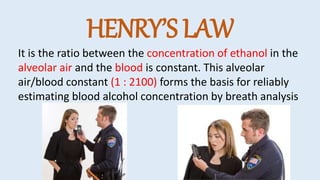
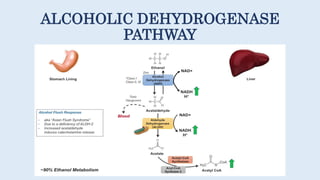
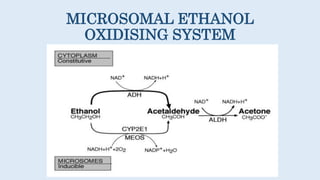
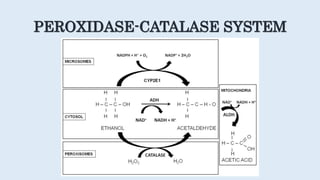
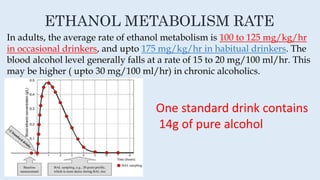
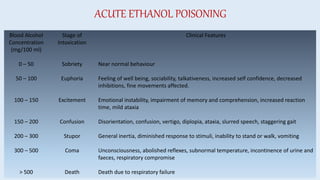
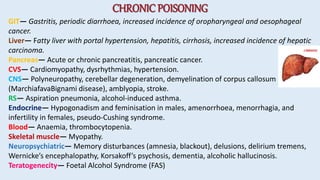
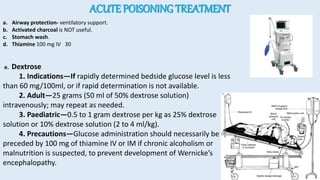
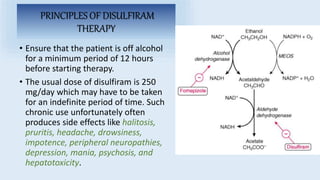
This document discusses alcohol poisoning and the effects of ethanol. It covers the categories of alcohols, ethanol uses including as a beverage and in medicine, toxicokinetics of ethanol absorption and metabolism, mechanisms of action on the body, acute and chronic poisoning symptoms, and treatment approaches for alcohol poisoning and chronic alcoholism.