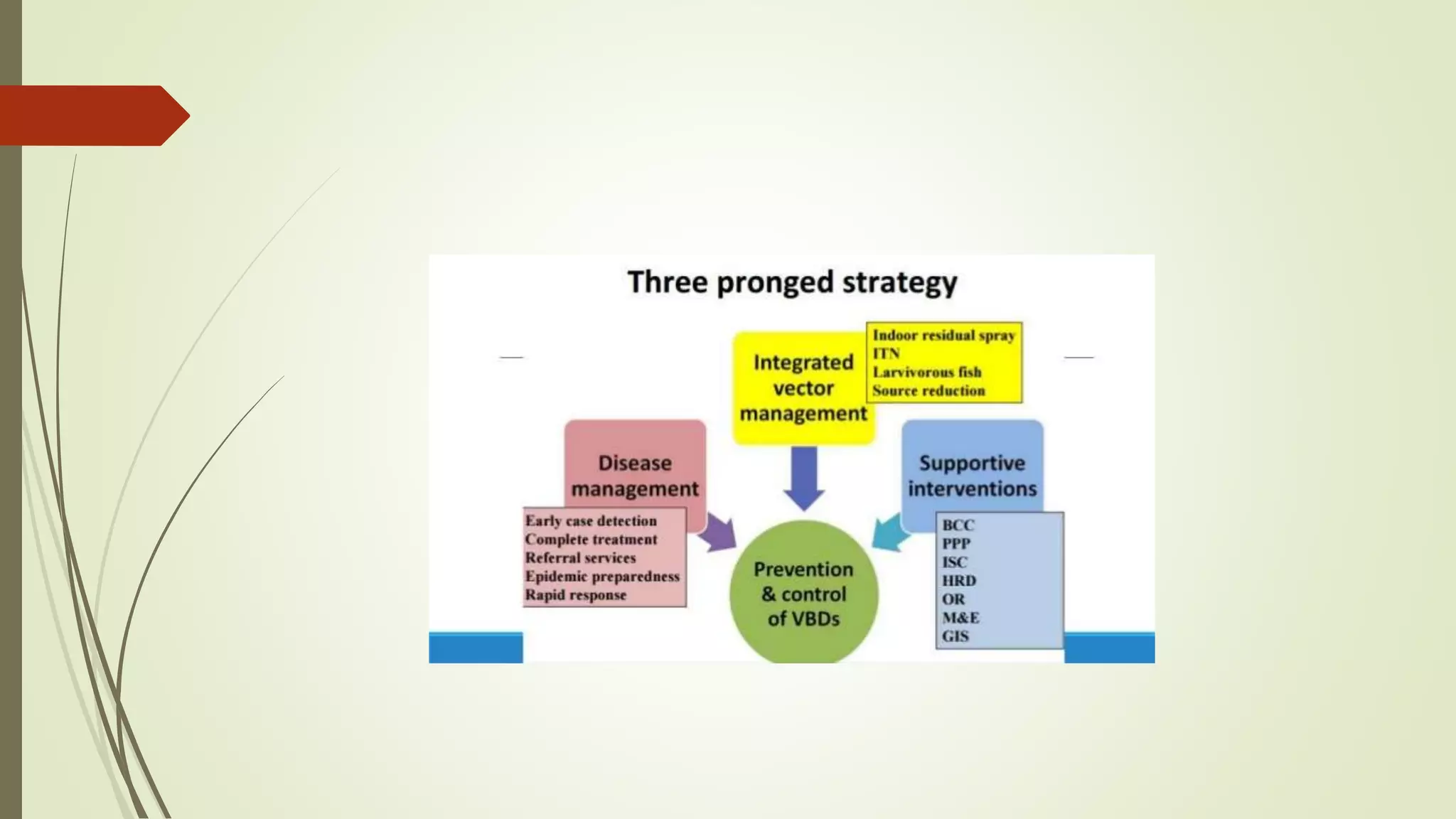
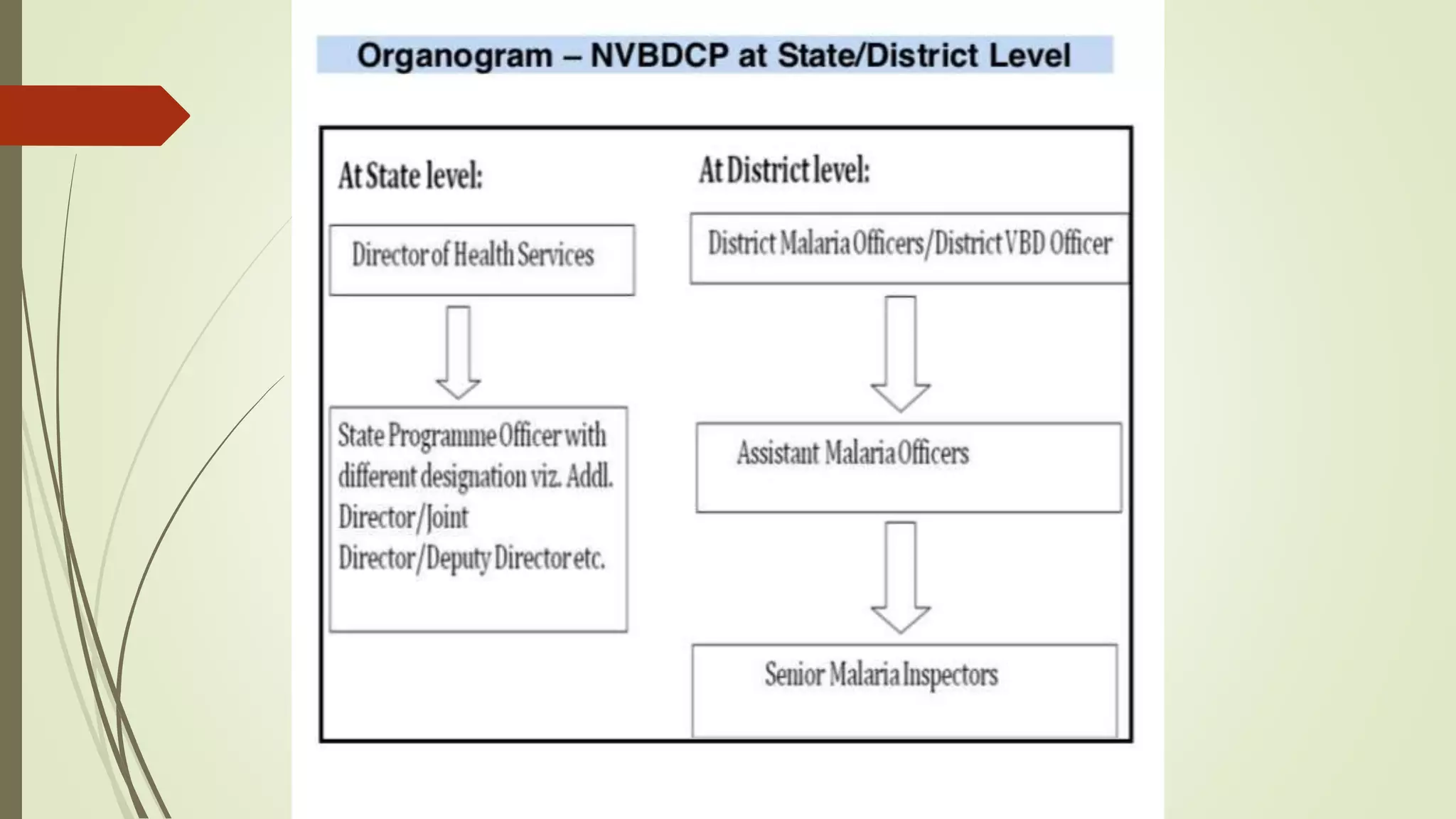
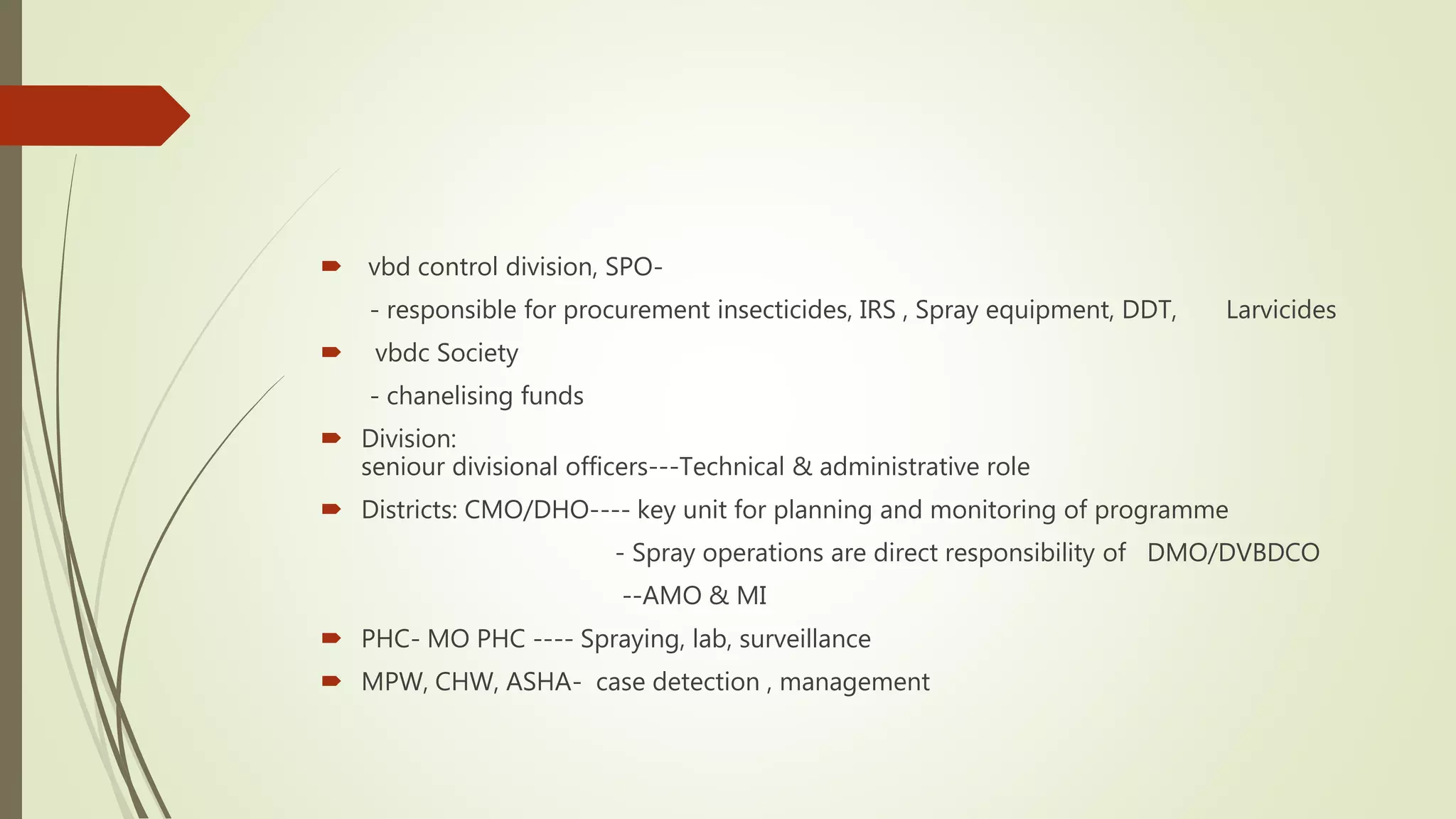
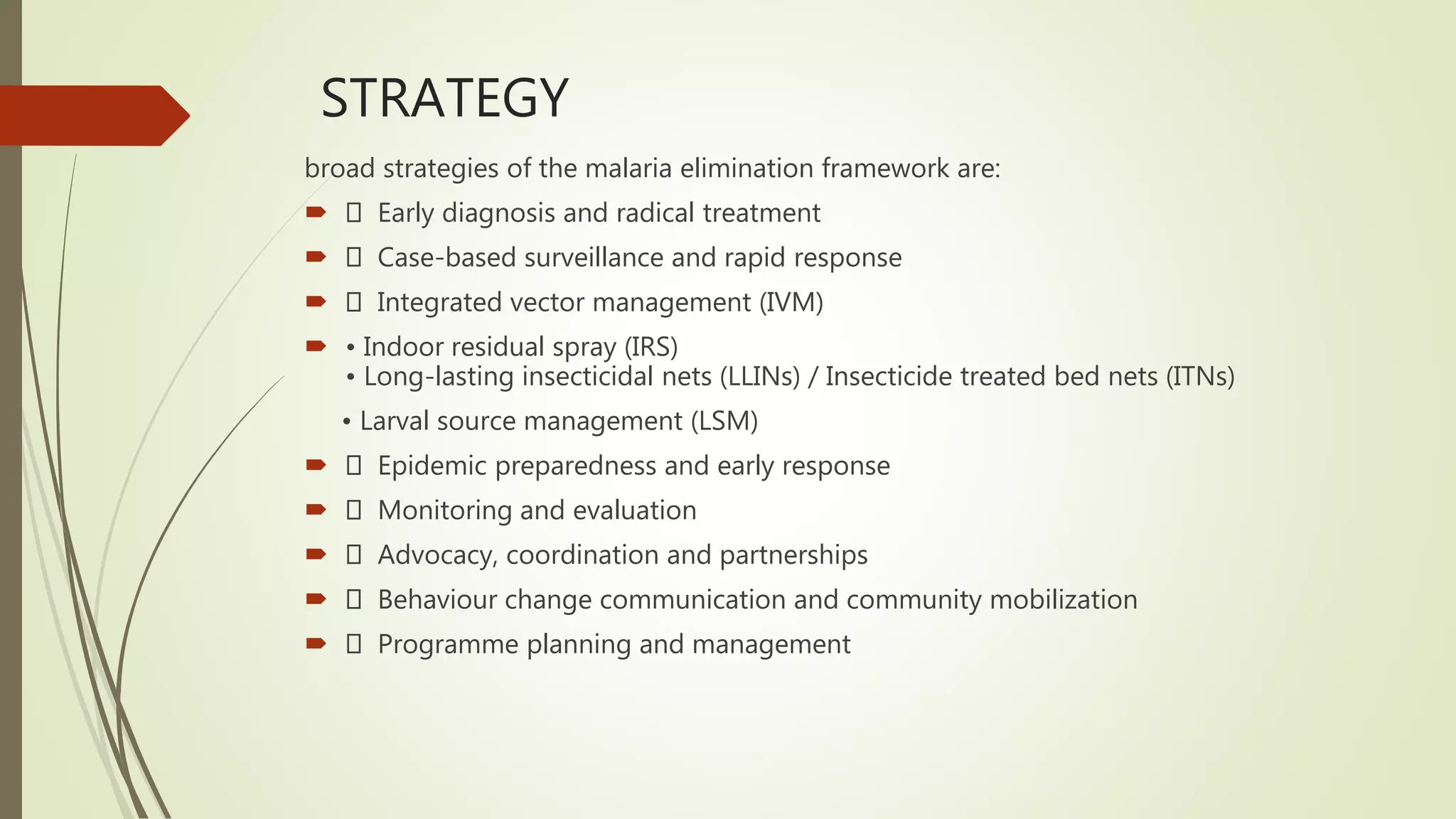
The National Vector Borne Disease Control Programme in India aims to combat six vector-borne diseases, notably malaria, dengue, and filariasis, with a focus on malaria eradication by 2030. The program includes policy formulation, technical guidance, training, and collaboration with international agencies to achieve its goals. Key milestones include interrupting malaria transmission, achieving zero indigenous cases, and implementing surveillance systems across various states and union territories.