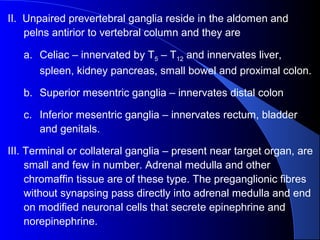
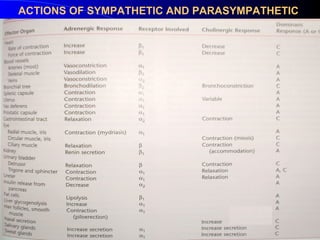
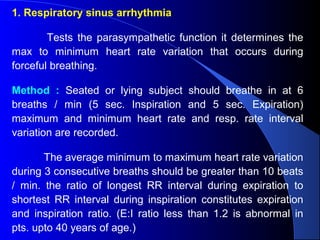
The document discusses the anatomy and physiology of the autonomic nervous system. It begins by describing the autonomic nervous system's organization based on reflex arcs between receptors, the central nervous system, and effectors. It then discusses the sympathetic and parasympathetic nervous systems in detail, including their anatomy, neurotransmitters, and receptors. Finally, it outlines some common tests used to evaluate autonomic integrity, such as tests of cardiac vagal function like respiratory sinus arrhythmia and tests of sympathetic function like postural stress responses and cold pressor tests.