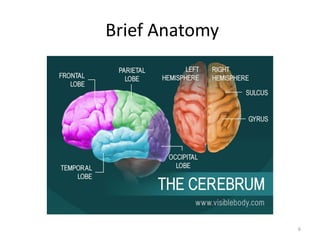
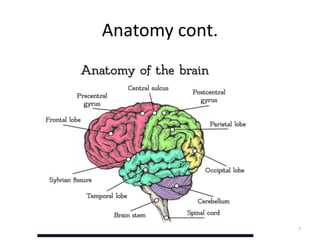
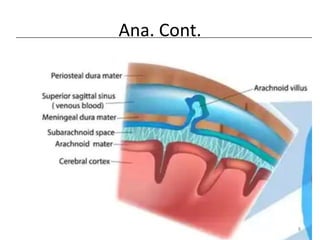
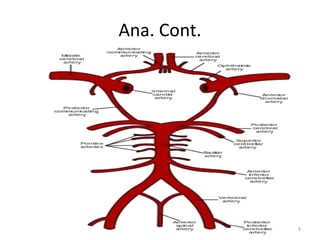
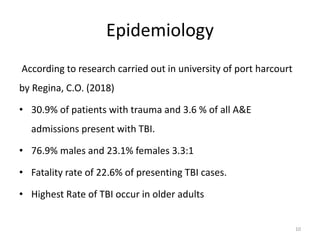
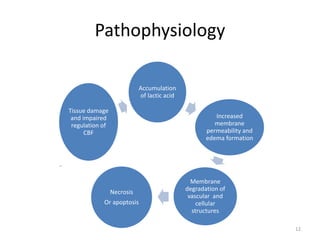
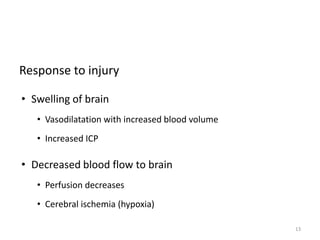
- The document presents a physiotherapy assessment of traumatic brain injury when the patient is unconscious. It covers definitions of TBI, brief brain anatomy, epidemiology showing high rates in males and older adults, and common causes being road accidents and falls.
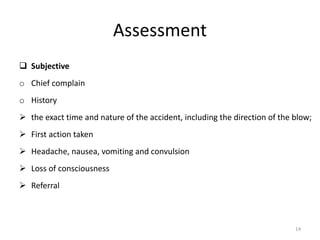
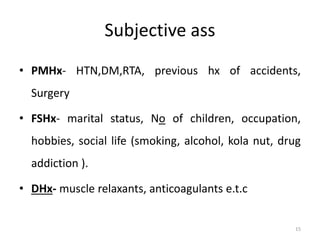
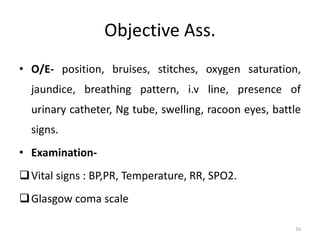
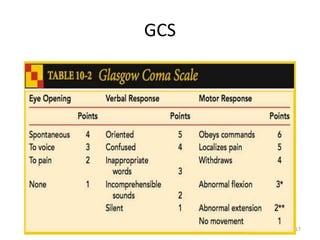
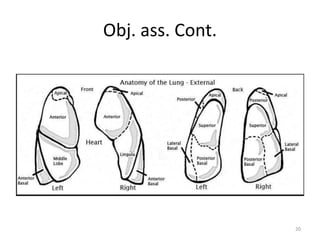
- The assessment includes subjective information from the patient's history and objective examination of vital signs, Glasgow Coma Scale, and neurological assessment.
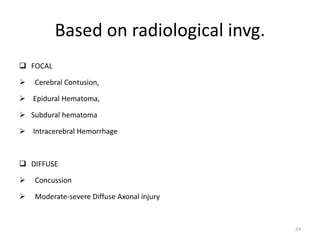
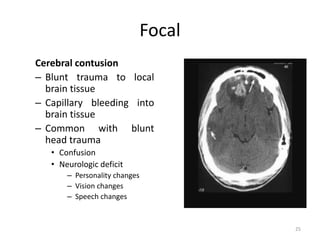
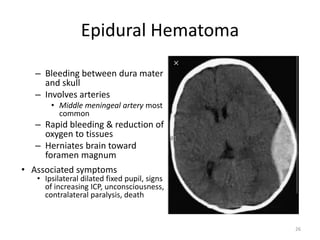
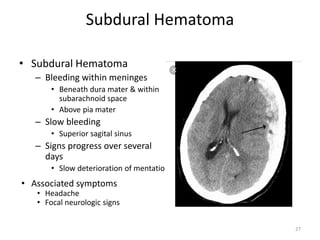
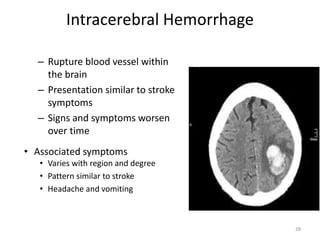
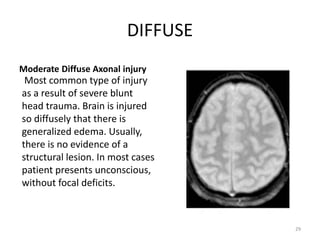
- Common radiological findings are discussed including focal injuries like contusions and hematomas, as well as diffuse injuries like concussions and diffuse axonal injury. Proper assessment is important for accurate diagnosis and management of TBI patients.