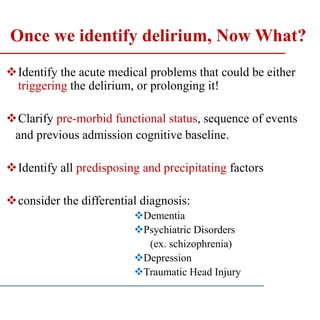
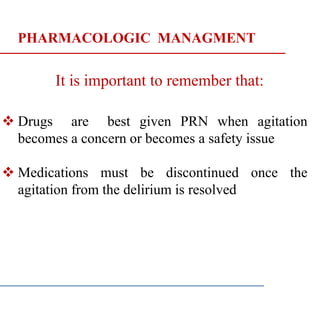
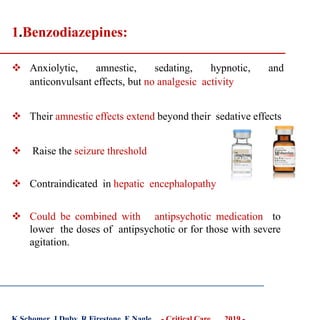
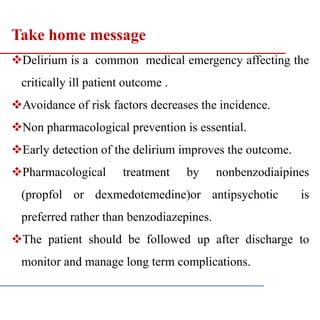
This document provides a protocol for assessing and managing ICU psychosis or delirium. It defines delirium and discusses its high incidence in ICU patients. Risk factors and pathophysiology are described. The importance of recognizing delirium is emphasized, and tools like the ICDSC and CAM-ICU for assessment are presented. Both non-pharmacological and pharmacological management strategies are outlined, including prevention techniques like the ESCAPE bundle. Common treatment medications like haloperidol and dexmedetomidine are discussed. The need for follow-up care to monitor long-term outcomes is also highlighted.
![Incidence of delirium
Delirium is one of the most common of medical
emergencies affecting up to 80% of patients in the intensive
care unit [ICU]) ,
Annoying fact.......Annoying disease
Marcantonio ER. N Engl J Med 2017;377(15):1456-66.
Most common psychiatric syndrome found in the general
hospital setting.
Upto 25% of hospitalized cancer patients
Upto 51% of postoperative patients
Patients, who develop delirium in the intensive care until
(ICU), have a two to four fold-increased risk of death
out of the hospital.](https://image.slidesharecdn.com/icupsychosis-200311192054/85/Icu-Psychosis-7-320.jpg)
![RECOGNITION OF DELIRIUM
1-EARLY PREDICTION
The Prediction of Delirium in ICU Patients (PRE-
DELIRIC) model uses 10 predictors :
AGE
APACHE II
Admission group,
Urgent admission,
Urea level,
Morphine use,
Metabolic acidosis
Sepsis
Sedation,
Coma,
Wassenaar A, et al. Intensive Care Med 2015;41:1048–56.[Article] [PubMed] [PMC]](https://image.slidesharecdn.com/icupsychosis-200311192054/85/Icu-Psychosis-13-320.jpg)
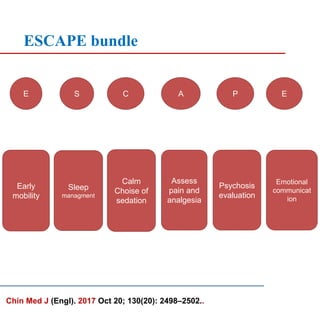
![ No recommendation for using a pharmacologic delirium
prevention protocol [administering prophylactic
antipsychotics to the general ICU population] in adult
ICU patients
Early and aggressive mobilization may reduce the
incidence and duration of delirium, shorten ICU and
hospital LOS, and lower hospital costs.
There is evidence based delirium prevention strategy .
[“ESCAPE” bundle]
What About Prevention?
Arch Intern Med. 2003;163(8):958-964. doi:10.1001/archinte.163.8.958
Try to Make ICU Less Traumatic for Patients, Families - Medscape - Jul 16 2019.](https://image.slidesharecdn.com/icupsychosis-200311192054/85/Icu-Psychosis-19-320.jpg)
![ A high-potency dopamine- blocking agent is most frequently
used because of its short half-life, few or no anticholinergic
side effects, no active metabolites, and lower sedation.
Oral or parenteral.
Safe in hepatic insufficiency
2.Butyrophenones
Comparisons of haloperidol and other antipsychotics did not find
any antipsychotic to be more effective than another.(e.g
quetapine or respirdone)
World Health Organization (WHO). [cited 29 Nov 2018].
Available from url: https://www.who.int/classifications/icd/en/GRNBOOK.pdf](https://image.slidesharecdn.com/icupsychosis-200311192054/85/Icu-Psychosis-23-320.jpg)
![ Dose-dependent respiratory depression and hypotension
Propofol infusion syndrome (PRIS)
propofol infusion syndrome [PRIS]
worsening metabolic acidosis
Hypertriglyceridemia
hypotension with increasing vasopressor requirements
Arrhythmias
Acute kidney
injury
hyperkalemia
rhabdomyolysis
liver dysfunction
[usually associated with prolonged administration of high
propofol doses (> 70 μg/kg/min)]
Side effects :
Kam, PC; . (July 2007). "Propofol infusion syndrome". Anaesthesia. 62
(7): 690–701.last edited on 29 January 2019](https://image.slidesharecdn.com/icupsychosis-200311192054/85/Icu-Psychosis-27-320.jpg)
![REFFERENCES
1. Boltey EM, Iwashyna TJ, Hyzy RC, Watson SR, Ross C, Costa DK. J Crit Care.
2019 Mar 01;51:192-197.
2. Marcantonio ER.. N Engl J Med 2017;377(15):1456-66.
3. Persico I, Cesari M, Morandi A, Haas J, Mazzola P, Zambon A, et al. J Am Geriatr
Soc 2018;66(10):2022-30 https://www.mayoclinic.org -20371386Jun 27, 2018 MAJ
Open. 2019 Apr-Jun; 7(2): E294–E299.
4. Babar A. Khan et al , Crit Care Med. 2017 May; 45(5): 851–857.
5. Devlin JW, Skrobik Y, Gelinas C, et al. Crit Care Med 2018; 46:e825–e873
Medscape - Jul 16 2019.
6. Whitlock EL. et al. K Schomer, J Duby, R Firestone, E Nagle… - Critical Care …,
2019 - Anesthesia & Analgesia 2014;118(4):809-17. World Health Organization
(WHO).. [cited 29 Nov 2018].
7. N Haque, RM Naqvi, M Dasgupta - Canadian Geriatrics Journal, 2019 -
gjonline.ca
8. T Saito, H Toda, GN Duncan, SS Jellison, T Yu… - bioRxiv, 2019 - biorxiv.org
9. KL Houseknecht, M May, M Beauchemin, D Barlow… - The FASEB …, 2019
10.Kam, PC; Cardone D. (July 2007). Anaesthesia. 62 (7): 690–701.last edited on 29
January 2019
11.Louis C, Godet T, Chanques G, Bourguignon N, Morand D, Pereira B, . 2018
12.Barr J, Fraser GL, Puntillo K, et al; American College of Critical Care Medicine,Crit
Care Med 2013; 41:263–306
13.Devlin JW, Skrobik Y, Gelinas C, et al: Crit Care Med 2018; 46:e825–e87
14.Salluh JIF, Wang H, Schneider EB, Nagaraja N, Yenokyan G, Damluji A, et al BMJ
2015;350:h2538.](https://image.slidesharecdn.com/icupsychosis-200311192054/85/Icu-Psychosis-35-320.jpg)