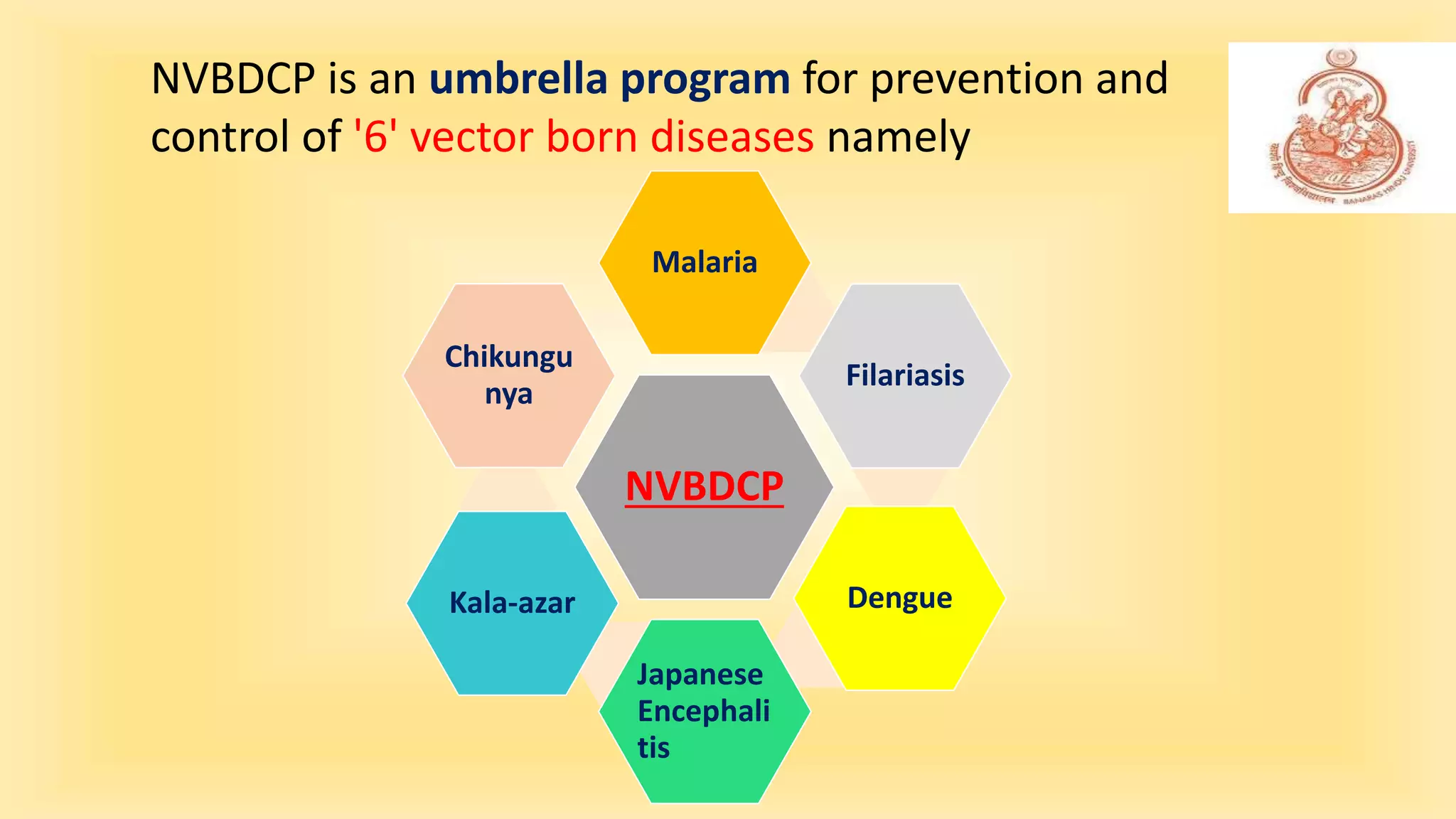
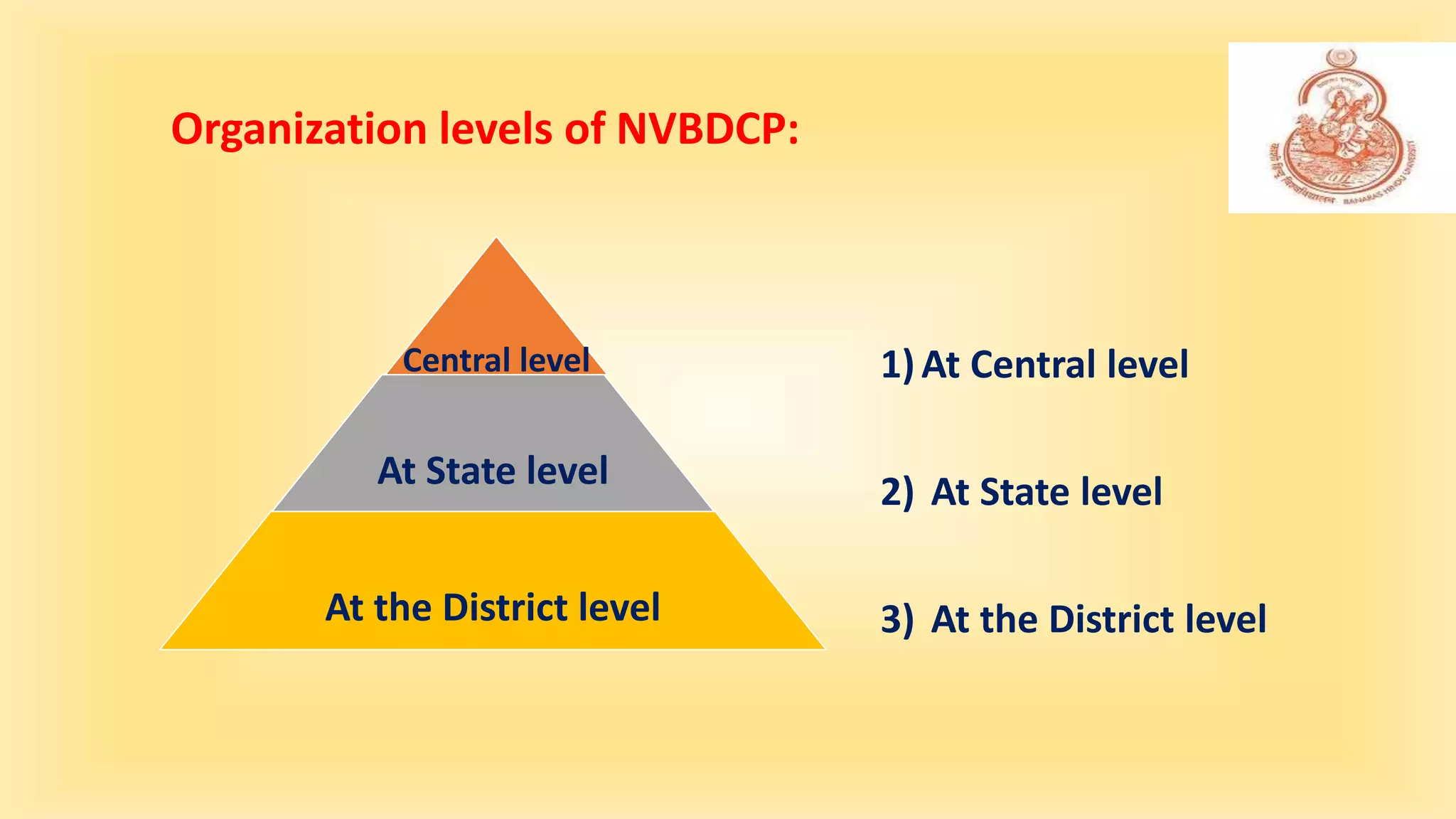
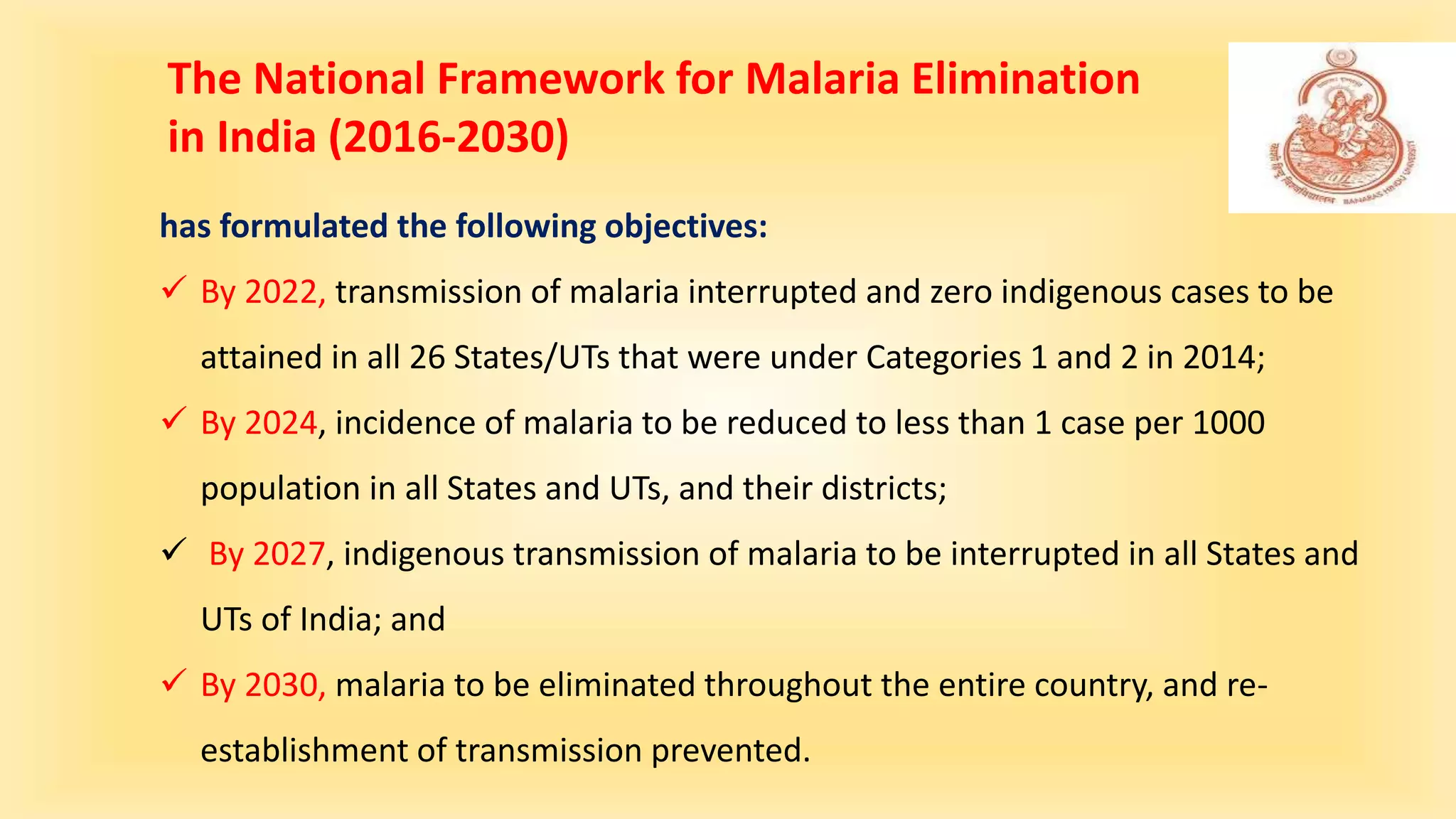
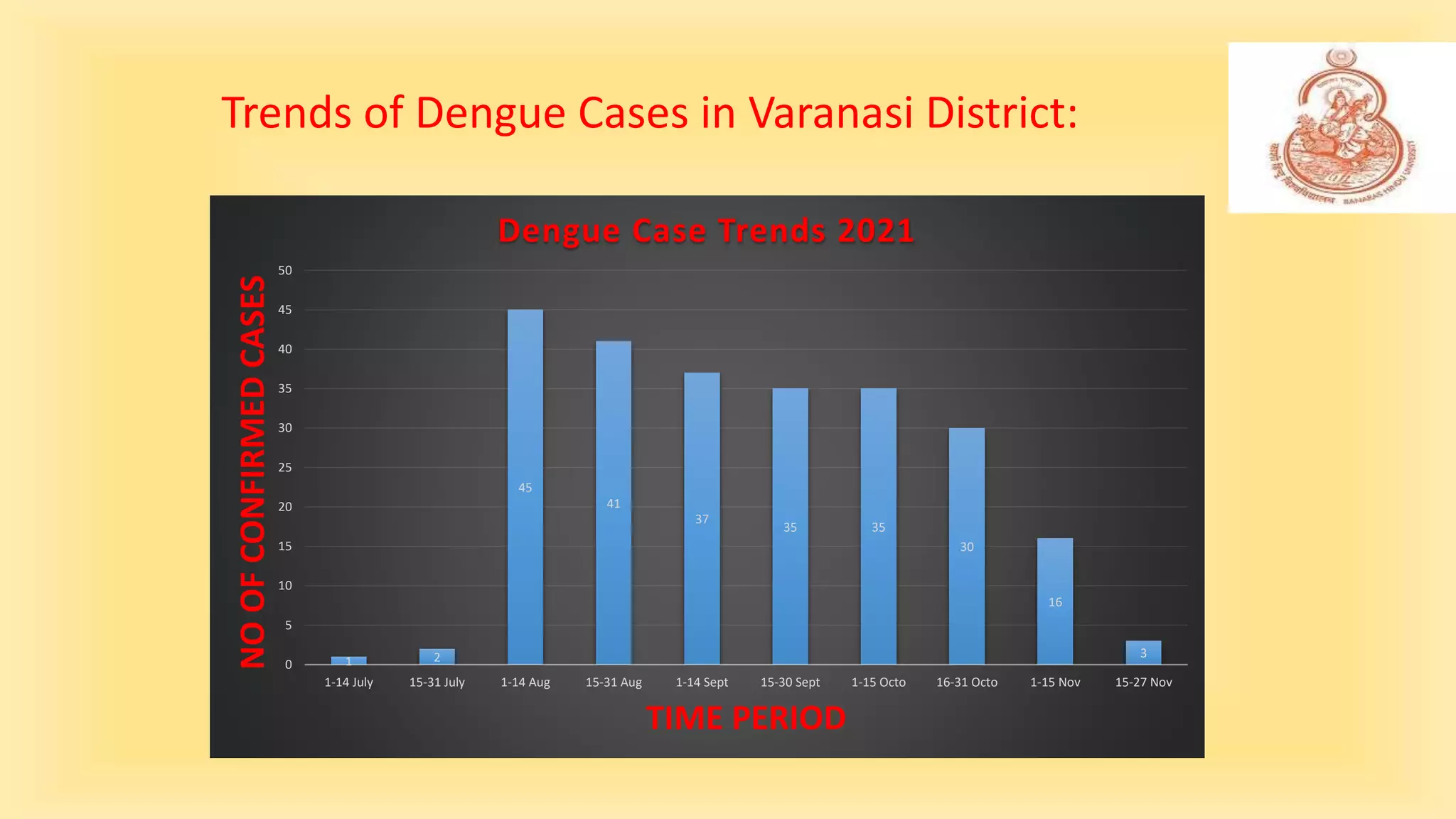
The National Vector Borne Disease Control Program (NVBDCP) aims to prevent and control six vector-borne diseases in India, including malaria and dengue, through a structured framework and multi-level governance. Launched in 2003, the program has set ambitious goals for disease elimination and employs various strategies, including surveillance, community participation, and integrated vector management. As of recent efforts, the program has seen progress in disease reduction, although challenges remain in achieving complete elimination targets.