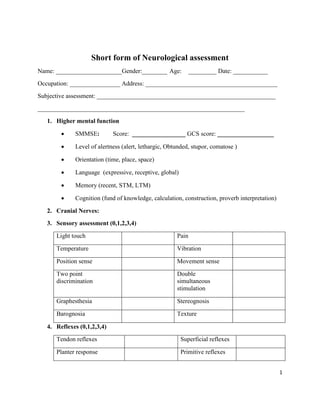
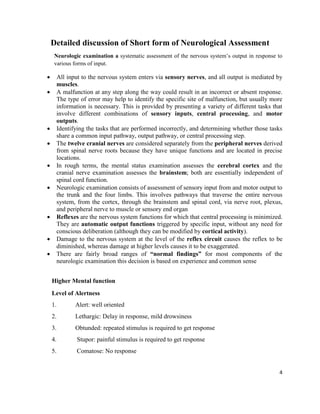
This document provides a template for conducting a short neurological assessment. It includes sections to document subjective information, assess higher mental functions like orientation and memory, examine the 12 cranial nerves, perform sensory and motor testing, evaluate reflexes, coordination, gait, and balance. Specific tests are outlined to assess functions like vision, hearing, facial strength and sensation. The assessment also includes objective tests of functional movements and special tests as needed. The goal is to systematically evaluate the nervous system's input and output through sensory, motor and cognitive tasks.






![10
the contralateral extremity. This second approach, however, is impractical with proximal
lower extremity joints, owing to potential stress on the low back. During testing, movement
of larger joints is usually discerned more quickly than that of smaller joints. The therapist’s
grip should remain constant and minimal (fingertip grip over bony prominences), to reduce
tactile stimulation.
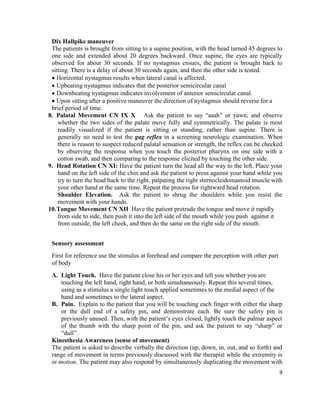
Proprioceptive Awareness (sense of position)
While the extremity or joint(s) is held in a static position by the therapist, the patient is
asked to describe the position verbally or to duplicate the position of the extremity or
joint(s) with the contralateral extremity (position matching). His test may also be
performed unilaterally using the same extremity or joint(s); first held in position by the
examiner, then returned to resting position, followed by active duplication of position by
patient using the same limb.
C. Vibration. Tap a 128 Hz tuning fork lightly against a solid surface to produce a slight
vibration. With the patient’s eyes closed, hold the non-vibrating end of the tuning fork
firmly on the DIP joint of the patient’s left thumb, and ask the patient if the vibration is
detectable. Let the vibration fade until the patient no longer detects it, then apply the tuning
fork to your own thumb to see if you can still feel any vibration. Repeat this testing on the
patient’s right thumb and both great toes
Two point discrimination
This test determines the ability to perceive two points applied to the skin simultaneously. It
is a measure of the smallest distance between two stimuli (applied simultaneously and with
equal pressure) that can still be perceived as two distinct stimuli. Two-point discrimination
values vary for different individuals and body parts.
Double Simultaneous Stimulation
This test determines the ability to perceive simultaneous touch stimuli (double
simultaneous stimulation [DSS]). The therapist simultaneously (and with equal pressure)
touches: (1) identical locations on opposite sides of the body, (2) proximally and distally on
opposite sides of the body, and/or (3) proximal and distal locations on the same side of the
body. he term extinction phenomenon is used to describe a situation in which only the
proximal stimulus is perceived, with “extinction” of the distal.
D. Graphesthesia. Ask the patient to close the eyes and identify a number from 0 to 9 that
you draw on his or her index finger using a ballpoint pen. Repeat with several other
numbers, and compare to the other hand. Perform analogous testing on the feet, but your
drawing may need to be larger there.
E. Stereognosis. Ask the patient to close the eyes and identify a small object (e.g., nickel,
dime, quarter, penny, key, paper clip) you place in his or her right hand. Test the left hand
in the same way.](https://image.slidesharecdn.com/generalneuroassessment-231029092913-d8e38143/85/General-Neuro-Assessment-pdf-10-320.jpg)