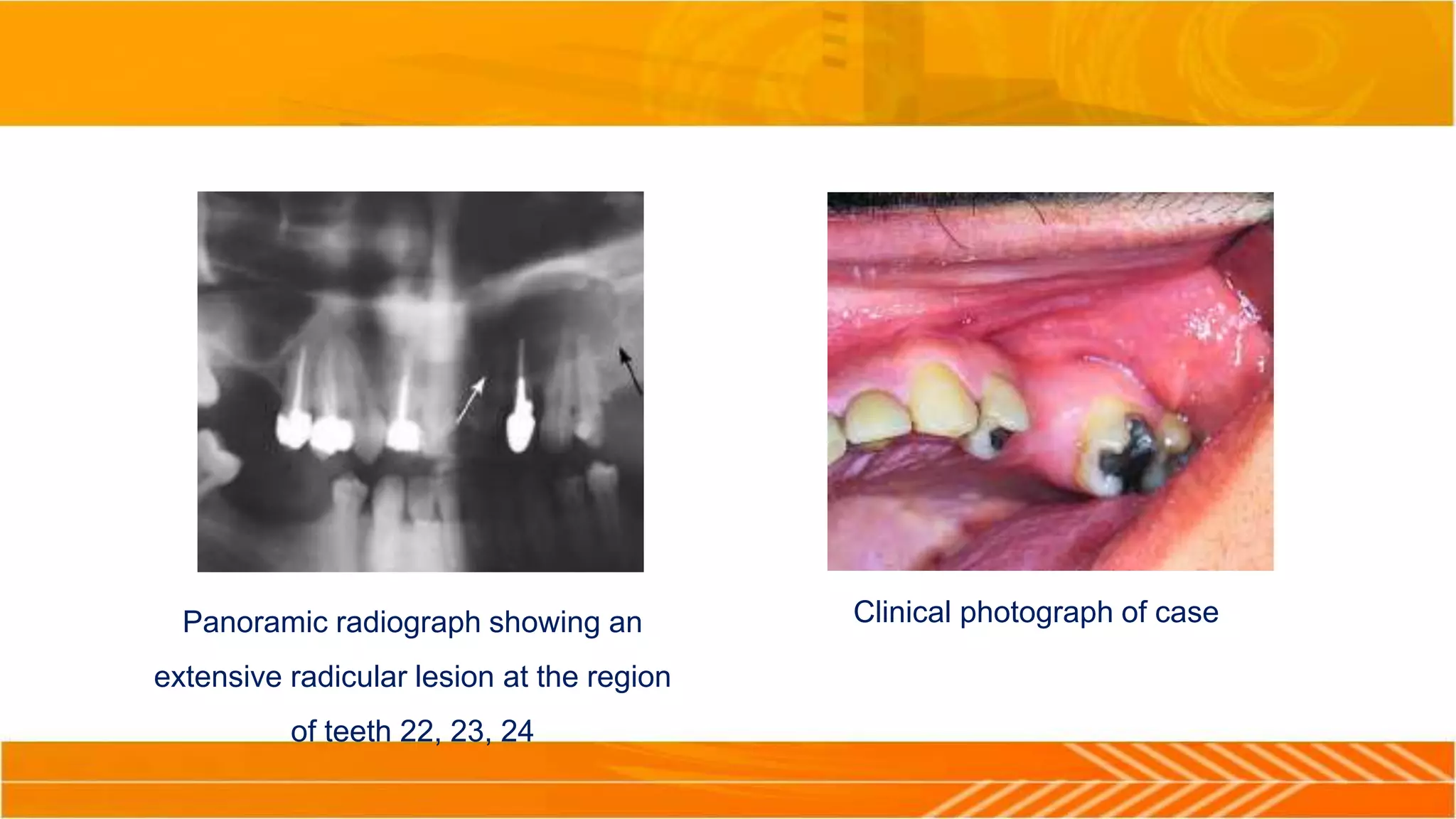
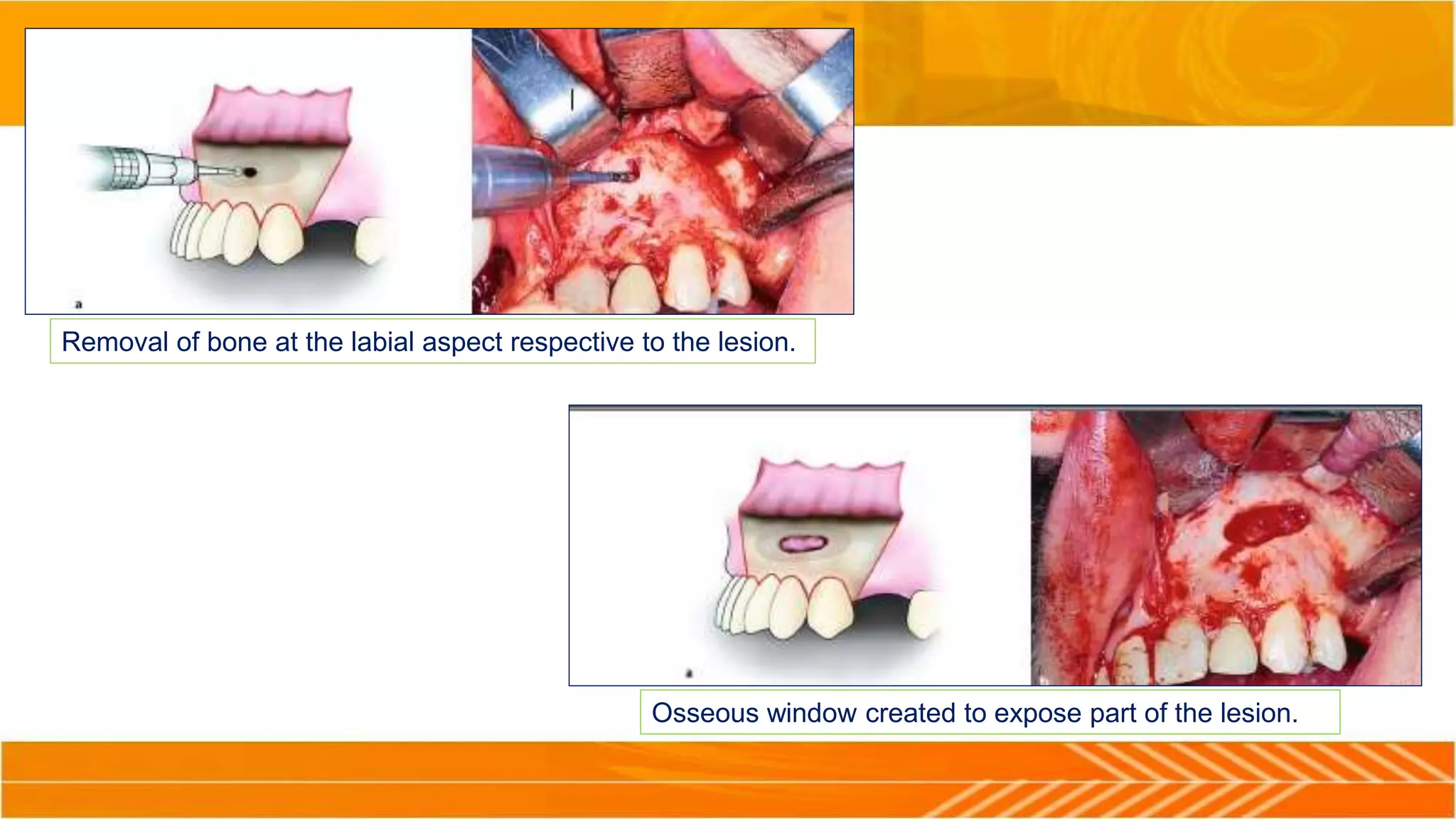
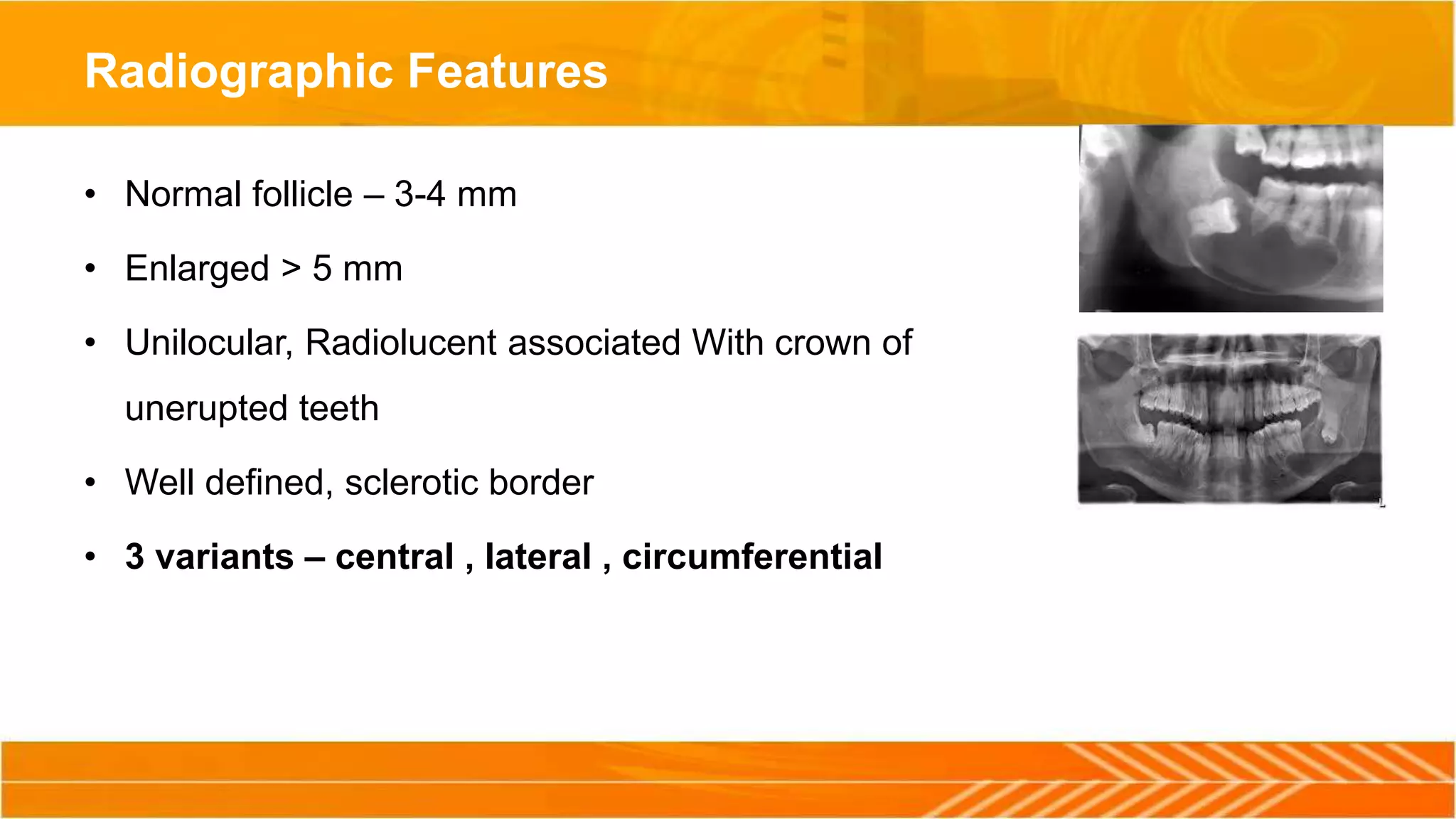
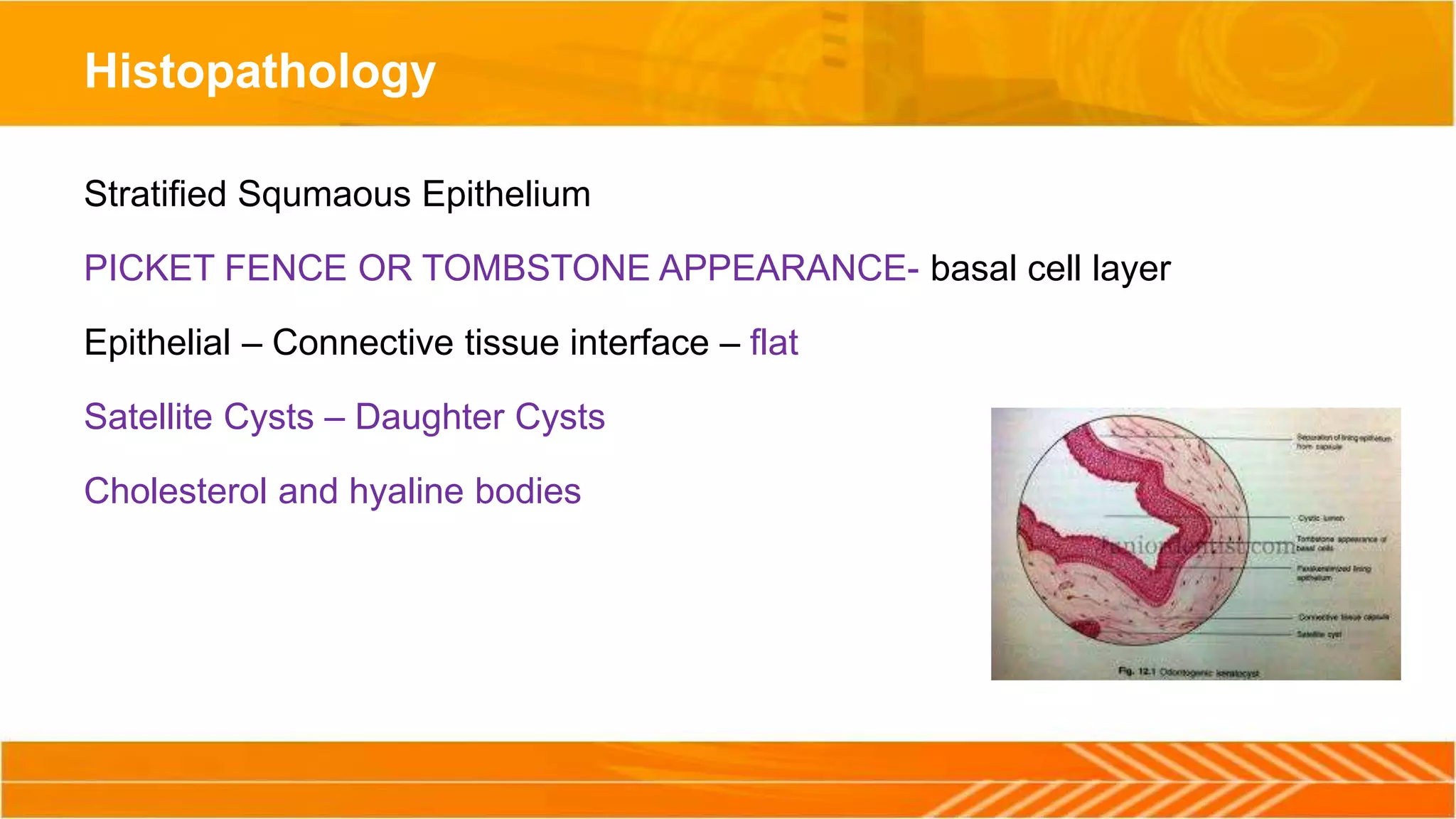
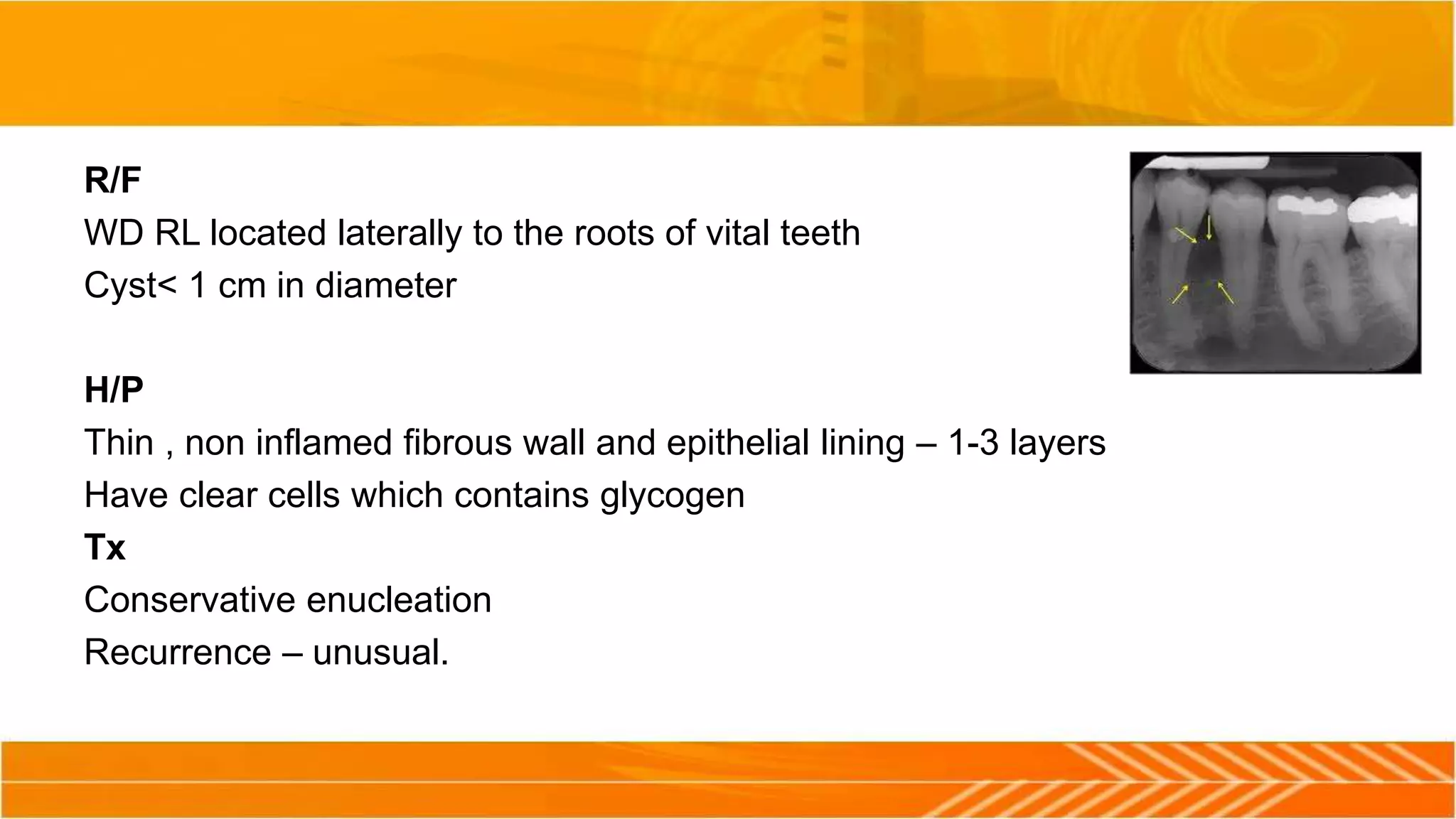
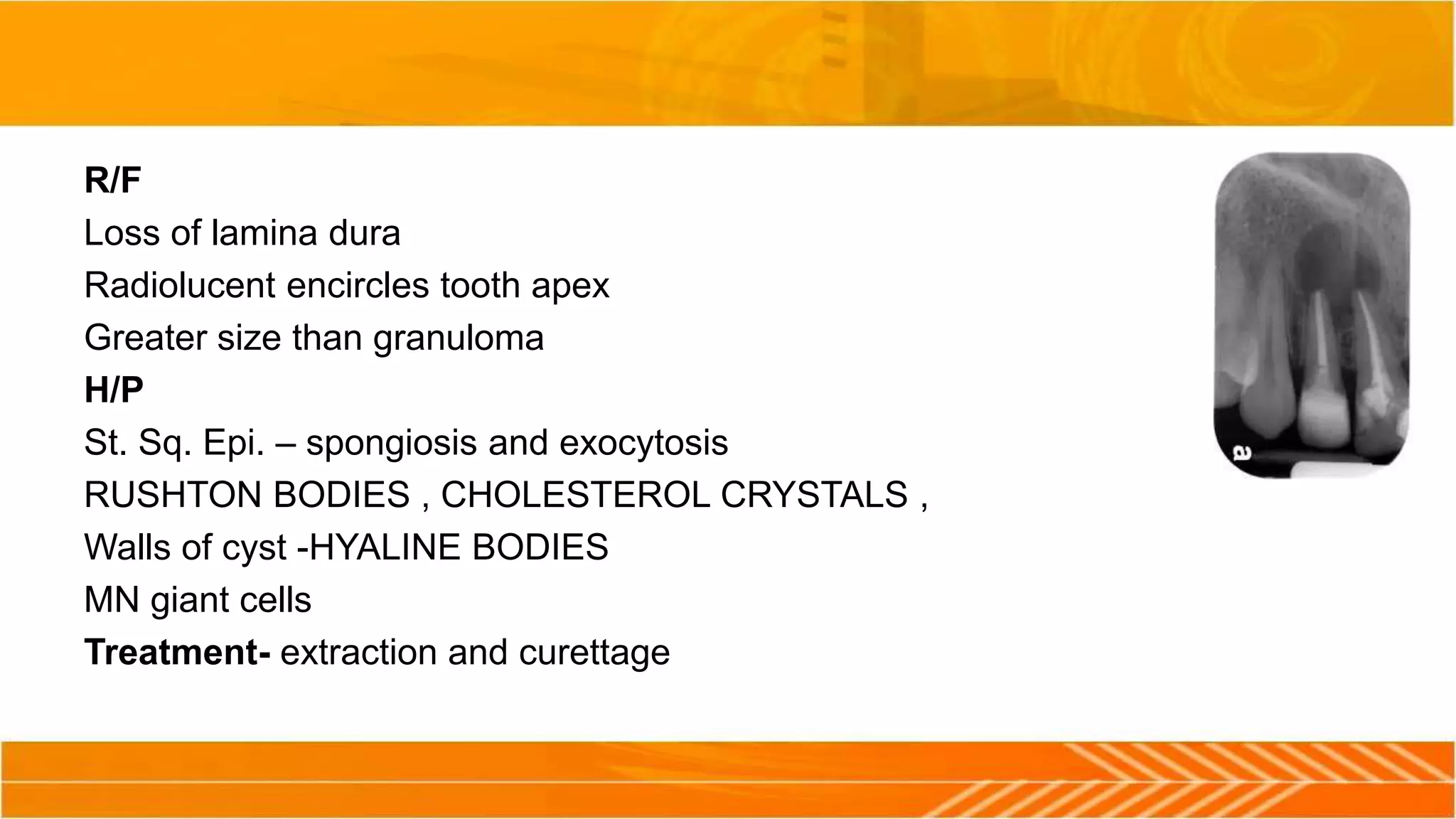
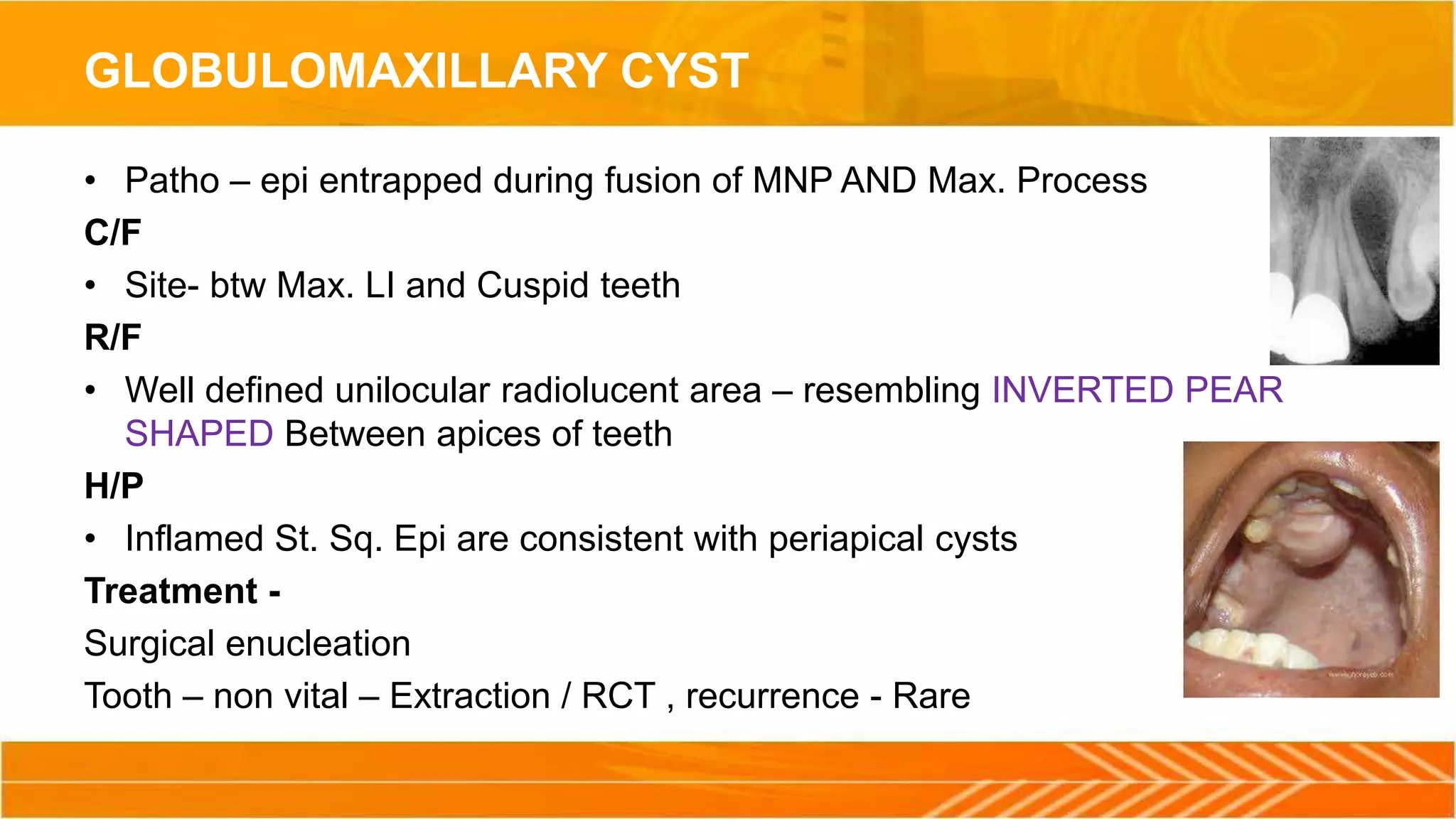
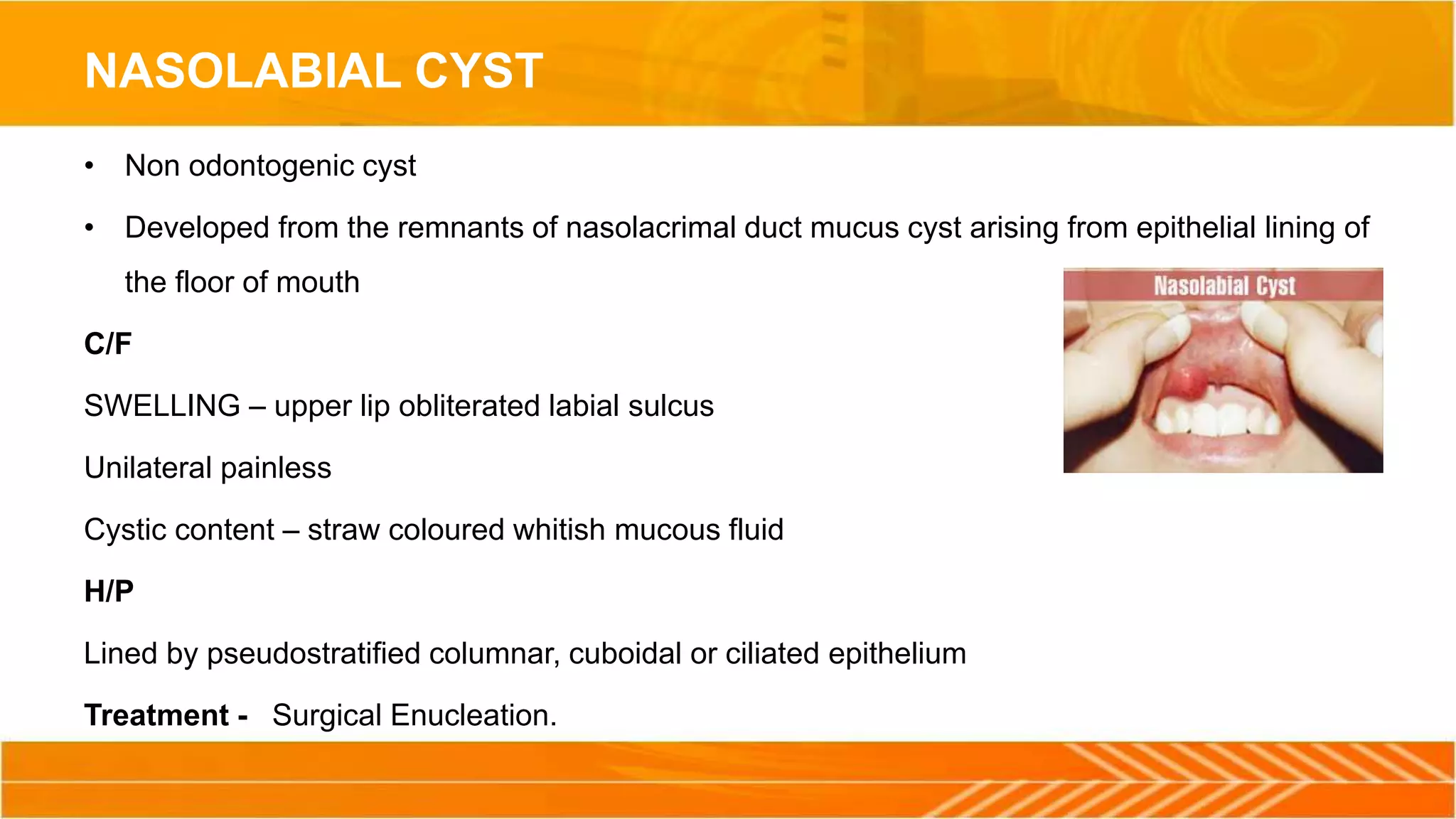
This document discusses cysts of the jaw, including definitions, types, pathogenesis, diagnosis, and treatment. It describes the two main types of cysts as true cysts lined by epithelium and pseudo cysts not lined by epithelium. Common jaw cysts discussed include dentigerous cysts, odontogenic keratocysts, and radicular cysts. The pathogenesis and theories of cyst enlargement are explained. Diagnostic methods like radiography, FNAC, and biopsy are outlined. Surgical treatment options for cyst removal include marsupialization, enucleation, enucleation with chemical cauterization, and resection.