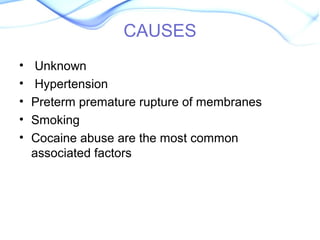
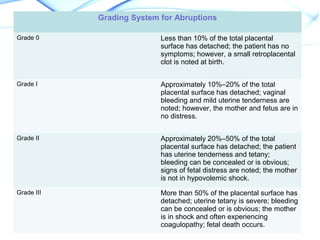
Abruptio placentae is the premature separation of the placenta from the uterus prior to delivery. It is characterized by vaginal bleeding, uterine tenderness, and fetal distress. Risk factors include hypertension, smoking, cocaine use, trauma, and short umbilical cord. Diagnosis is based on clinical symptoms and examination of the placenta after delivery. Treatment depends on severity but may include bed rest, monitoring, blood transfusions, and emergency cesarean section if the mother or baby show signs of distress.