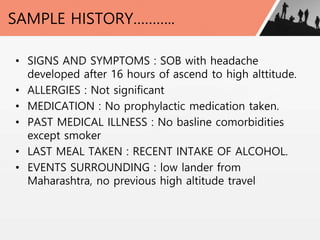
A 25-year-old male presented with shortness of breath and headache 16 hours after ascending to an altitude of 4,200 meters via cable car in Gulmarg, India. On examination, he had a respiratory rate of 36, oxygen saturation of 60% on room air, and clear lung sounds. He was given oxygen, paracetamol, and nifedipine and improved over 4 days, then was discharged. The document discusses various high altitude medical disorders, risk factors, management approaches, and advice for preventing issues like acute mountain sickness.