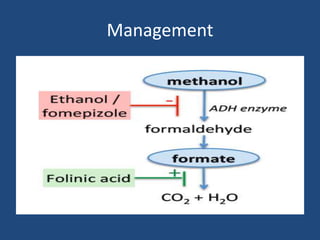
1) Methanol is toxic to humans when ingested and is sometimes used as an ethanol substitute by alcoholics. It is metabolized to formaldehyde and formic acid which cause metabolic acidosis, blindness, and can be fatal.
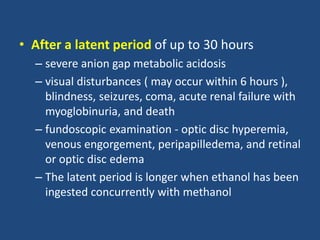
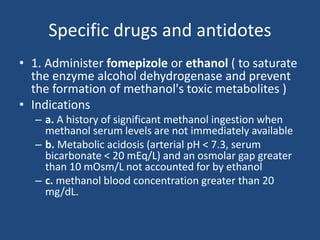
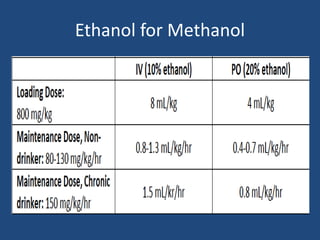
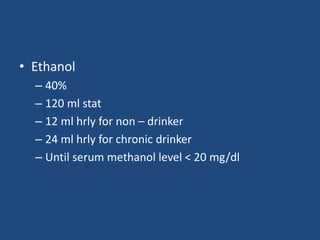
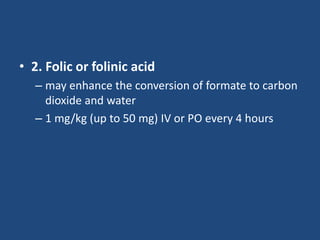
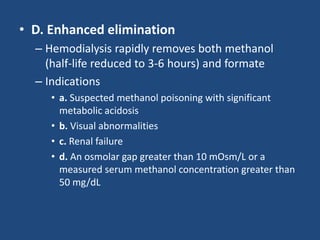
2) The toxic effects of methanol occur after a latent period of 30 hours as it is slowly metabolized. Symptoms include vision loss, seizures, coma and death. Treatment focuses on preventing further metabolism using fomepizole or ethanol and enhancing excretion through hemodialysis.
3) Diagnosis is based on history of ingestion and laboratory findings showing a large osmolar or anion gap metabolic acidosis. Levels of methanol, formate or a