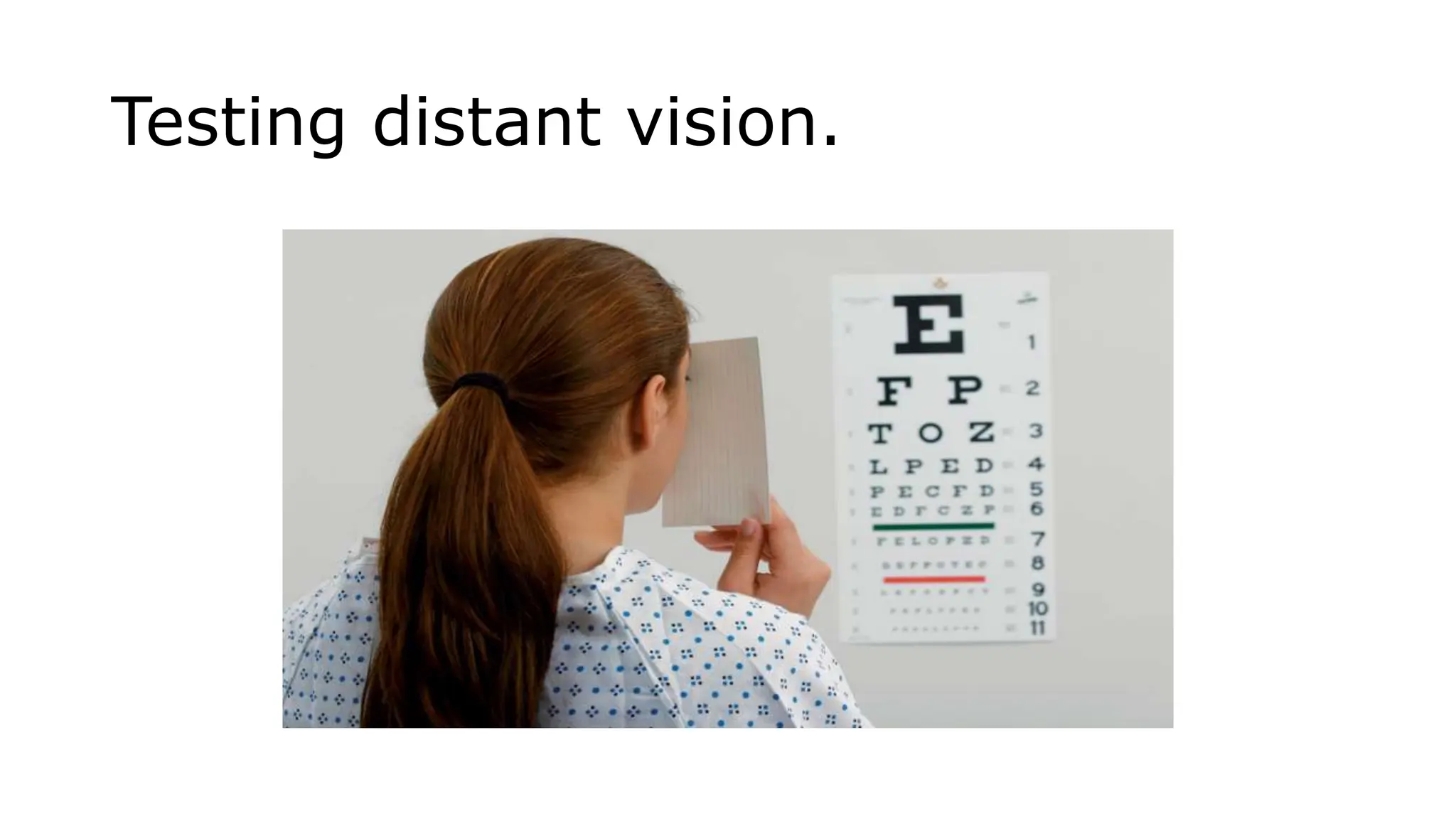
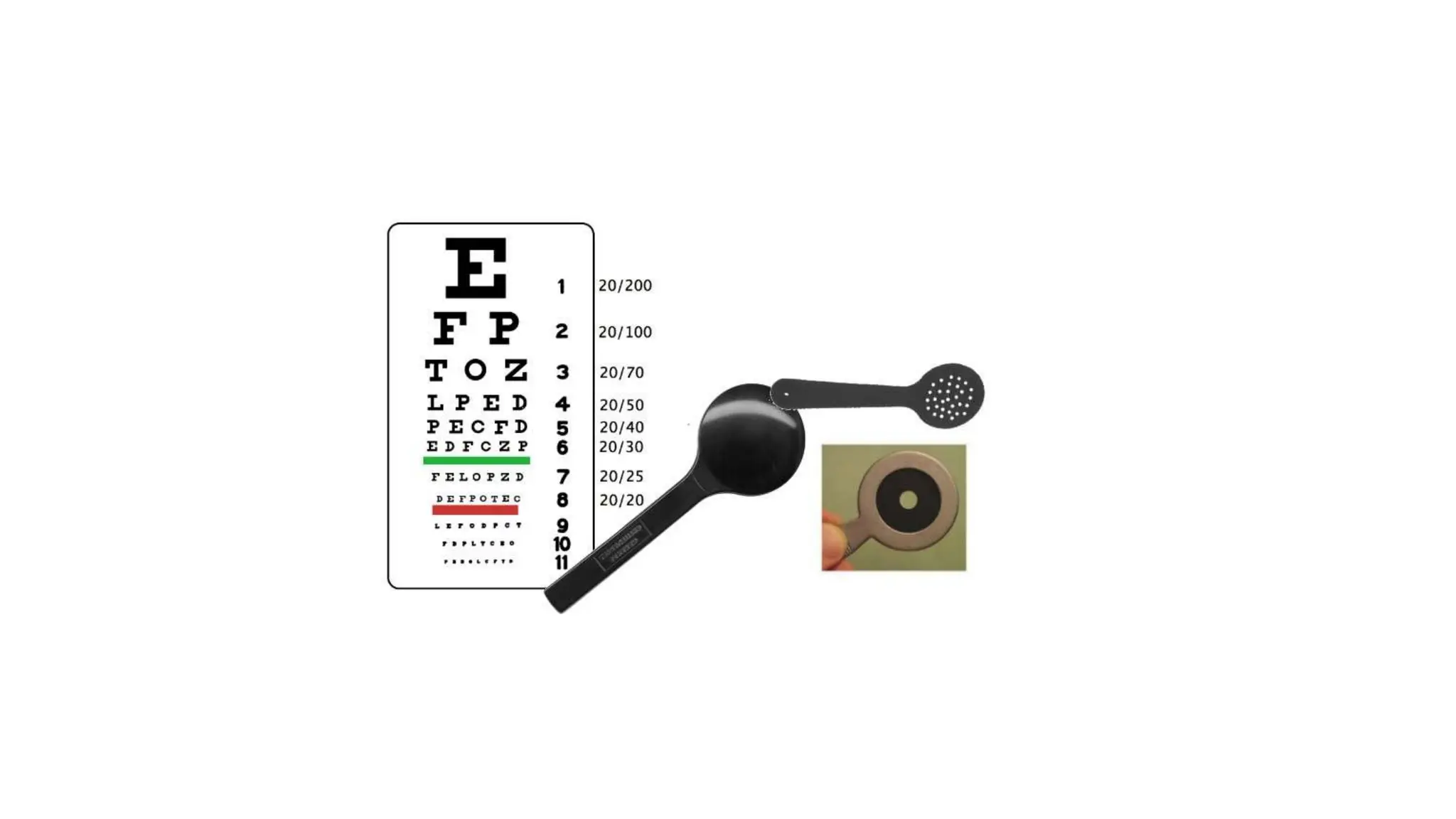
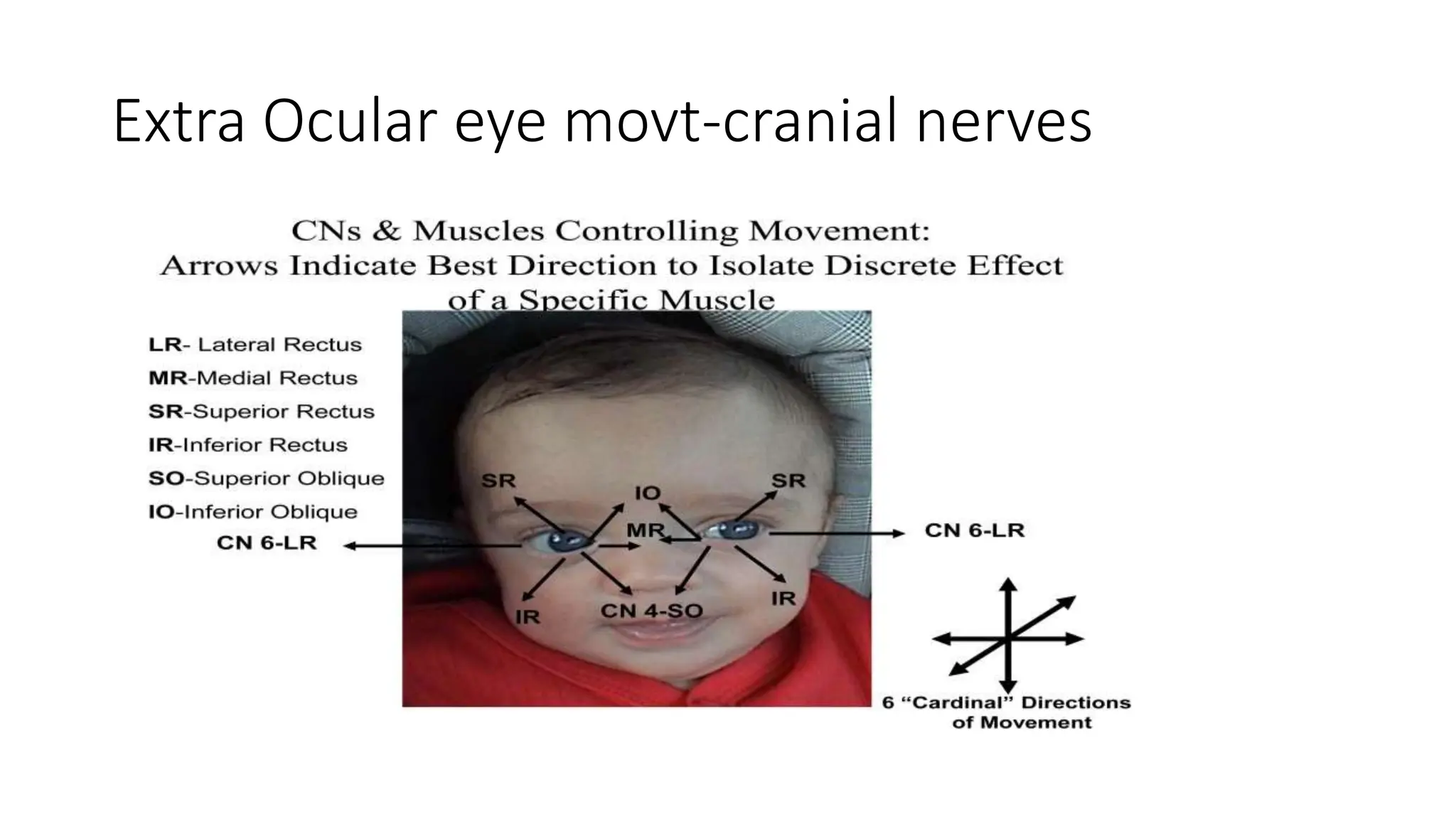
The document outlines a comprehensive eye examination process, focusing on assessing external eye structures, visual acuity, and extraocular movements. It details various tests like visual fields, pupillary responses, and the evaluation of internal eye structures to detect abnormalities. Emphasis is placed on interpreting findings related to cranial nerve function and potential vision impairments.