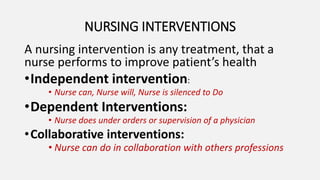
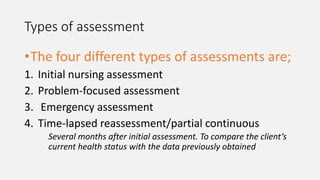
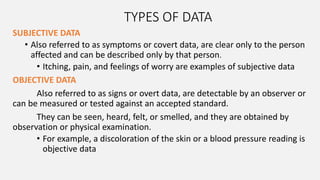
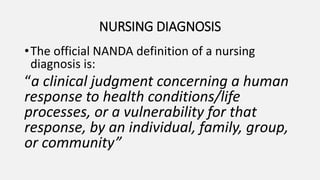
The nursing process is a systematic and critical thinking method used by nurses to provide individualized care and address client health needs through assessment, diagnosis, planning, implementation, and evaluation. This process includes various types of assessments, diagnoses based on client responses, and strategic planning for interventions. The nursing diagnosis differs from medical diagnosis as it focuses on human responses to health issues, guiding nurses in effective care management.












![Formulating Diagnostic Statements
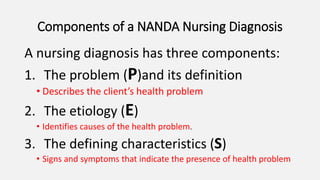
The Nursing diagnosis = P+E+S
PROBLEM [P] Etiology [E] Evidence (defining
characteristics)
ACUTE ABDOMINAL PAIN
Acute inflammation of the
appendix,
• Guarding
• Patient assuming a bent
position to relieve the
pain
• Patient verbalizing a
9/10 pain scale
• Flushed patient face
• Patient sighing](https://image.slidesharecdn.com/thenursingprocess-220918073733-553189e0/85/THE-Nursing-process-1-3-pptx-18-320.jpg)