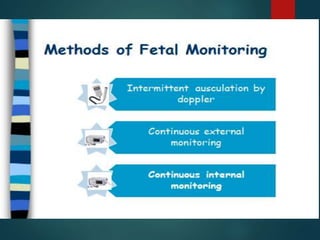
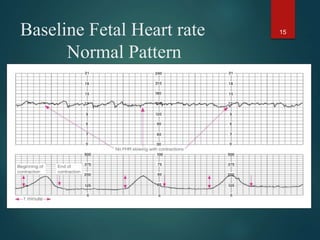
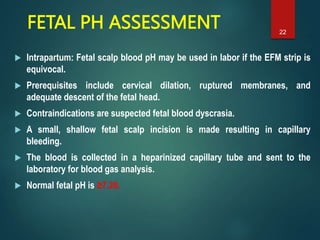
This document discusses intrapartum fetal heart rate monitoring. It defines normal and abnormal fetal heart rate patterns and categories. Category I indicates a normal tracing. Category II is indeterminate, while Category III tracings are abnormal, showing absent variability and late or variable decelerations. The document outlines intrauterine resuscitation measures to improve fetal oxygenation if abnormalities arise, such as giving oxygen, IV fluids, changing position and reducing contractions. Fetal scalp blood sampling to check pH can guide management in equivocal cases. Overall, the document provides guidance on interpreting and responding to fetal heart rate tracings during labor and delivery.