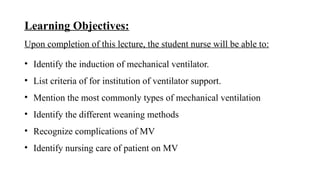
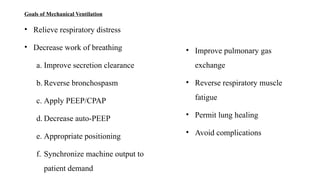
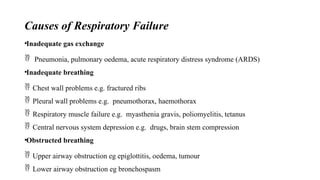
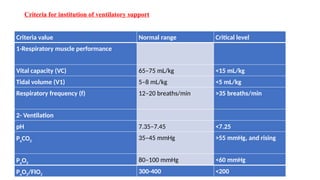
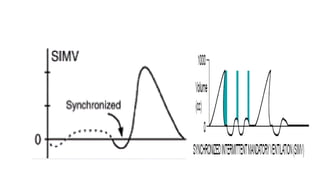
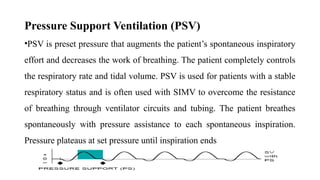
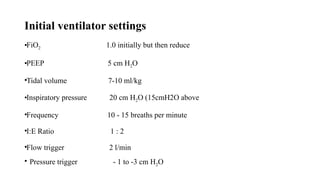
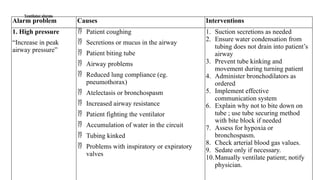
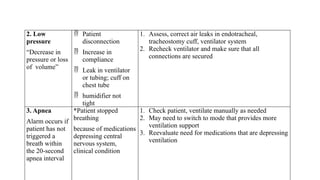
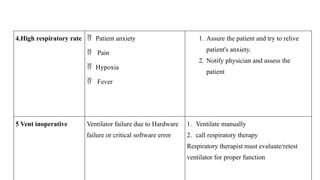
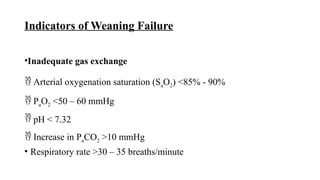
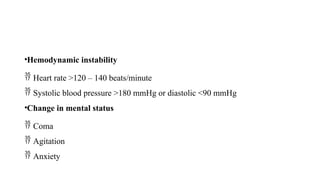
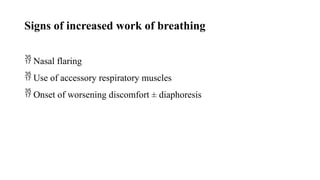
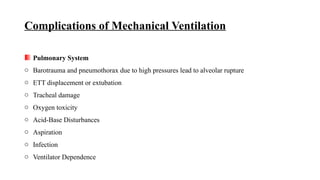
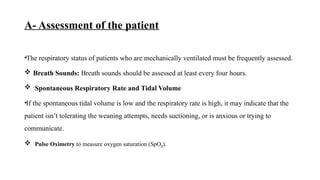
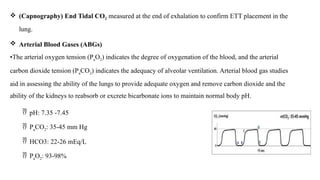
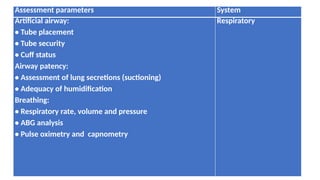
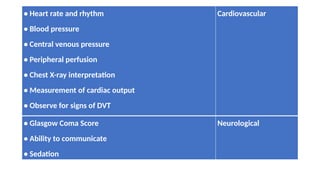
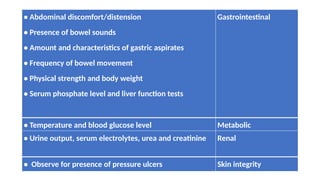
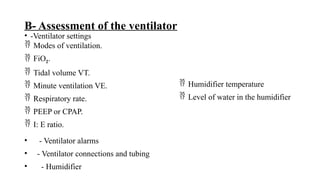
This document outlines the objectives and definitions related to mechanical ventilation, including indications, types, and modes of ventilation, as well as criteria for instituting ventilatory support. It discusses various ventilator settings, weaning methods, potential complications, and nursing care for patients on mechanical ventilation. Additionally, the document emphasizes the importance of ongoing assessment of both the patient and the ventilator to ensure proper functioning and patient safety.