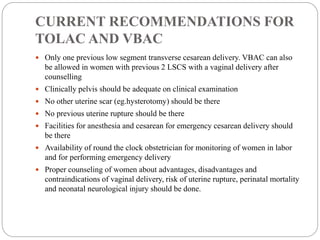
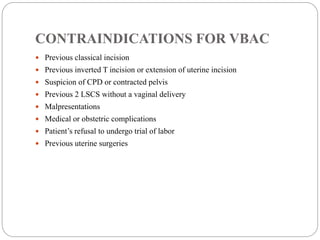
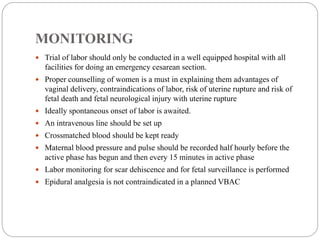
This document provides recommendations and guidelines for vaginal birth after cesarean (VBAC). It outlines that VBAC can be allowed for women with one previous low transverse cesarean incision as long as the pelvis is adequately sized and there are no other uterine scars or previous uterine ruptures. Facilities for emergency cesarean delivery and 24/7 obstetrician availability are required. Women should be properly counseled on risks and monitored closely during a trial of labor, which should only occur in a well-equipped hospital. Risks include an unsuccessful vaginal delivery, scar dehiscence or rupture, and associated maternal and perinatal morbidity.