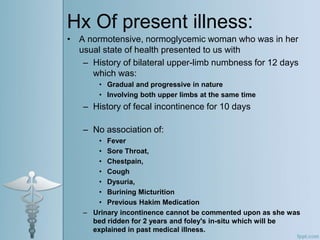
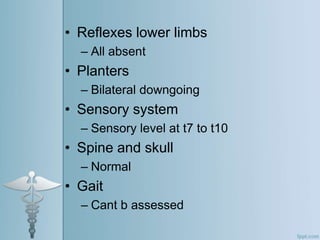
- A 36-year-old female presented with bilateral upper limb numbness and fecal incontinence. She had a history of multiple sclerosis diagnosed in 2015, with recurrent episodes of lower limb weakness.
- MRI of the cervical spine showed hyperintense lesions in 2017 and cord atrophy in 2021. AQP4 antibodies were positive, confirming a diagnosis of neuromyelitis optica spectrum disorder (NMOSD).
- NMOSD is an autoimmune condition targeting the aquaporin-4 protein. It is characterized by optic neuritis and transverse myelitis, and differs from multiple sclerosis in presentation and treatment approach.