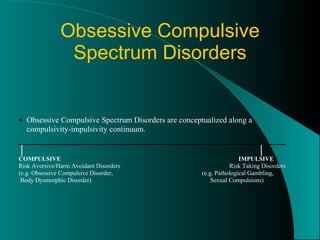
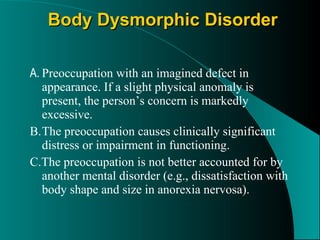
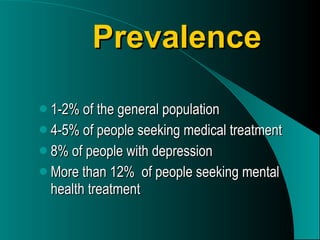
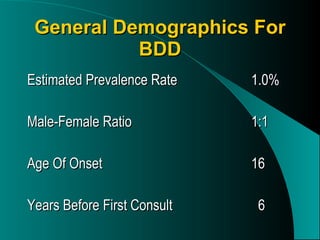
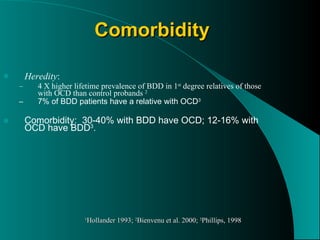
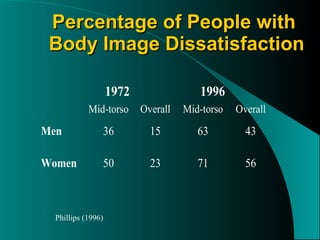
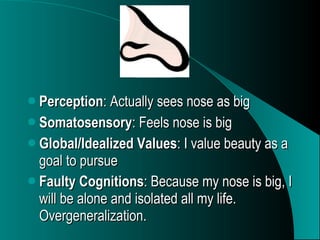
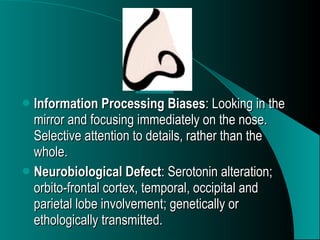
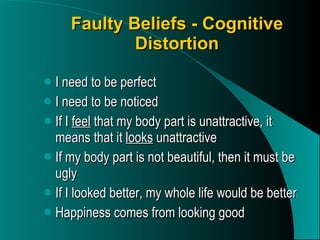
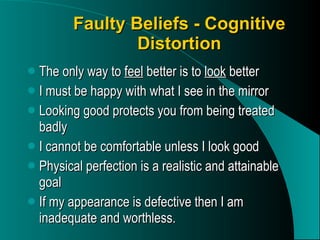
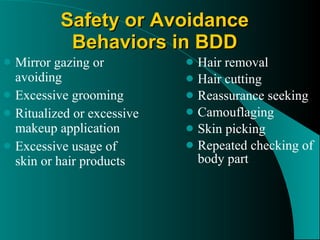
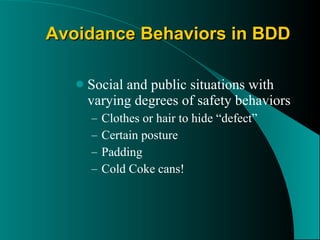
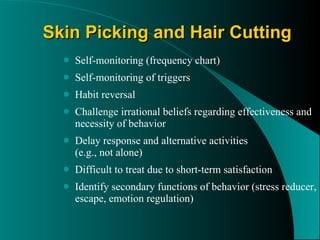
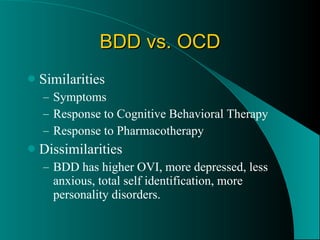
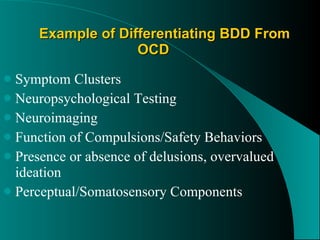
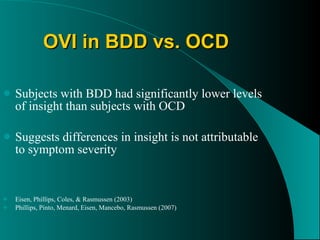
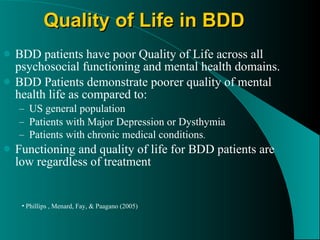
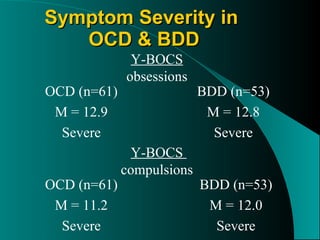
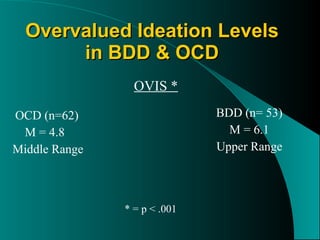
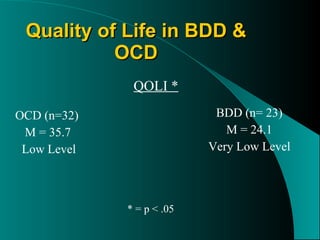
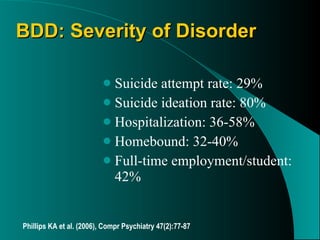
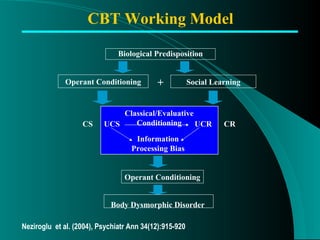
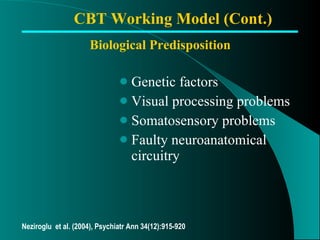
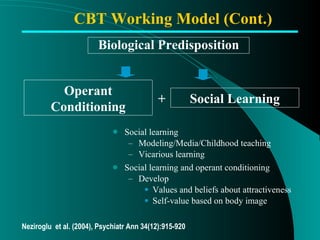
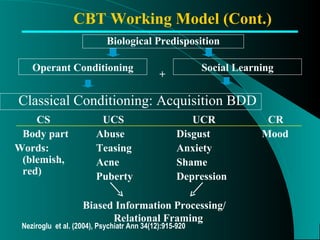
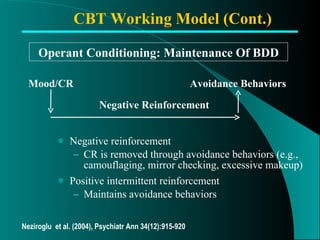
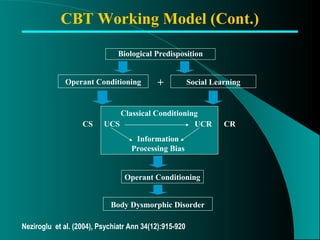
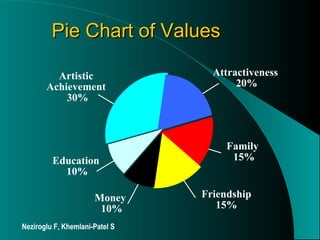
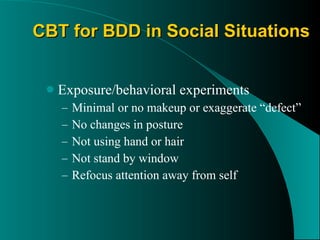
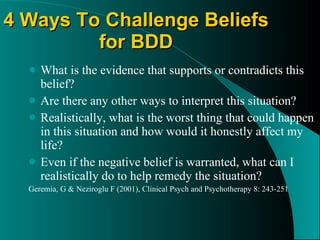
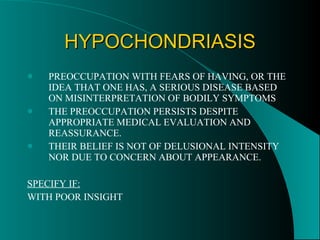
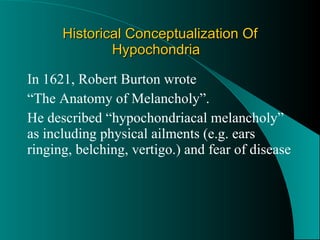
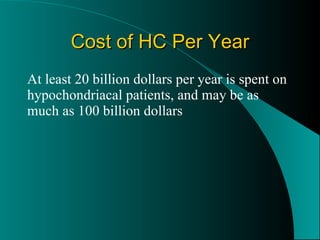
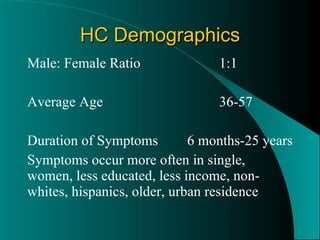
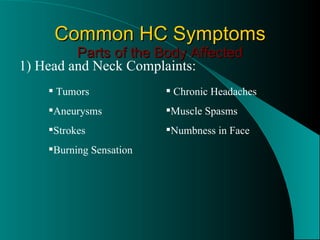
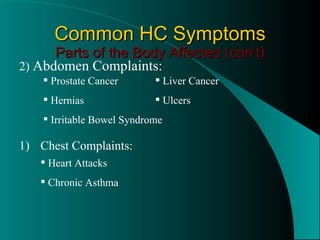
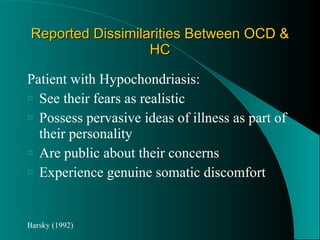
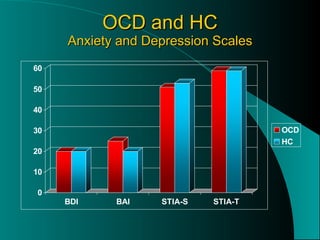
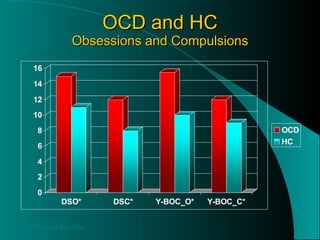
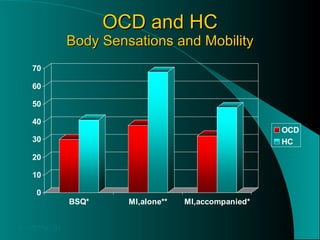
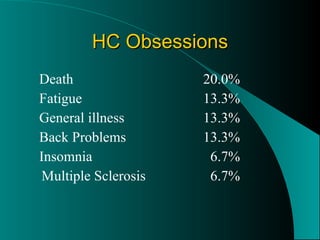
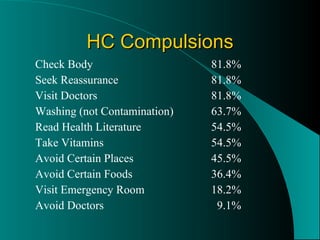
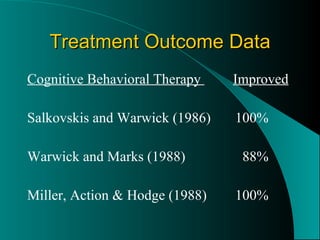
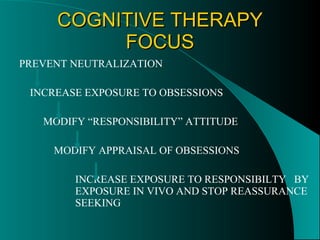
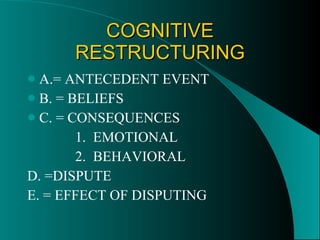
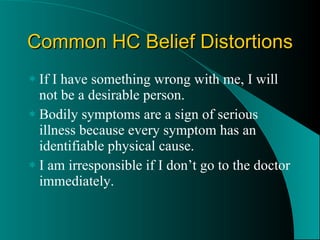
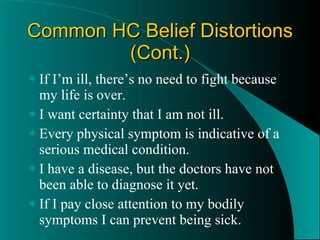
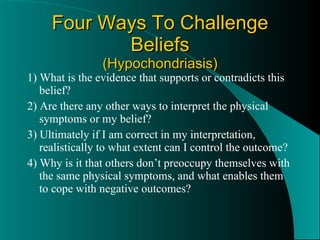
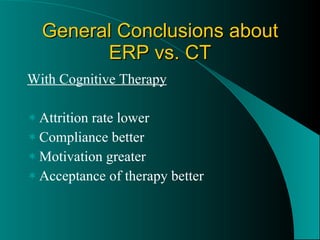
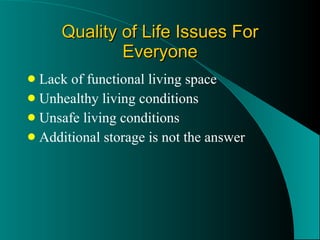
The document discusses Body Dysmorphic Disorder (BDD) and Hypochondriasis. It compares the two disorders and outlines their key characteristics, including prevalence, demographics, comorbidities, and treatments. BDD involves a preoccupation with an imagined or slight defect in appearance. Hypochondriasis involves a preoccupation with fears of having a serious illness despite medical reassurance. Both disorders share similarities with OCD but also have distinct features and impacts on quality of life. Cognitive-behavioral therapy is an appropriate treatment approach for both.