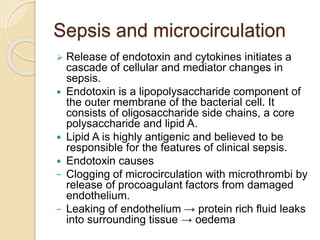
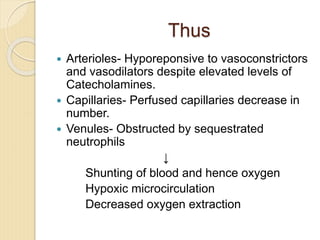
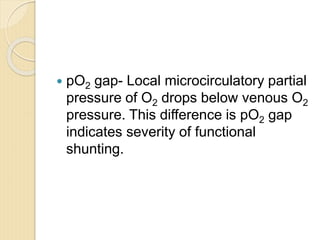
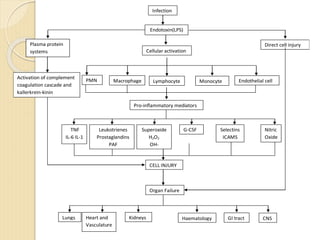
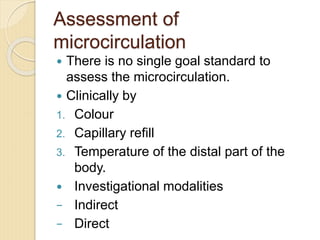
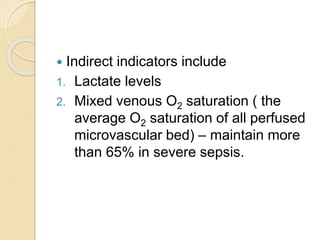
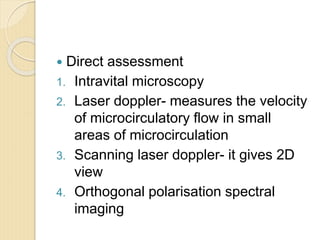
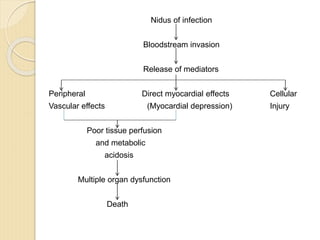
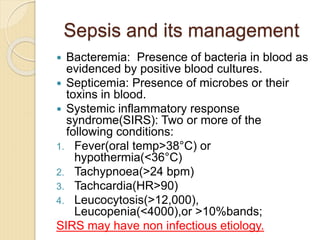
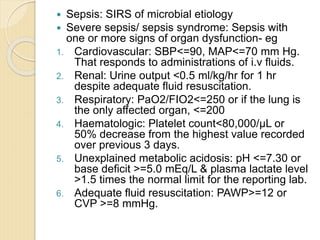
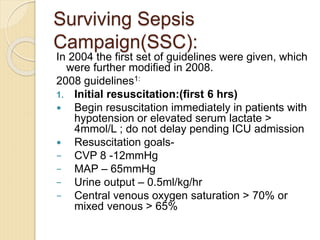
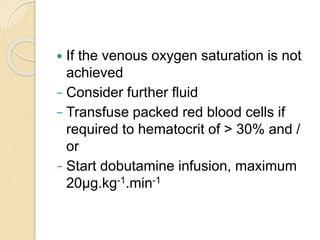
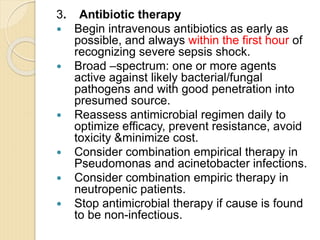
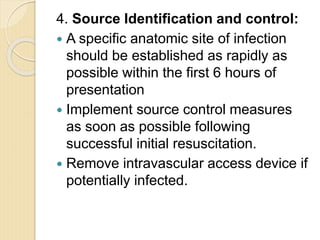
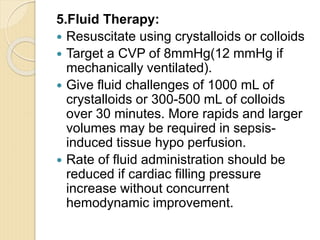
The microcirculation consists of resistance vessels (arterioles), exchange vessels (capillaries), and capacitance vessels (venules). Capillary recruitment increases exchange surface area to meet metabolic demands. In sepsis, endotoxin and cytokines cause endothelial damage, microthrombi formation, increased viscosity, and hyporesponsiveness of arterioles. This decreases perfused capillaries and increases shunting, resulting in tissue hypoxia. Direct assessment methods include intravital microscopy and laser doppler, while indirect indicators include lactate and mixed venous oxygen saturation. Timely management of sepsis per Surviving Sepsis Campaign guidelines focuses on early resuscitation, diagnosis, antibiotics, source control, fluids, vasop