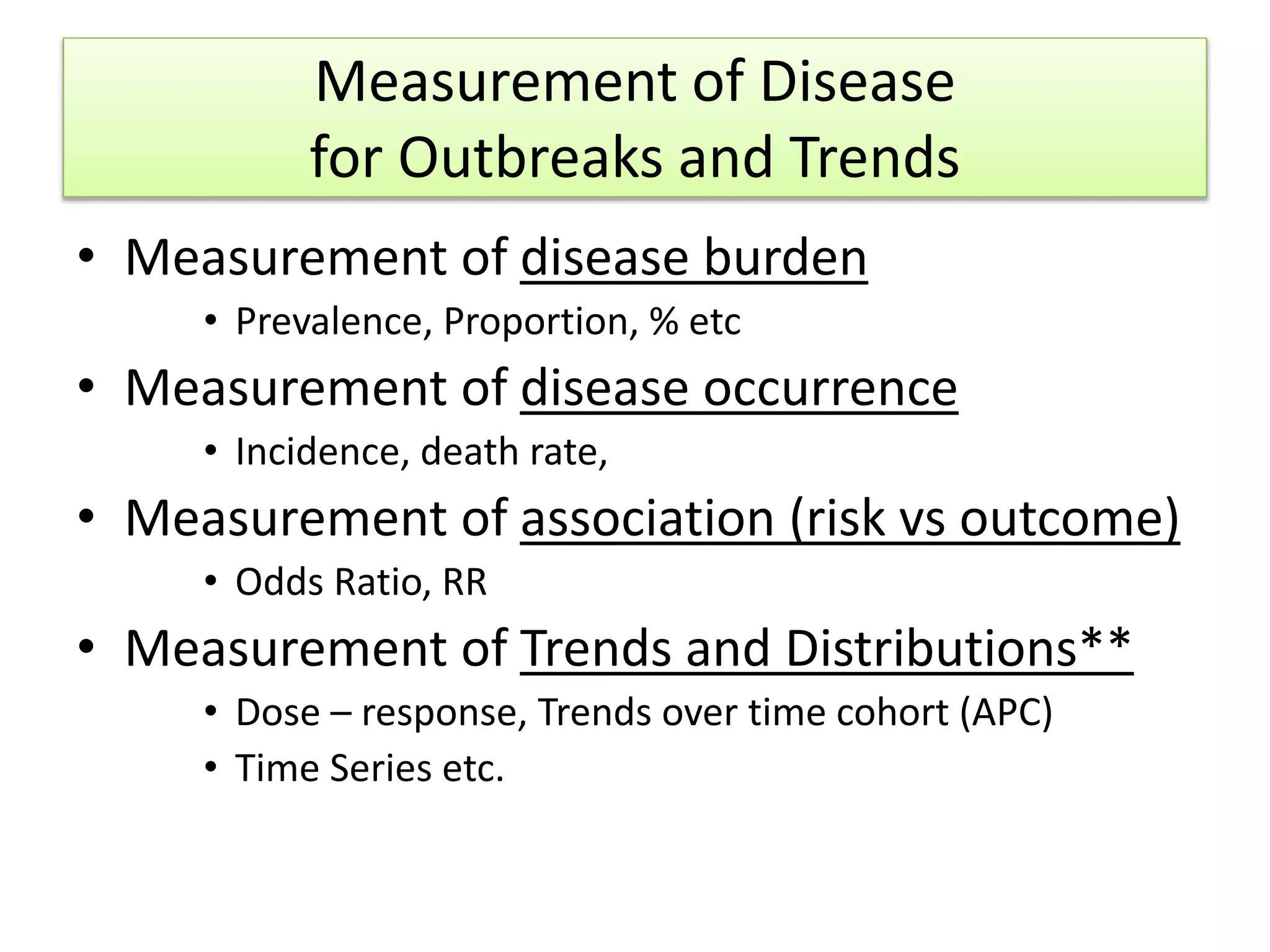
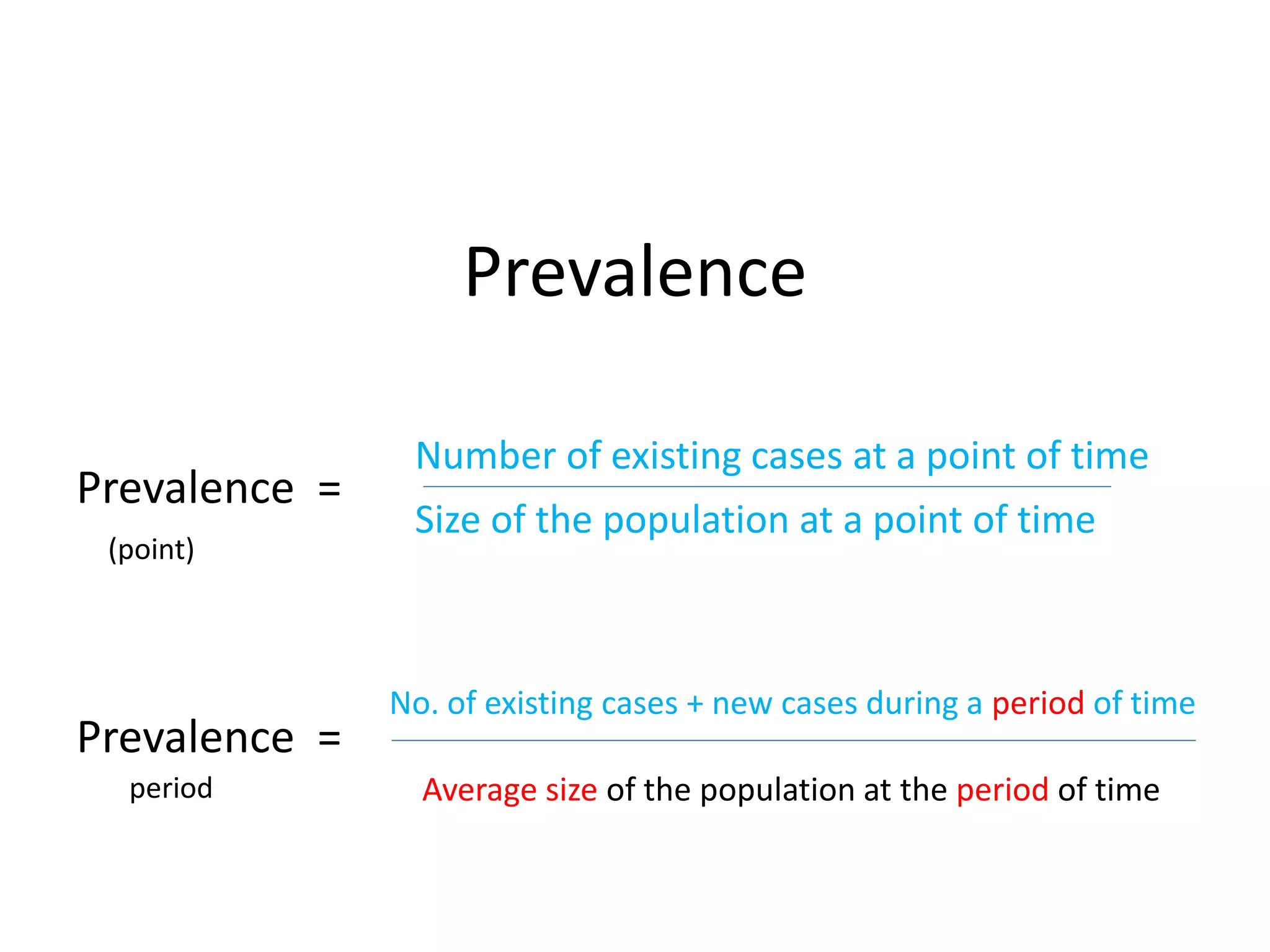
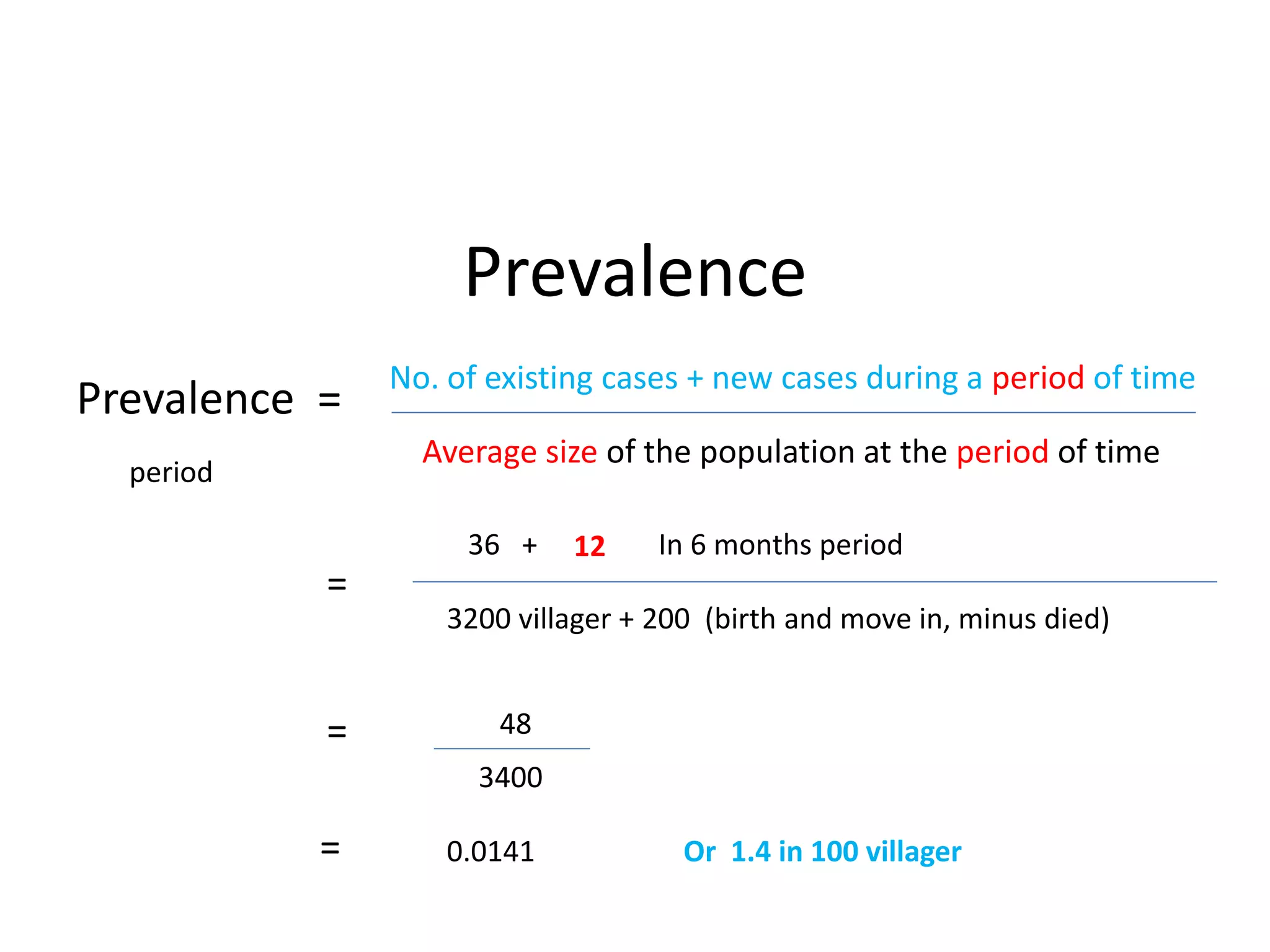
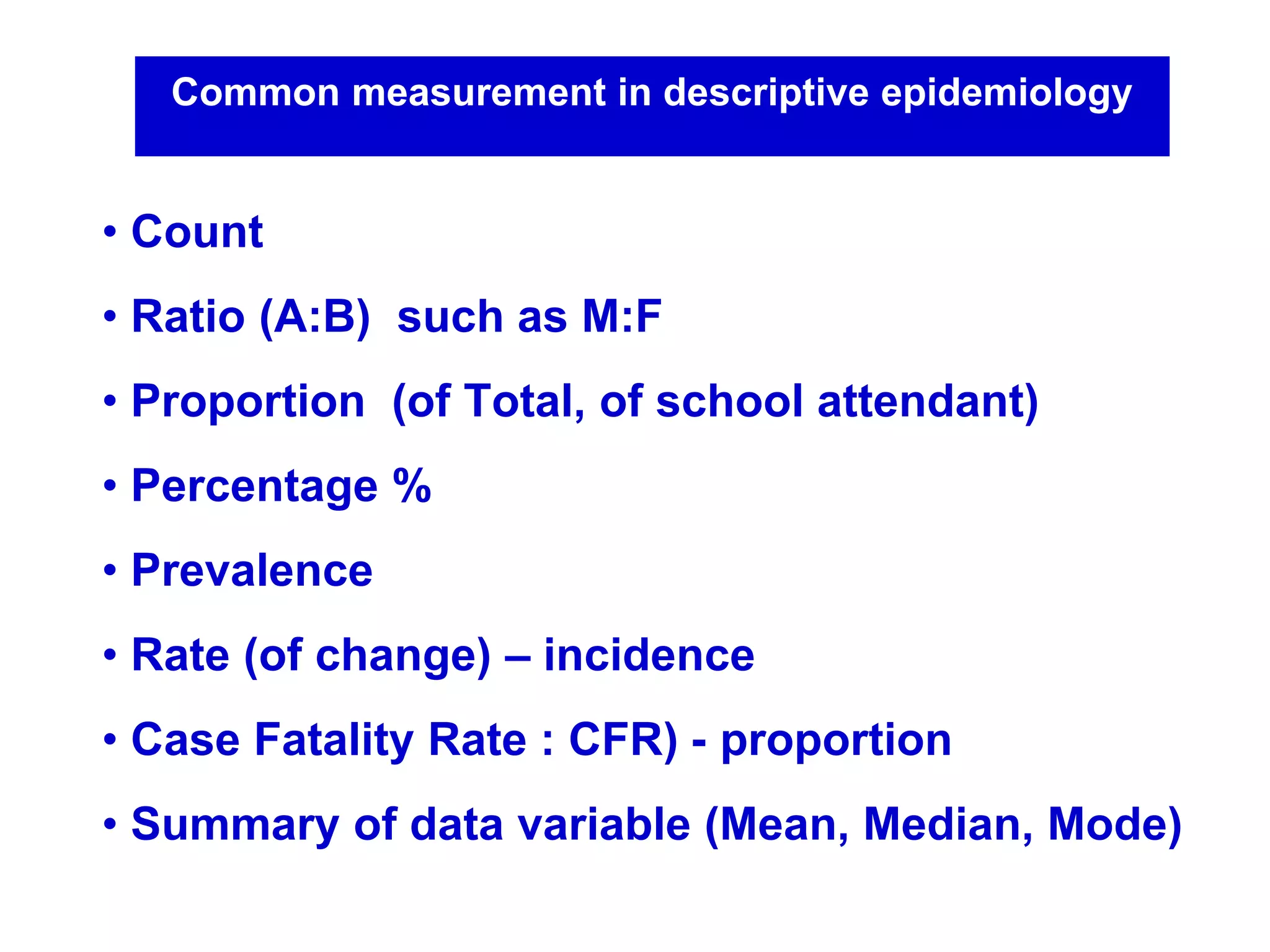
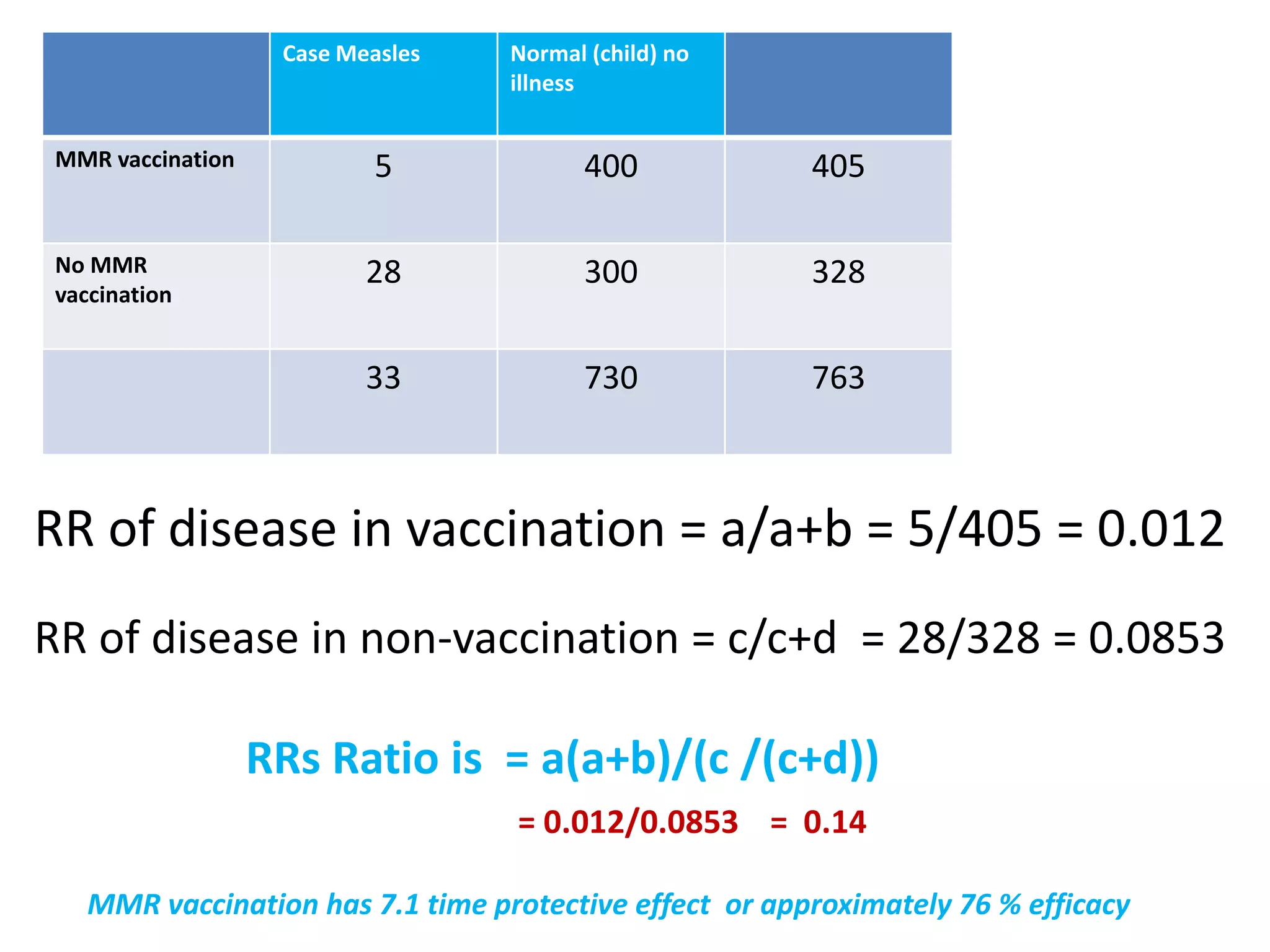
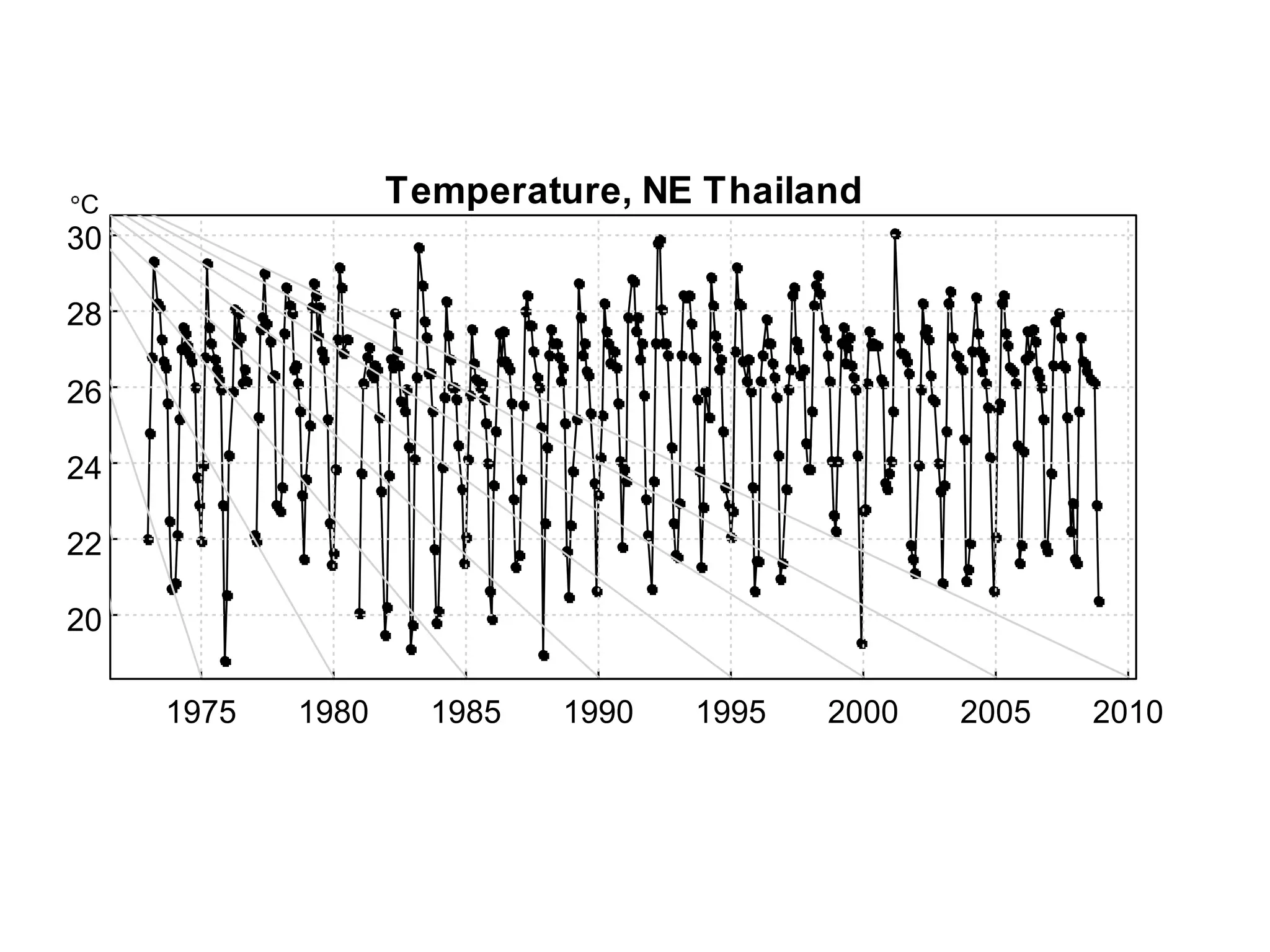
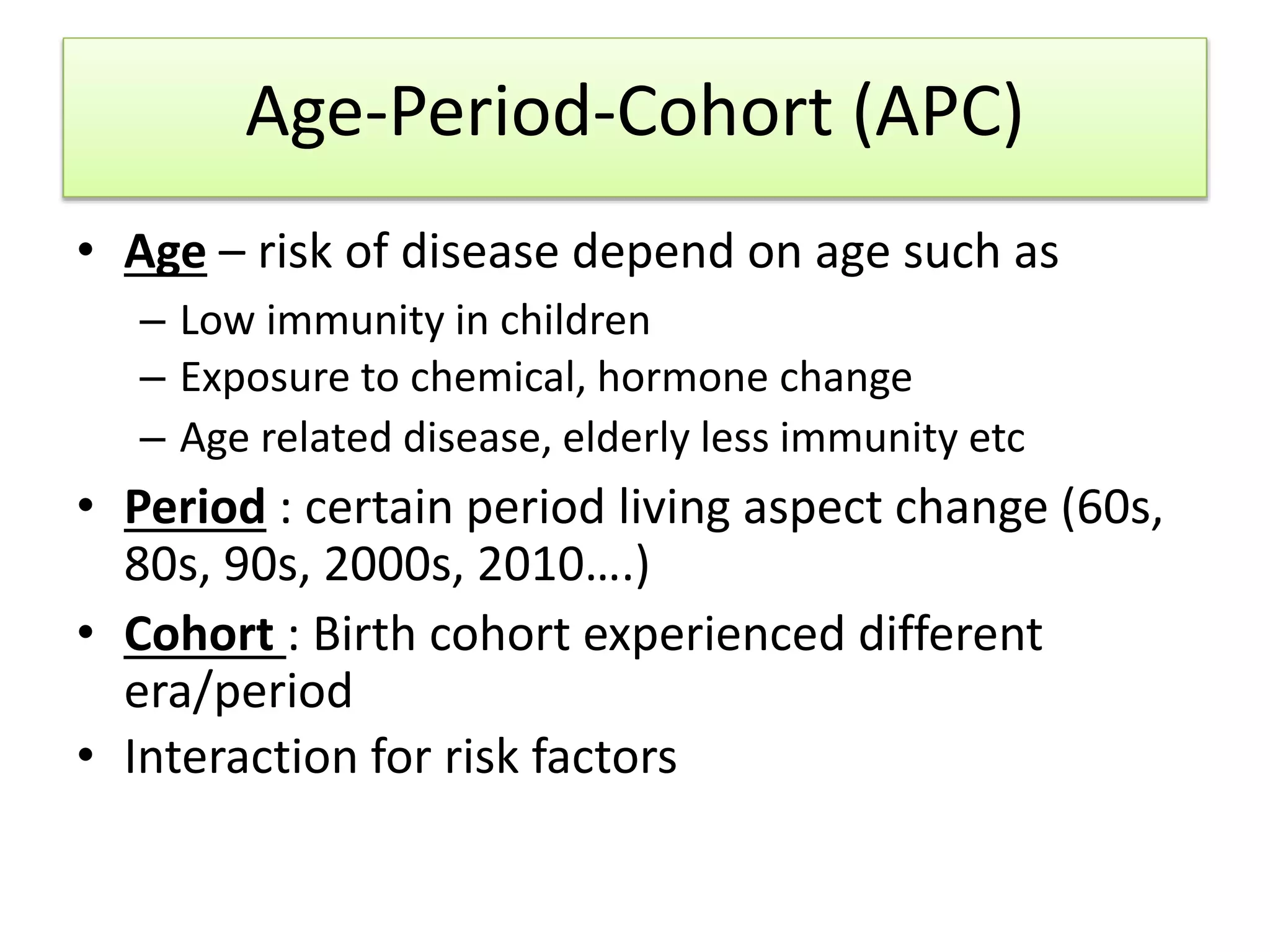
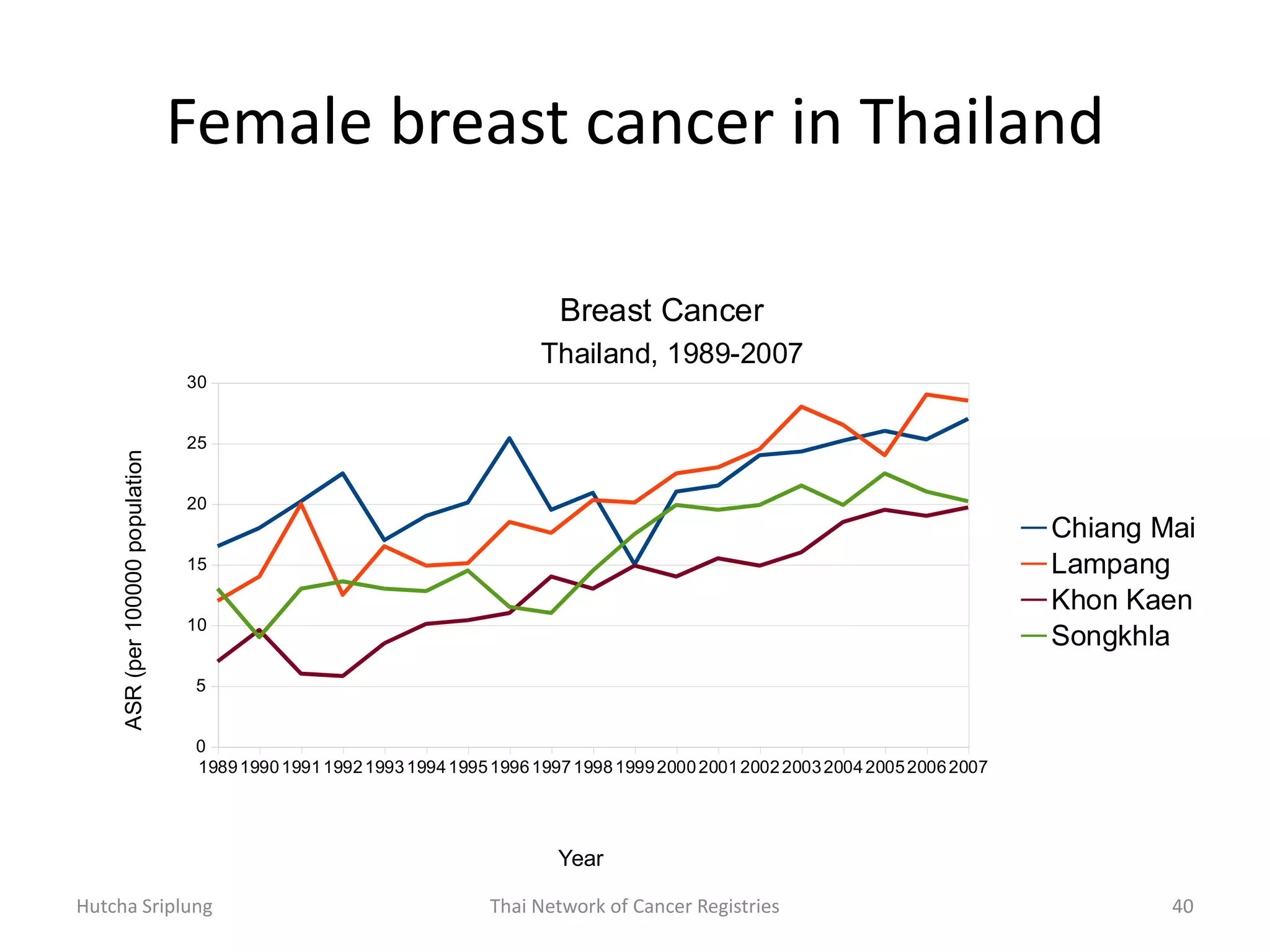
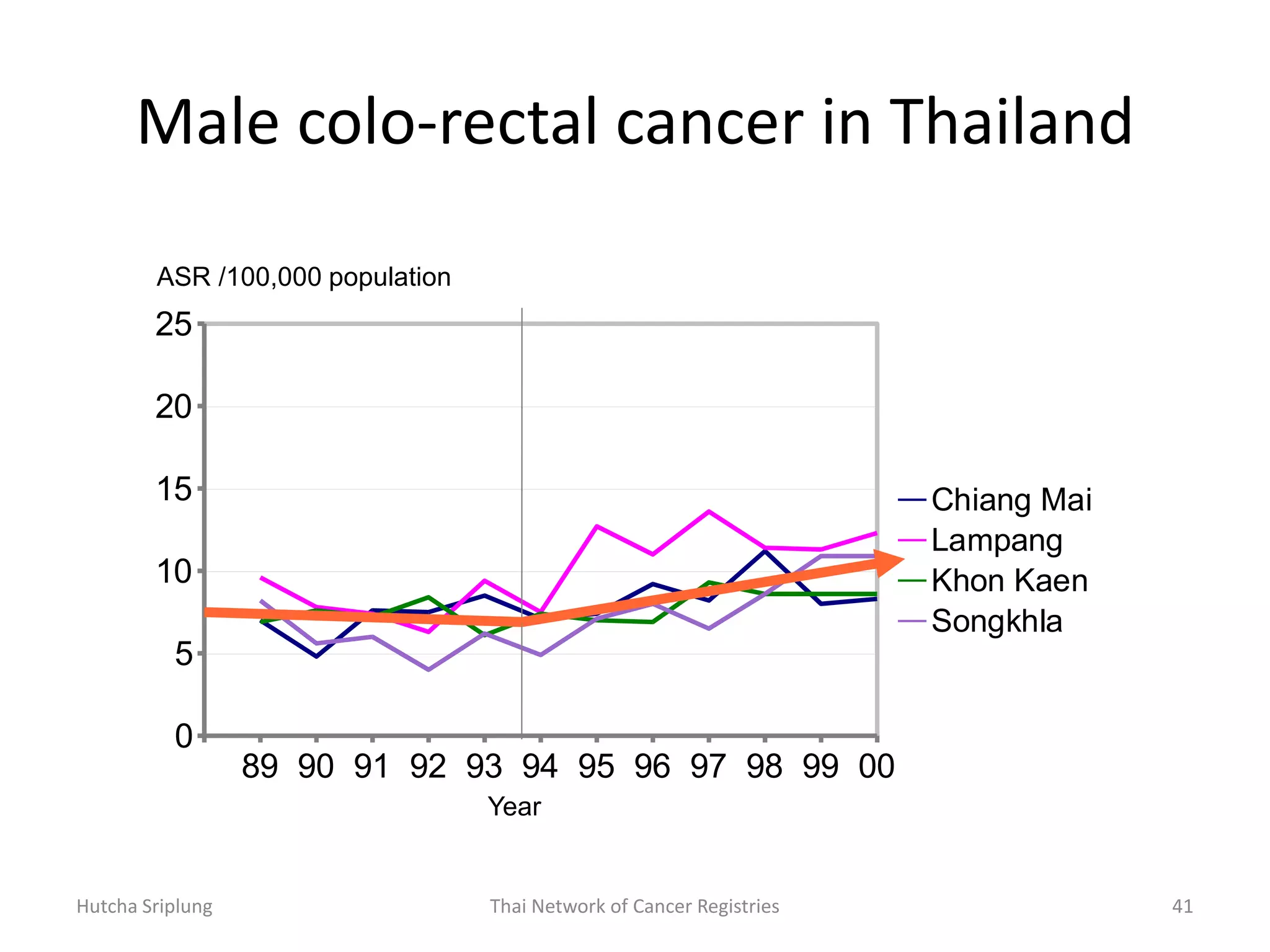
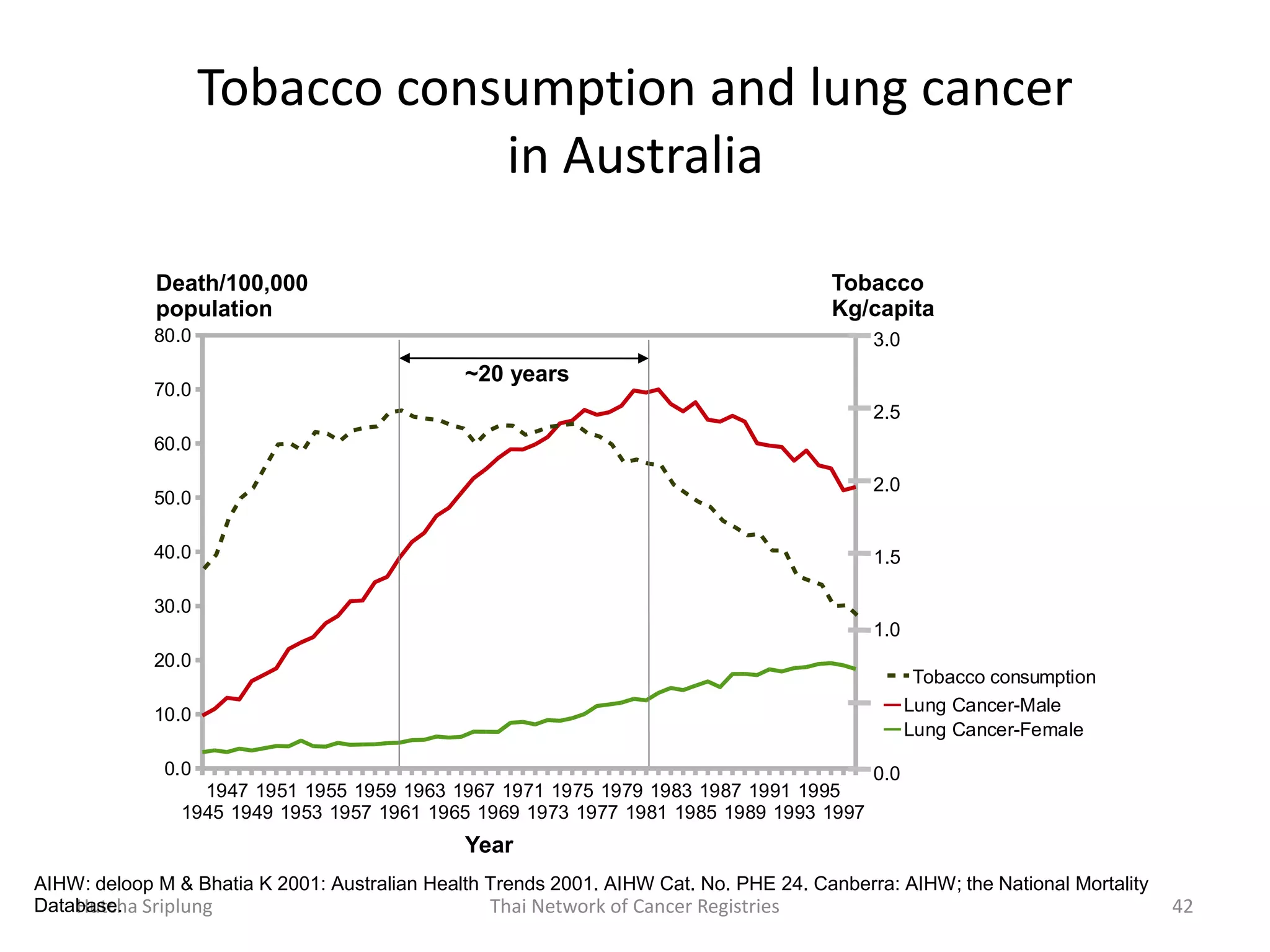
This document discusses various methods for measuring disease frequency and trends. It defines key epidemiological terms like prevalence, incidence, odds ratio, and relative risk. It explains how to calculate these measures and interpret them. For example, it shows how to calculate the odds ratio from a 2x2 table to measure the association between alcohol use and accidents. It also discusses factors that can indicate a causal relationship and gives examples of time series analysis of disease trends over time.