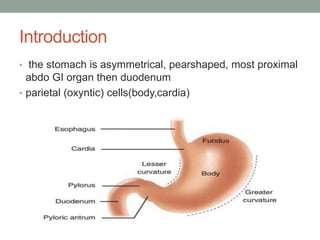
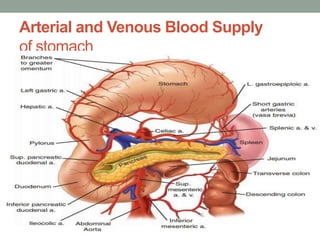
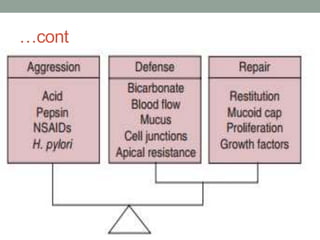
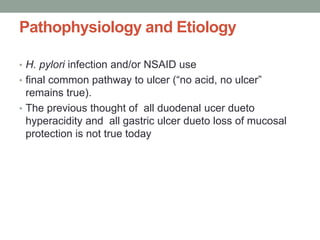
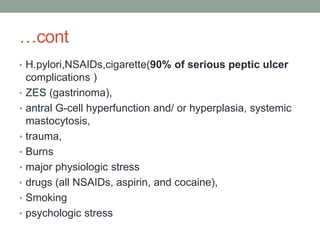
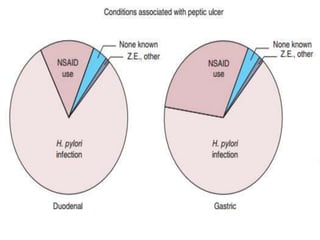
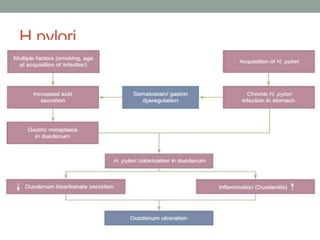
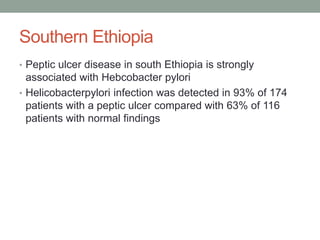
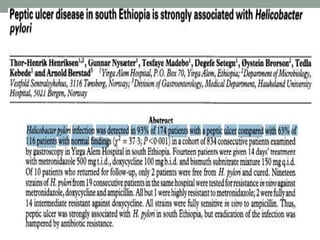
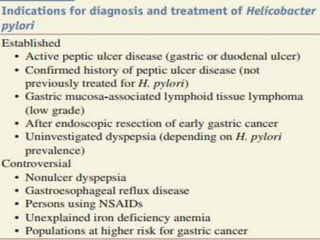
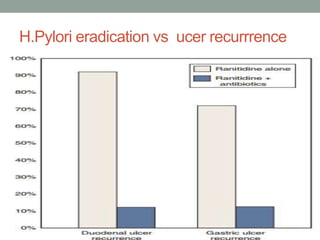
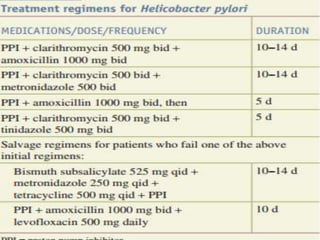
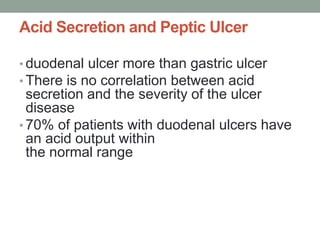
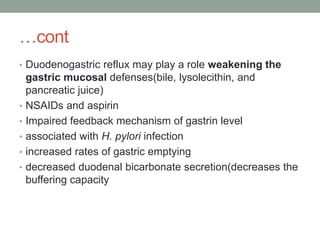
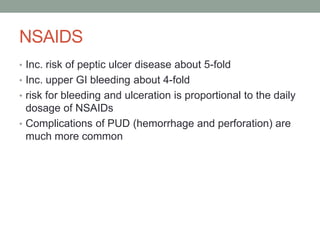
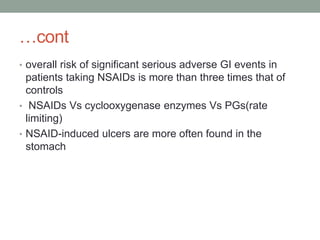
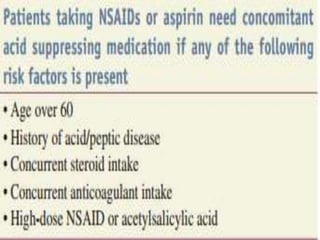
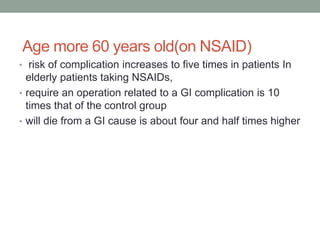
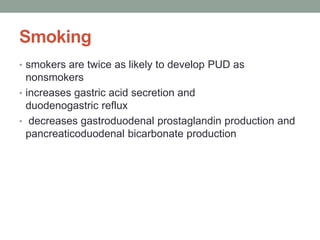
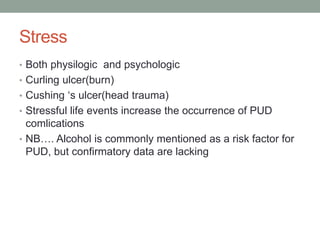
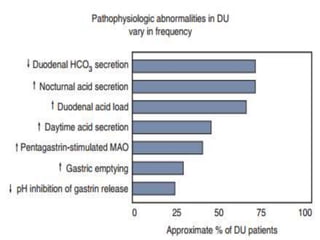
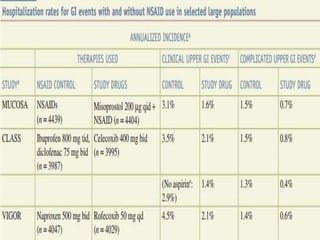
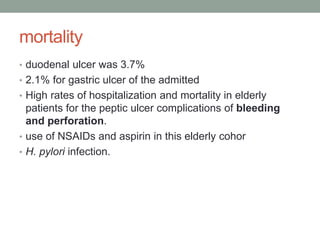
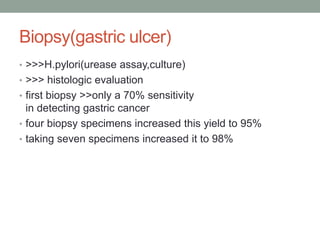
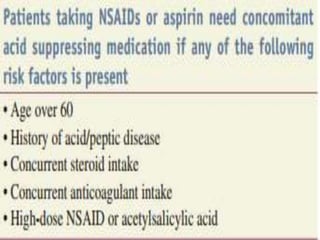
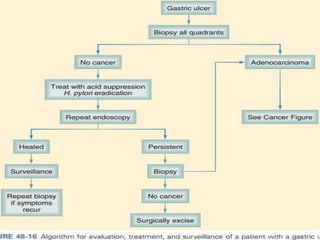
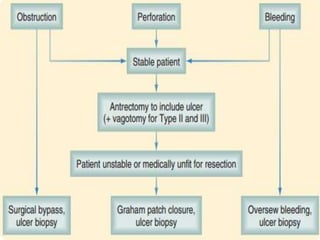
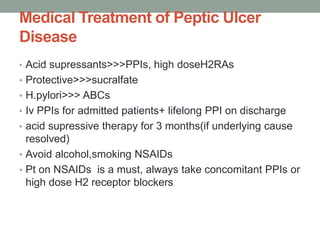
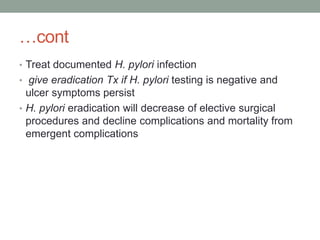
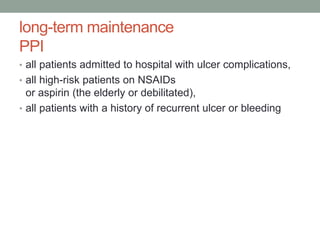
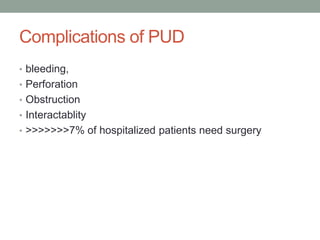
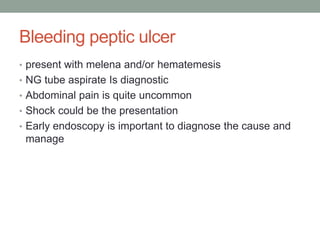
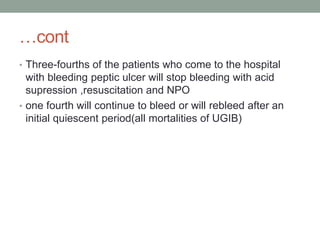
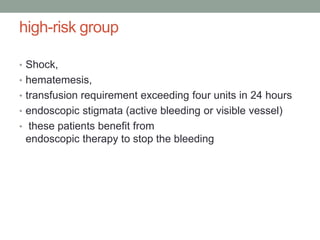
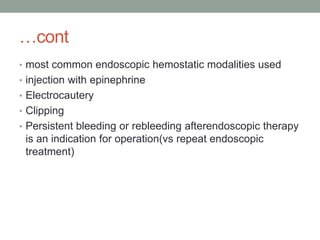
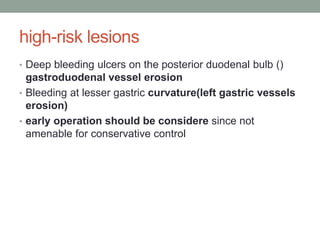
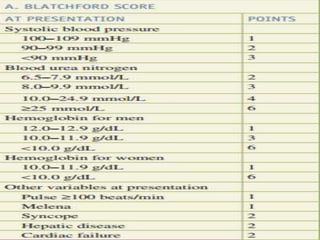
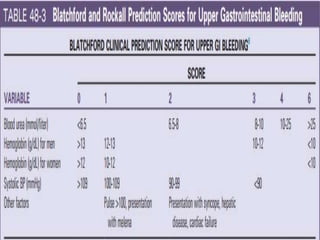
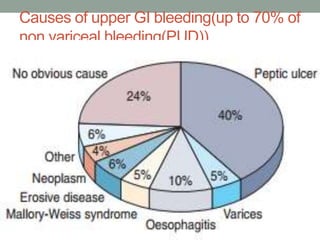
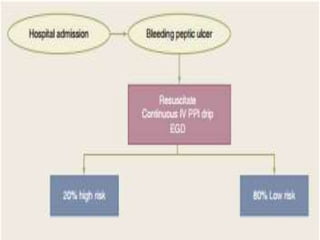
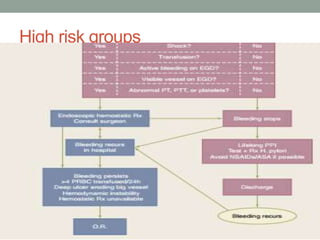
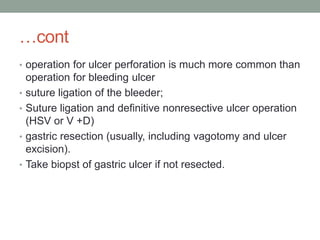
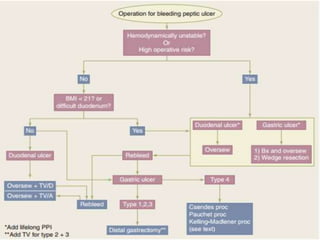
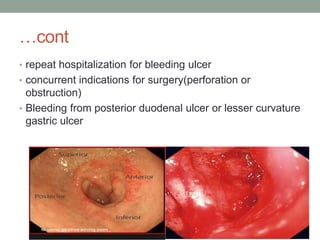
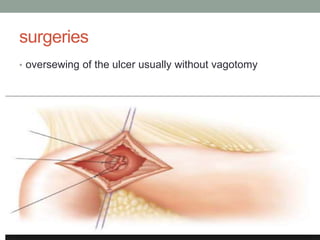
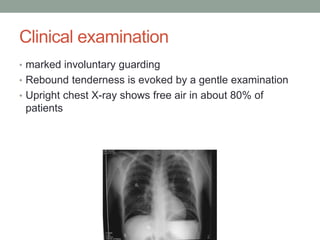
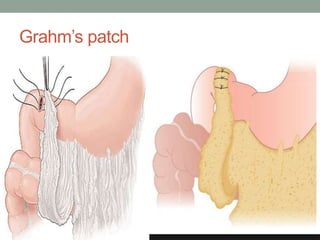
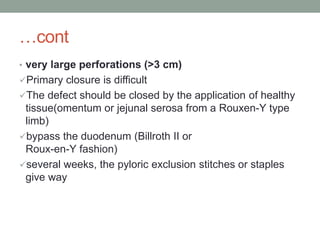
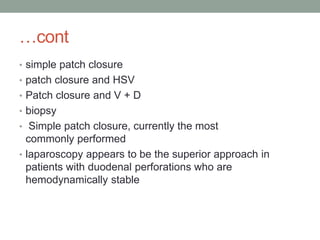
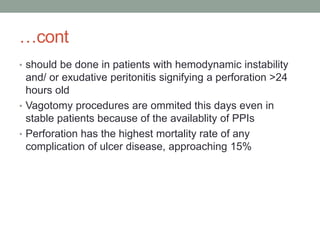
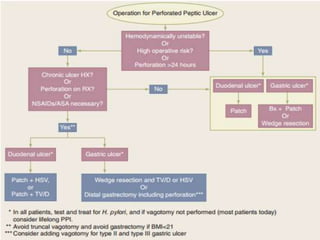
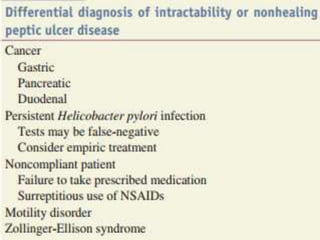
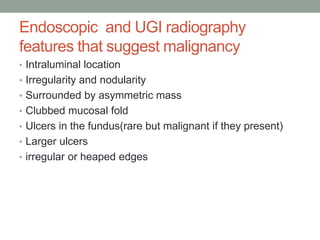
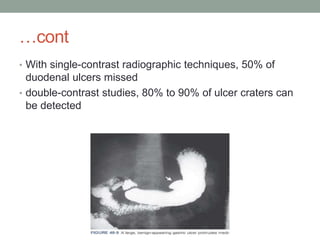
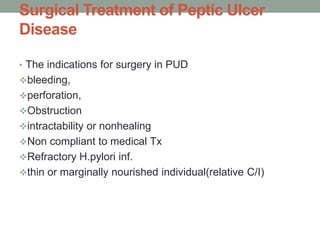
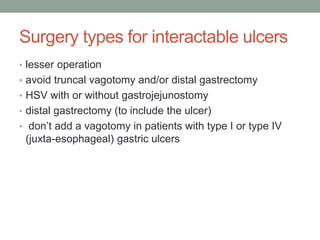
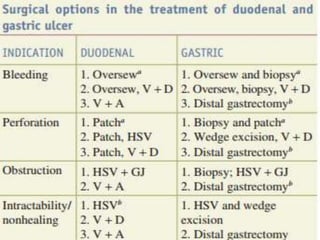
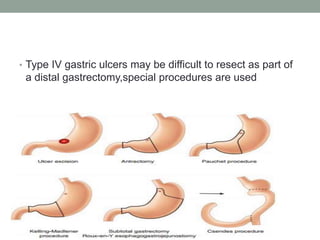
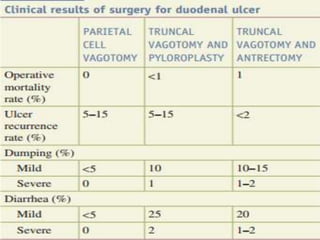
This document provides an overview of peptic ulcer disease (PUD) and its management. It discusses the types and causes of PUD, including Helicobacter pylori infection and NSAID use. Complications of PUD like bleeding, perforation, and obstruction are also covered. The management of PUD focuses on medical treatment with acid suppressants, H. pylori eradication therapy, and long-term maintenance to prevent recurrence. Surgical treatment may be needed for complications that do not respond to medical management.