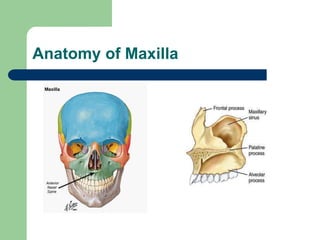
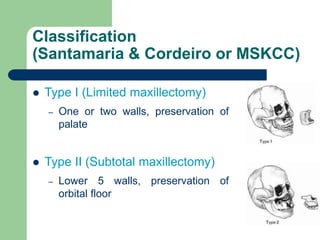
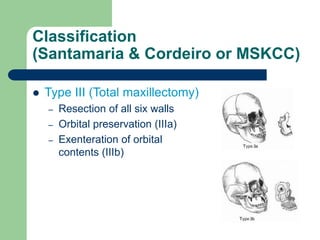
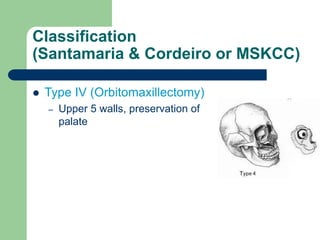
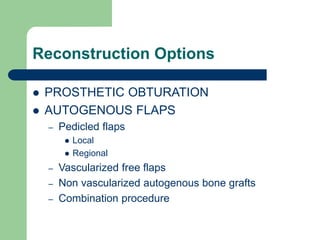
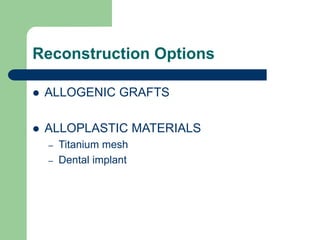
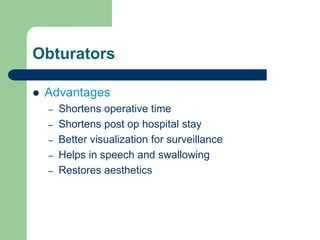
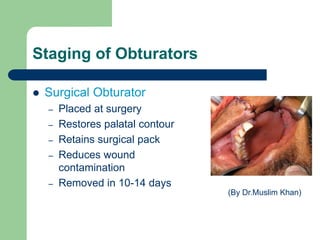
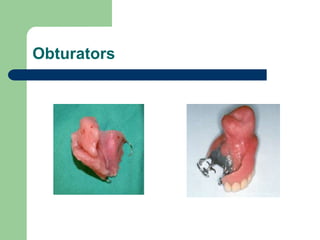
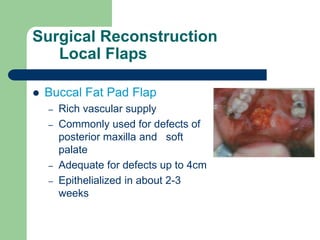
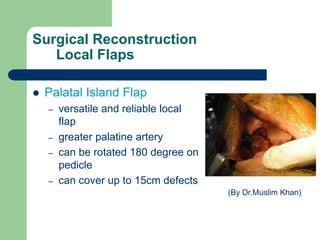
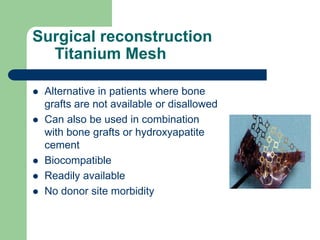
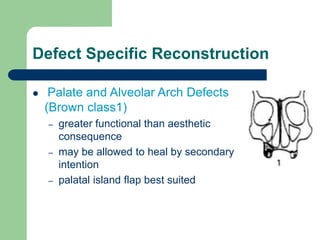
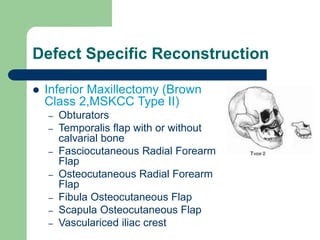
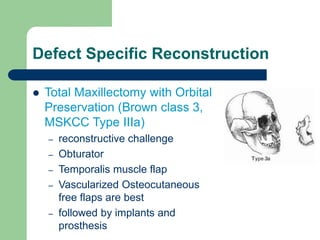
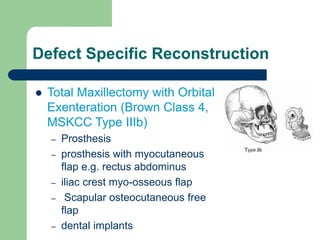
This document summarizes reconstruction of the maxilla following maxillectomy. It describes the anatomy and goals of maxillary reconstruction. Maxillectomy defects are classified and reconstruction options are outlined, including prosthetic obturators, local and regional pedicled flaps, microvascular free flaps, bone grafts, and titanium mesh. Defect-specific reconstruction approaches are provided for different types of maxillectomy defects, such as palate defects, inferior maxillectomies, total maxillectomies with and without orbital exenteration, and orbitomaxillectomies.