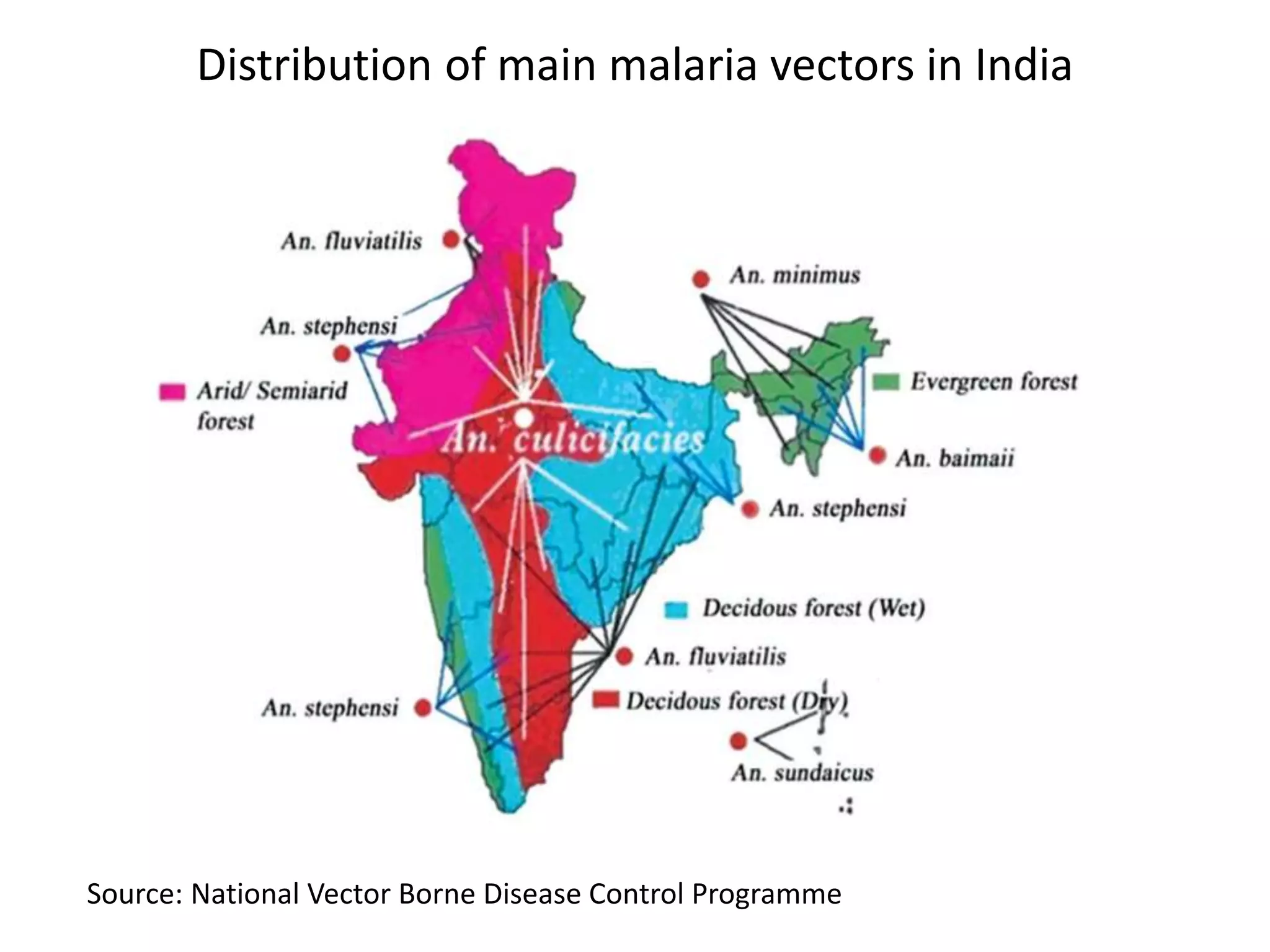
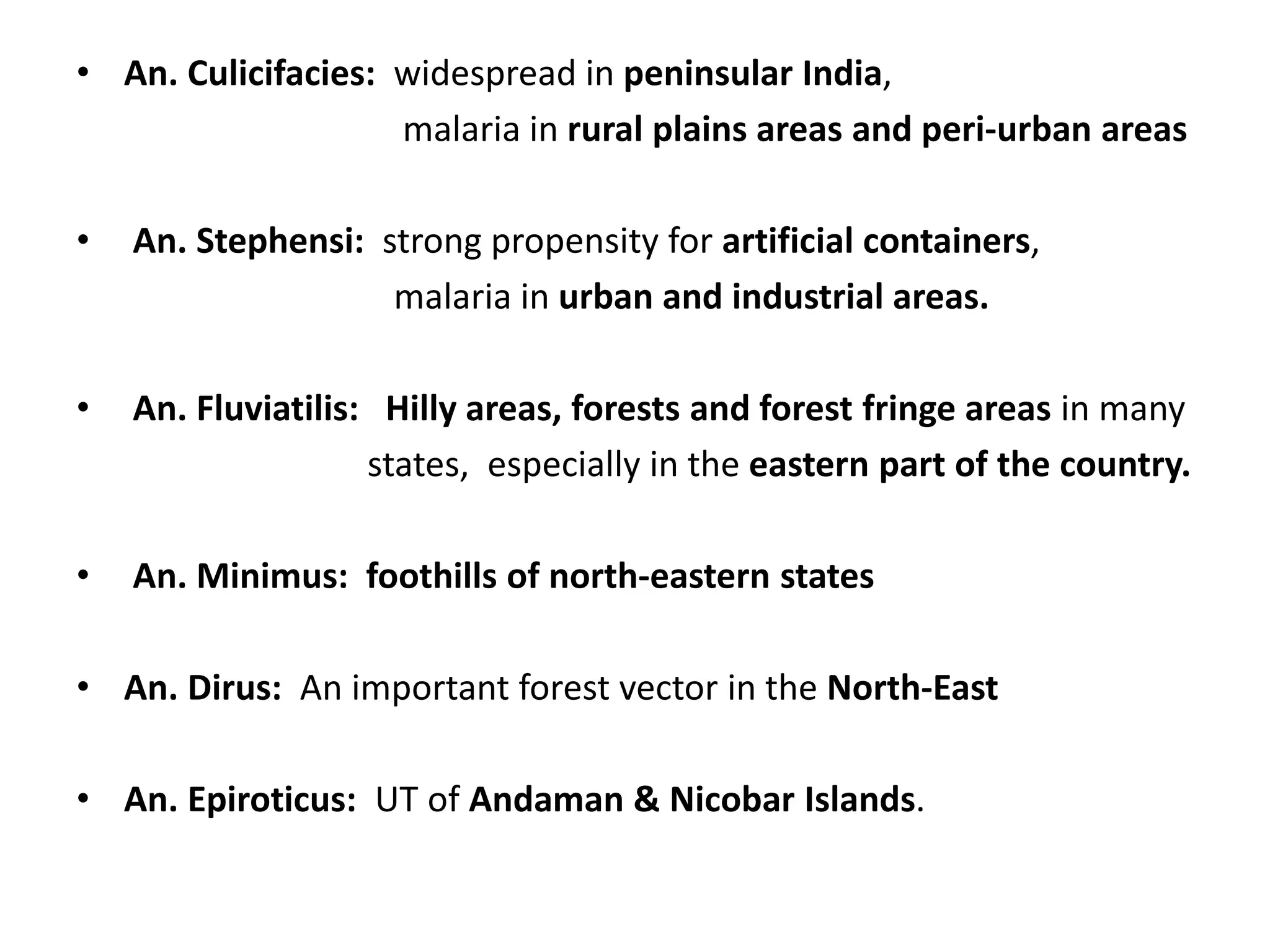
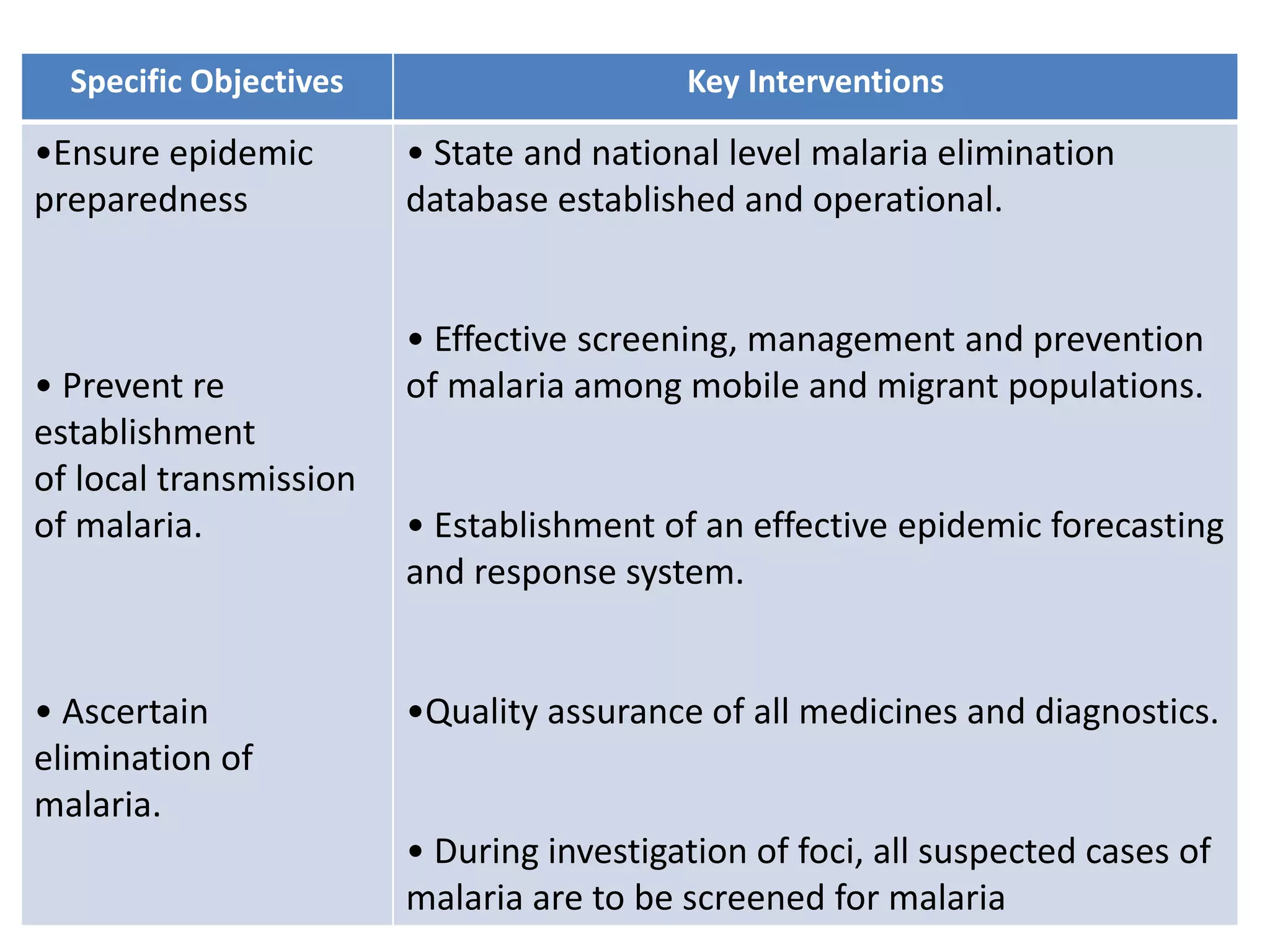
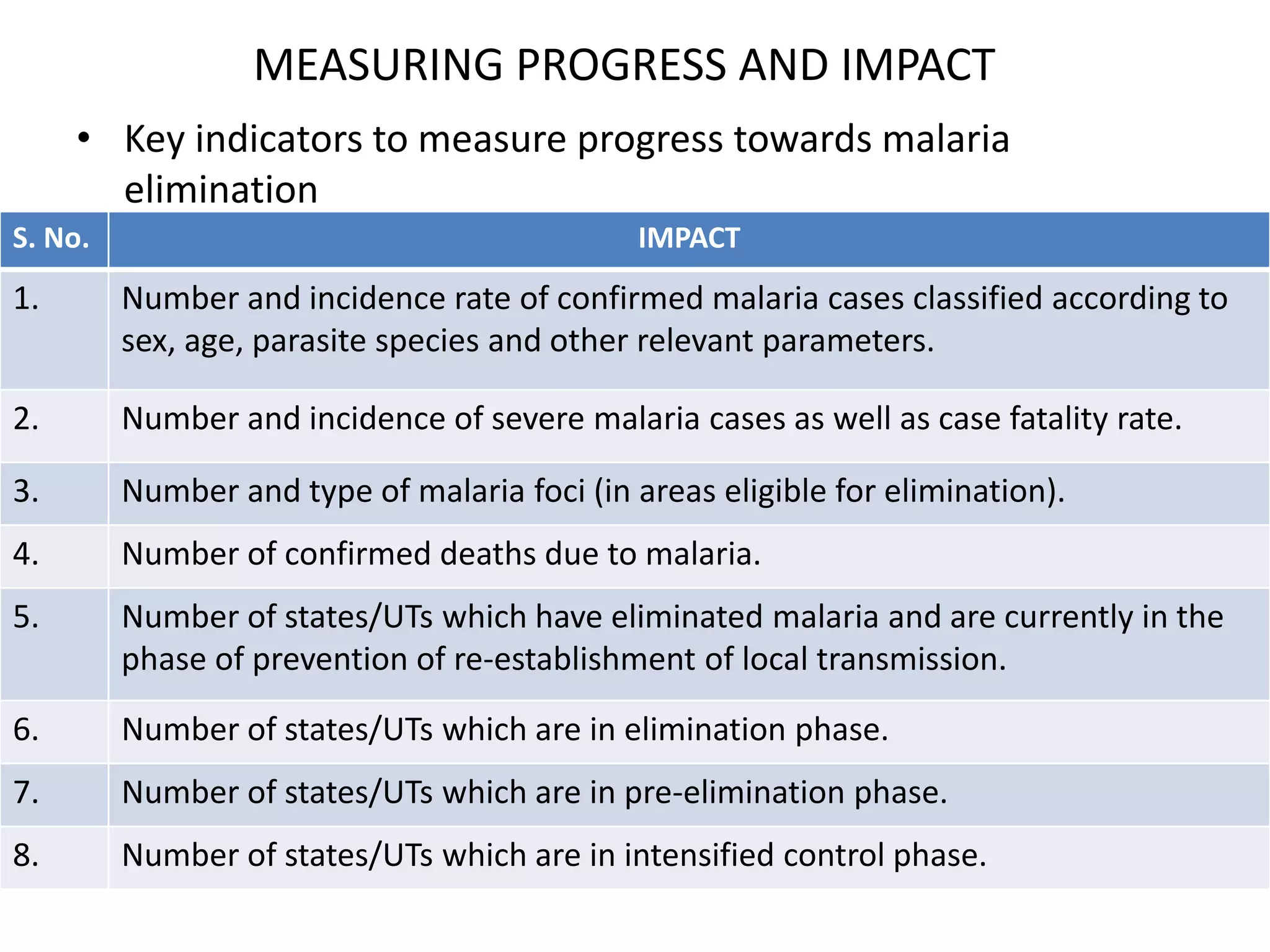
The document provides a history of malaria control in India and outlines the national framework for malaria elimination from 2016-2030. It discusses key milestones in malaria control, the current epidemiological profile and trends, strategic approaches, objectives and targets. The framework aims to eliminate malaria throughout India by 2030. Key interventions include scaling up prevention and treatment efforts, strengthening surveillance and response, and interrupting transmission in active foci. Progress will be measured using indicators like case incidence rates and numbers of states achieving elimination. Challenges to control include population movement, resource shortages, and insecticide resistance.