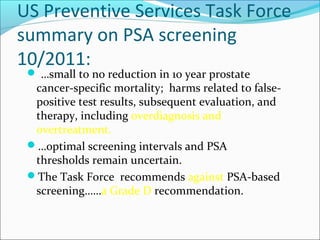
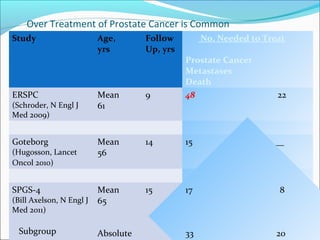
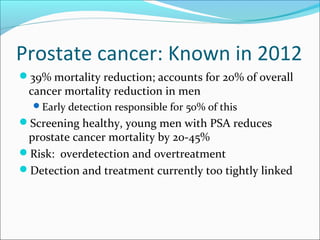
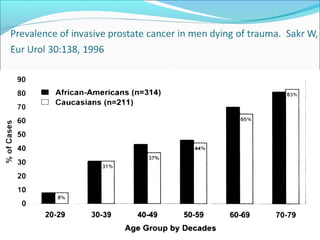
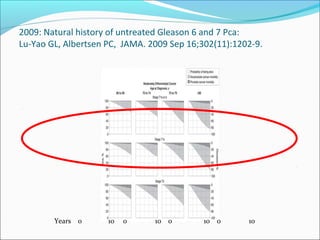
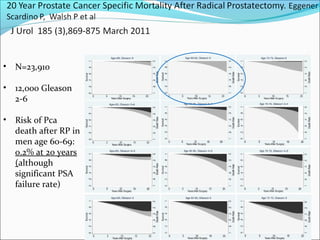
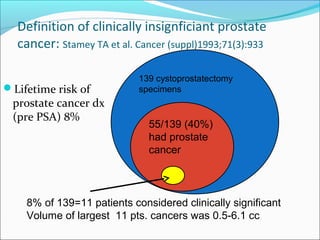
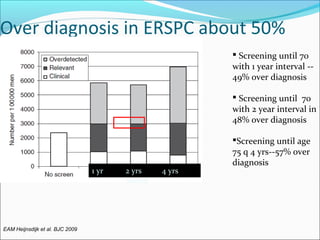
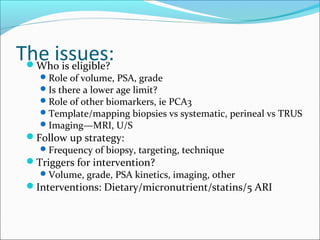
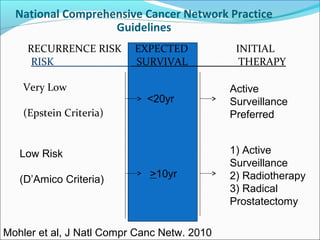
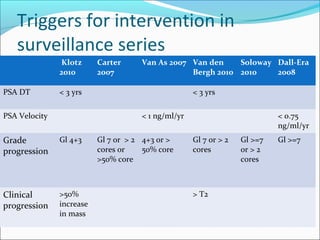
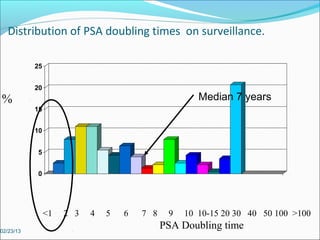
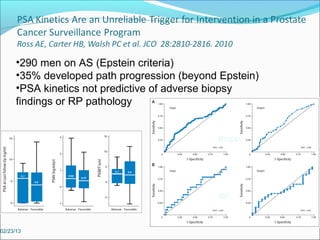
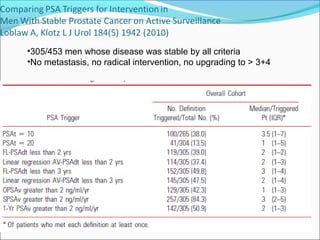
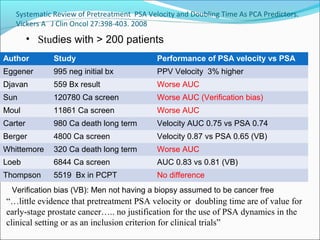
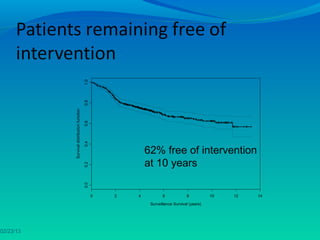
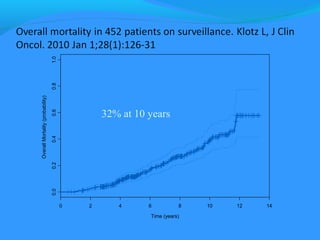
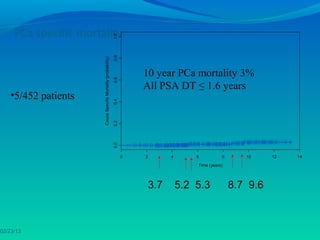
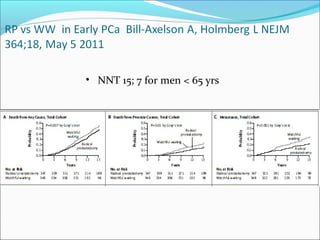
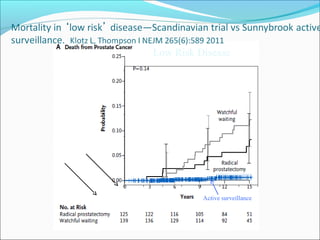
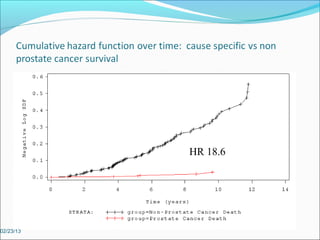
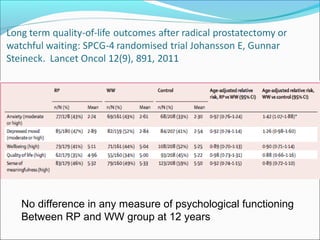
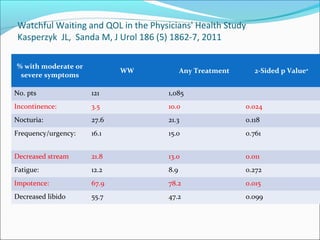
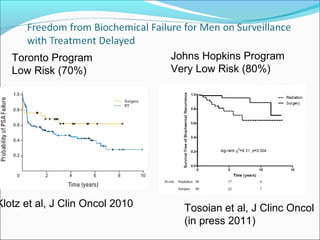
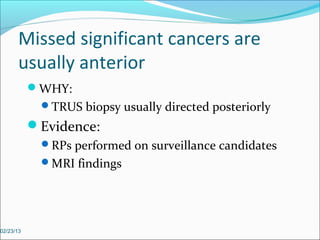
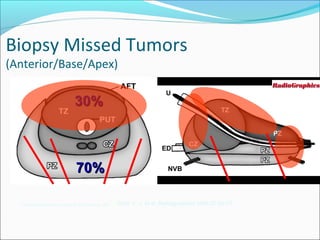
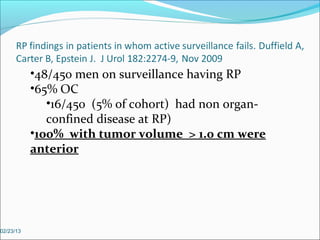
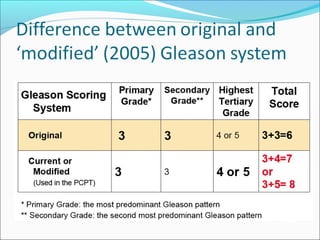
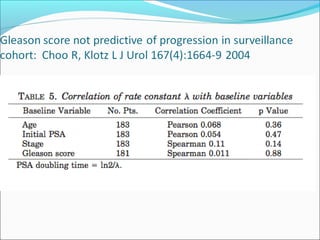
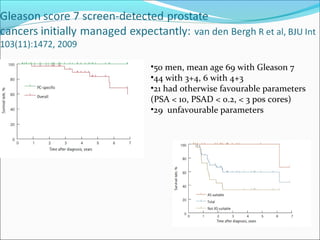
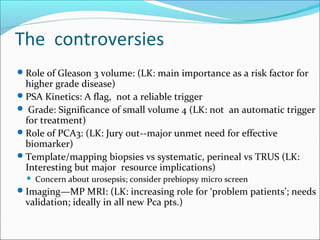
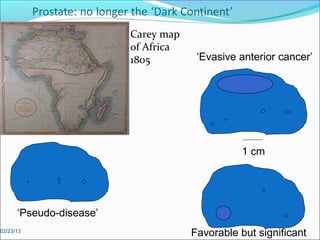
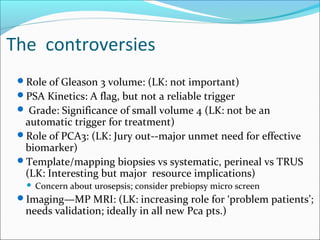
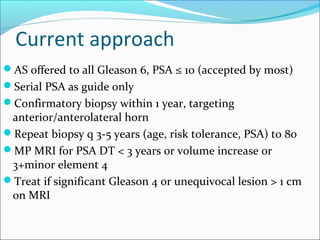
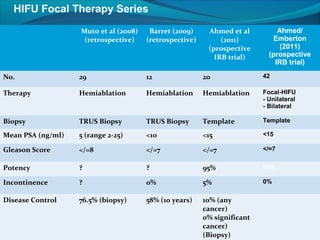
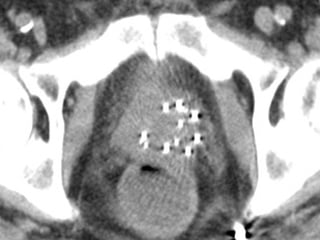
This document discusses the management of low risk prostate cancer. It outlines the natural history of untreated low risk prostate cancer and the problems of overdiagnosis and overtreatment. Active surveillance is presented as a management option for low risk prostate cancer, with the rationale being to avoid unnecessary treatment and preserve quality of life. Results from active surveillance studies show low rates of cancer progression and metastasis, with 62% free from intervention at 10 years in one study. Triggers for intervention on active surveillance like rising PSA, grade progression, or tumor volume increase are discussed.