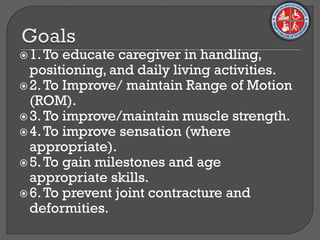
This document outlines the physiotherapy management of brachial plexus injuries in children at different stages of development. It describes the brachial plexus and types of injuries. Rehabilitation is divided into 5 stages focused on improving range of motion, muscle strength, sensation and age-appropriate milestones through techniques like passive and active movement, splinting and functional activities. Complications are addressed and techniques like electrical stimulation are used. The overall goal is to prevent deformities and learned non-use while regaining optimal function.