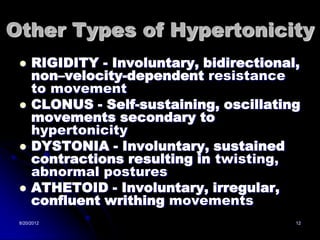
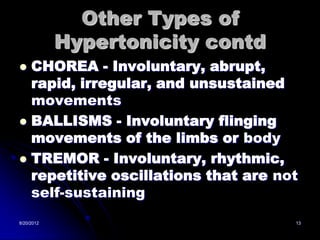
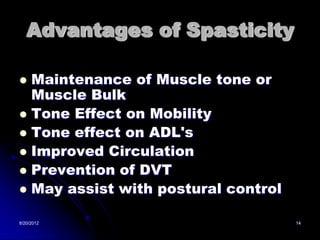
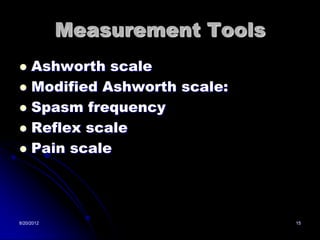
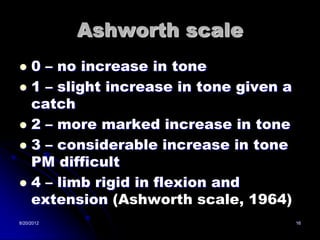
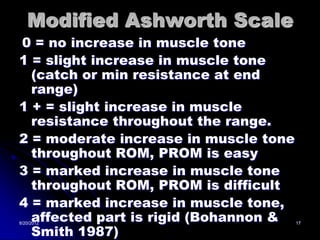
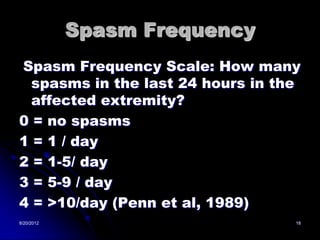
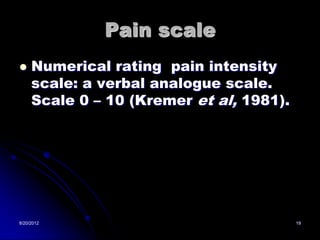
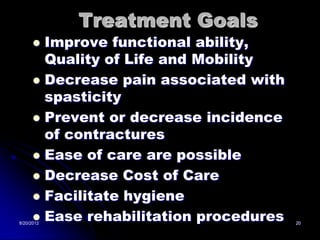
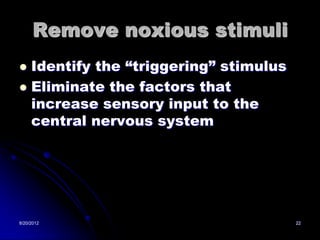
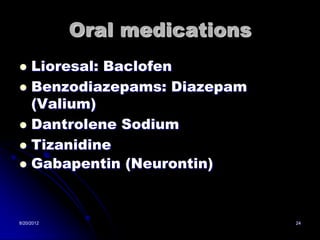
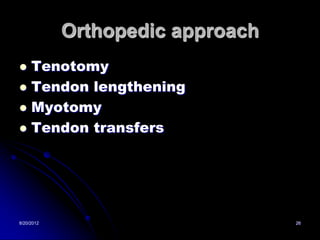
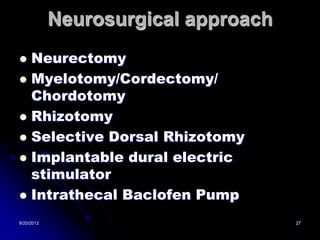
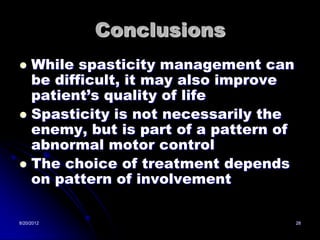
This document discusses spasticity after stroke. It defines spasticity as an abnormal muscle tone with increased resistance to passive stretch. There are different types of spasticity including lead pipe, cogwheel, and clasp knife. The pathophysiology involves loss of inhibitory control in the spinal cord. Treatment options include rehabilitation therapy, oral medications, neurolysis, orthopedic procedures, and neurosurgery. Measurement tools include the Ashworth scale and pain scales. The goals of treatment are to improve function and mobility while decreasing pain.