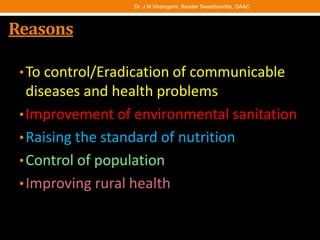
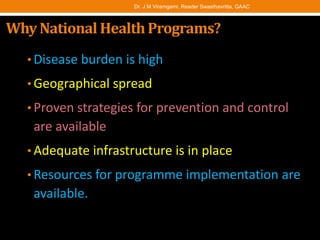
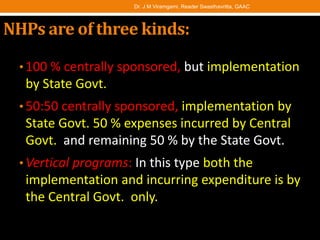
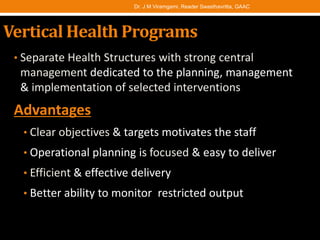
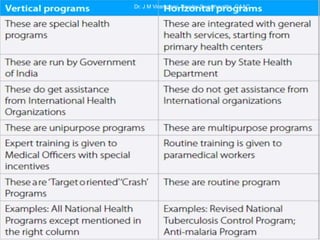
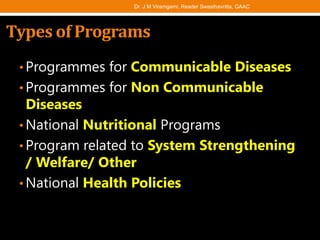
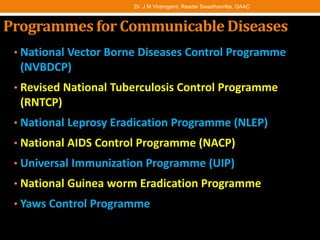
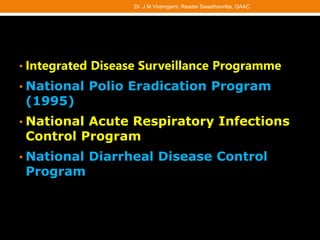
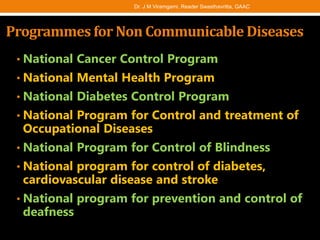
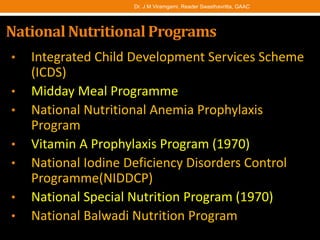
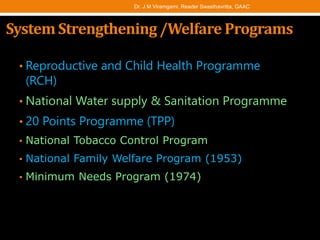
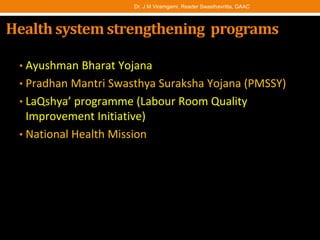
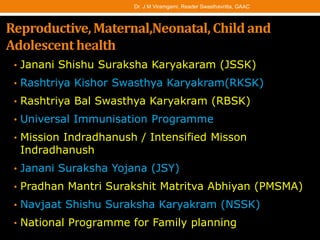
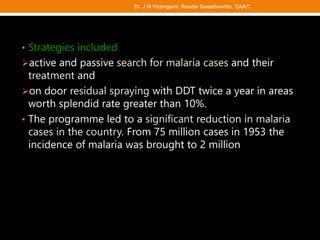
The document provides an overview of national health programs in India. It discusses how various programs were launched after India gained independence to improve public health and control diseases. The programs are of three types - fully funded by central government, jointly funded by central and state governments, and vertical programs fully run by central government. The document outlines numerous programs targeting communicable diseases, non-communicable diseases, nutrition, and health system strengthening. It provides details on strategies for key programs like National Vector Borne Diseases Control Programme and National filarial control program.