1. The lacrimal system includes the secretory portion which produces tears and the drainage system which drains tears from the eye into the nasal cavity.
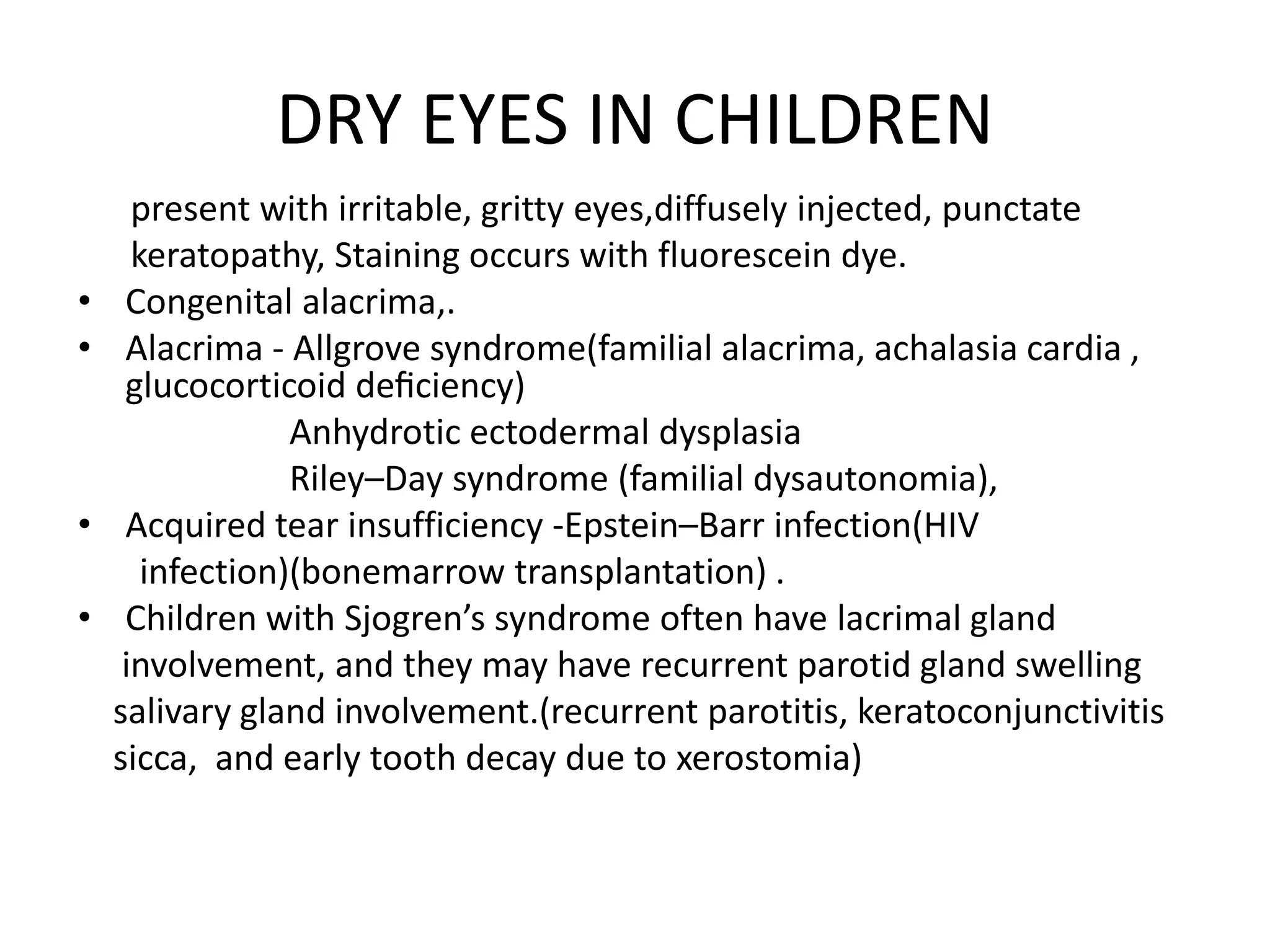
2. Common lacrimal disorders in children include dry eyes, tumors/granulomas of the lacrimal gland, congenital nasolacrimal duct obstruction, and congenital or acquired abnormalities of the puncta and canaliculi.
3. Congenital nasolacrimal duct obstruction is treated initially with observation but older children may require probing or dacryocystorhinostomy to resolve persistent epiphora. Acquired nasolacrimal duct obstruction can result from trauma, infection, or inflammation.





![LACRIMAL TUMOURS& GRANULOMAS
• Orbital‘pseudotumour’ (now idiopathic orbital
inflammatory disease)- painful swelling-responds to
steroids
• Malignant epithelial tumours including mixed-cell
adenocystic
• Lacrimal gland enlargement –sarcoidosis
&leukaemia.
• Dacrocystocoele - congenital swelling located at
medial canthus d/t trapped fluid inside the lacrimal
sac & NLD. [tense, blue, non-pulsatile swelling
below the medial canthus seen at birth]](https://image.slidesharecdn.com/lacrimaldisordersinchildrencopy-201112183547/75/Lacrimal-disorders-in-children-7-2048.jpg)









