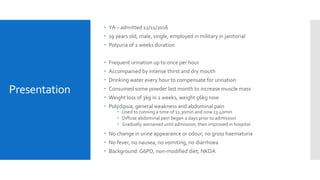
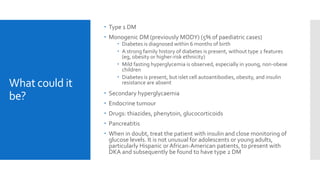
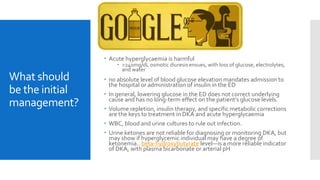
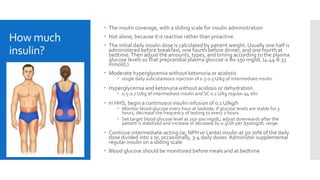
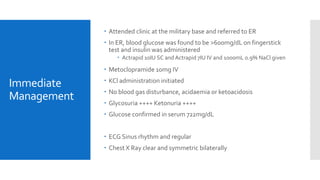
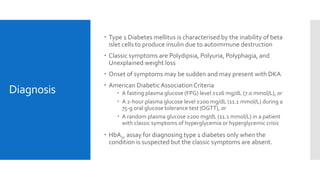
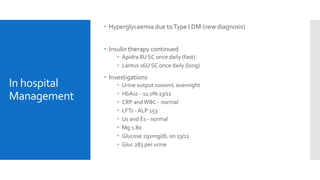
The document details the case study of a 19-year-old male diagnosed with type 1 diabetes mellitus, highlighting symptoms such as polyuria, polydipsia, and weight loss, alongside his medical history. It outlines the management plan, including insulin therapy, blood glucose monitoring, and dietary education, while emphasizing the need for close follow-up and patient education to prevent complications. The report stresses the importance of achieving tight glycemic control to minimize the risk of microvascular and macrovascular issues associated with diabetes.