This document discusses the management of spasticity through pharmacological, surgical, and physiotherapy approaches.
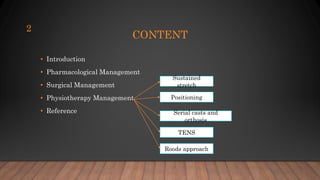
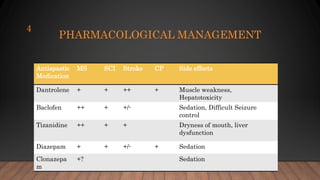
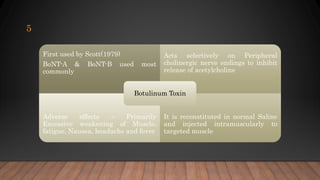
Pharmacological management includes medications like baclofen, tizanidine, and diazepam which can help reduce spasticity but have side effects like sedation. Botulinum toxin injections target specific muscles to weaken them.
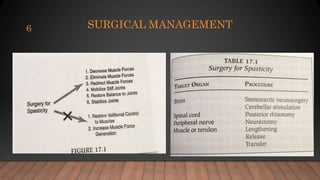
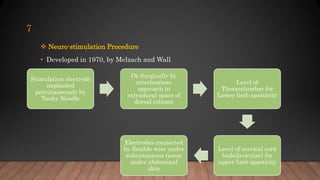
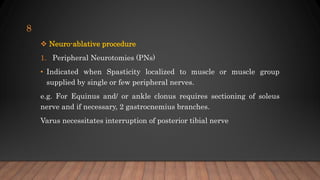
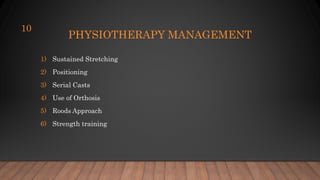
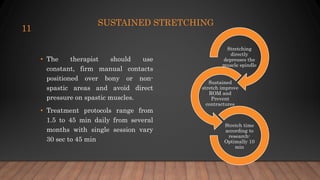
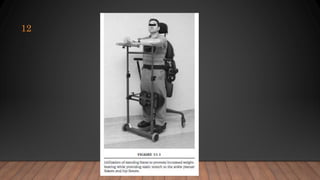
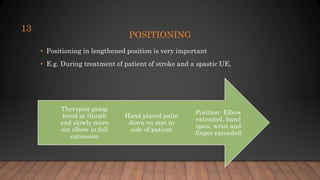
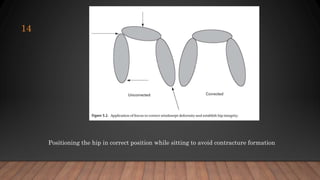
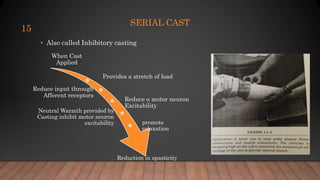
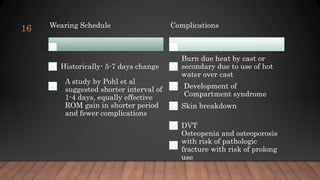
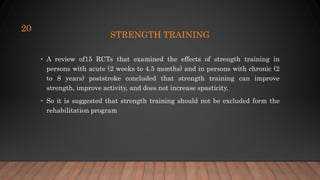
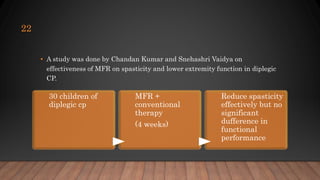
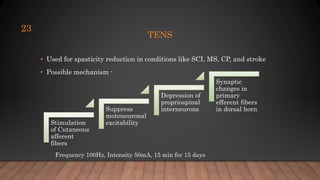
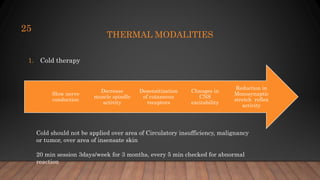
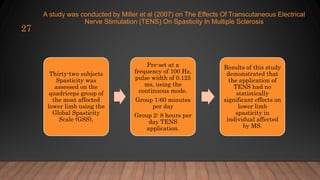
Surgical options are neurostimulation or neuroablative procedures like peripheral neurotomies. Physiotherapy includes sustained stretching, positioning, serial casting, orthotics, strength training, Roods approach, and modalities like TENS, heat, and cold therapy. Studies show these approaches can effectively reduce spasticity without increasing weakness. Management must be tailored to