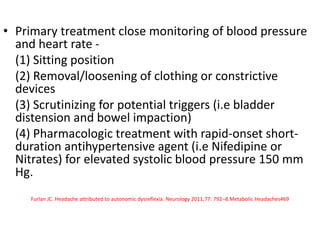
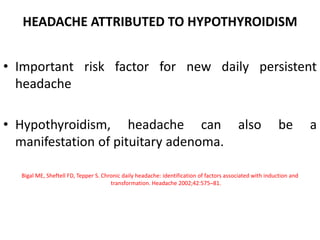
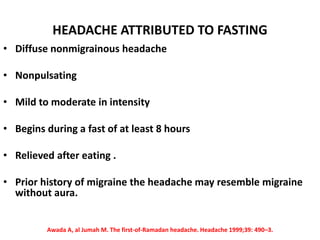
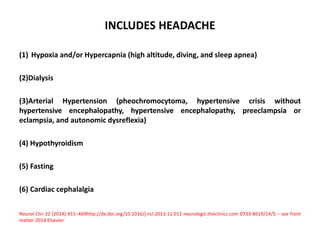
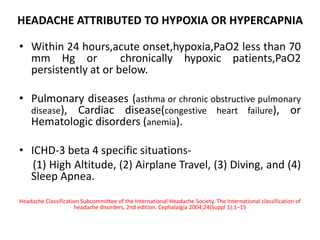
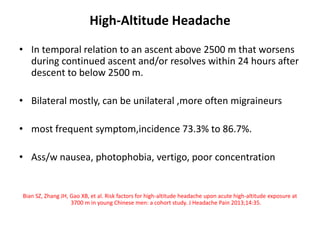
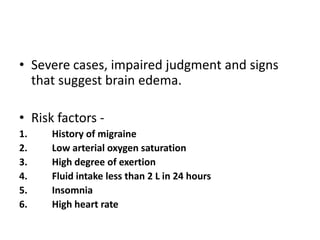
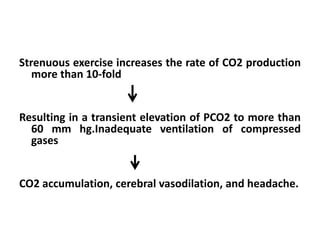
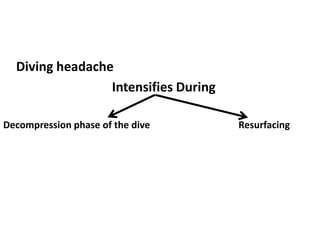
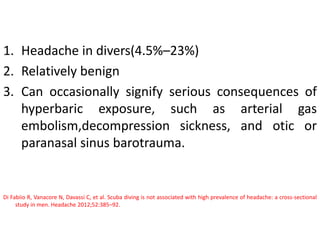
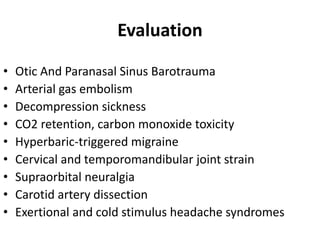
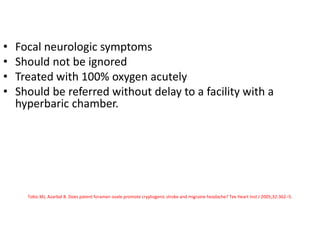
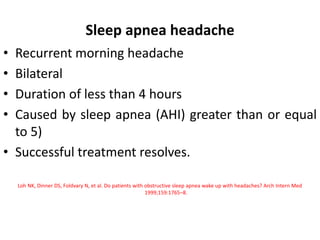
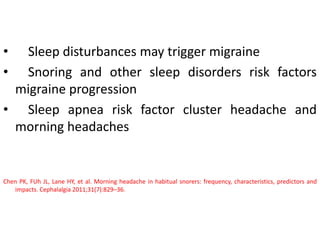
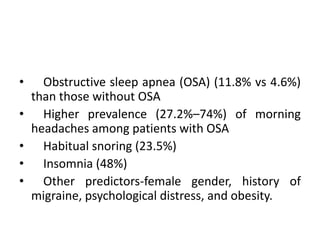
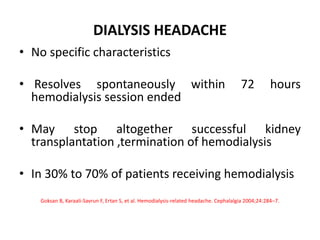
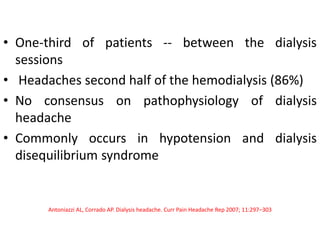
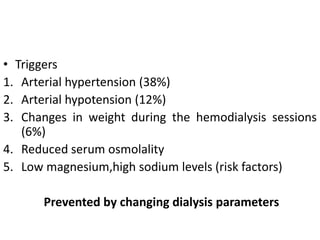
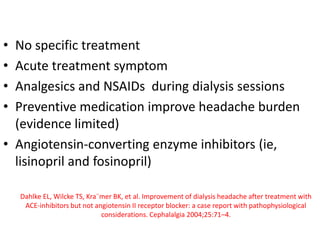
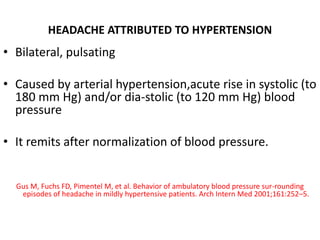
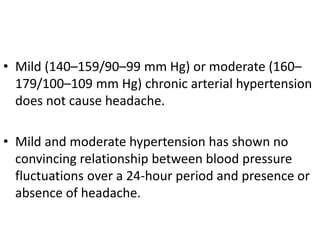
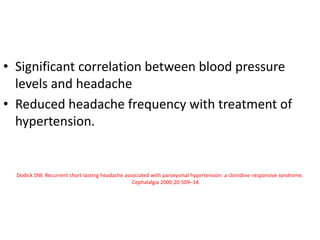
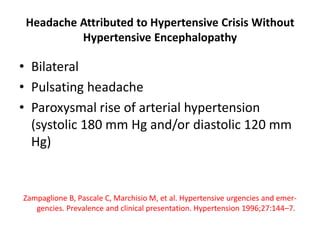
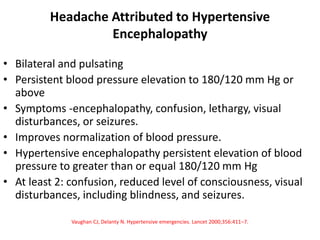
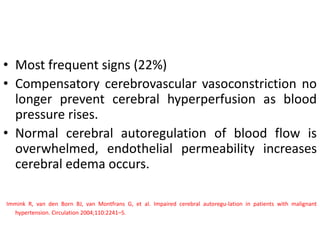
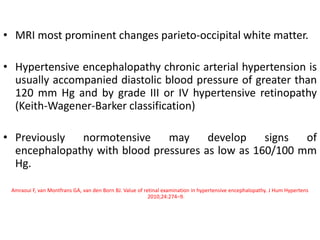
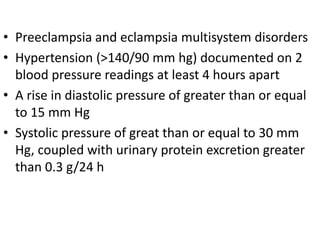
This document discusses various types of metabolic headaches according to the International Classification of Headache Disorders. It summarizes the diagnostic criteria and proposed pathophysiology for headaches attributed to conditions like high altitude, airplane travel, diving, sleep apnea, dialysis, hypertension, and pheochromocytoma. Specific details are provided on symptoms, triggers, evaluations and treatments for these secondary headache disorders related to disruptions in homeostasis.

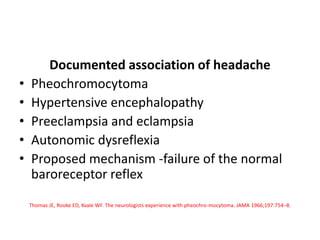
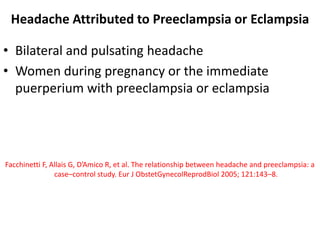
![• In addition, tissue edema, thrombocytopenia, and
abnormalities in liver function
• A case-control study found that headache was
significantly more frequent in patients with
preeclampsia (63%) than in controls (25%) (odds
ratio [OR] 4.95; 95% CI, 2.47–9.92)](https://image.slidesharecdn.com/metabolicheadache-200519205301/85/Metabolic-headache-53-320.jpg)