The document provides guidance on positioning a patient for a cranio-caudal (CC) mammogram view. Key points include:
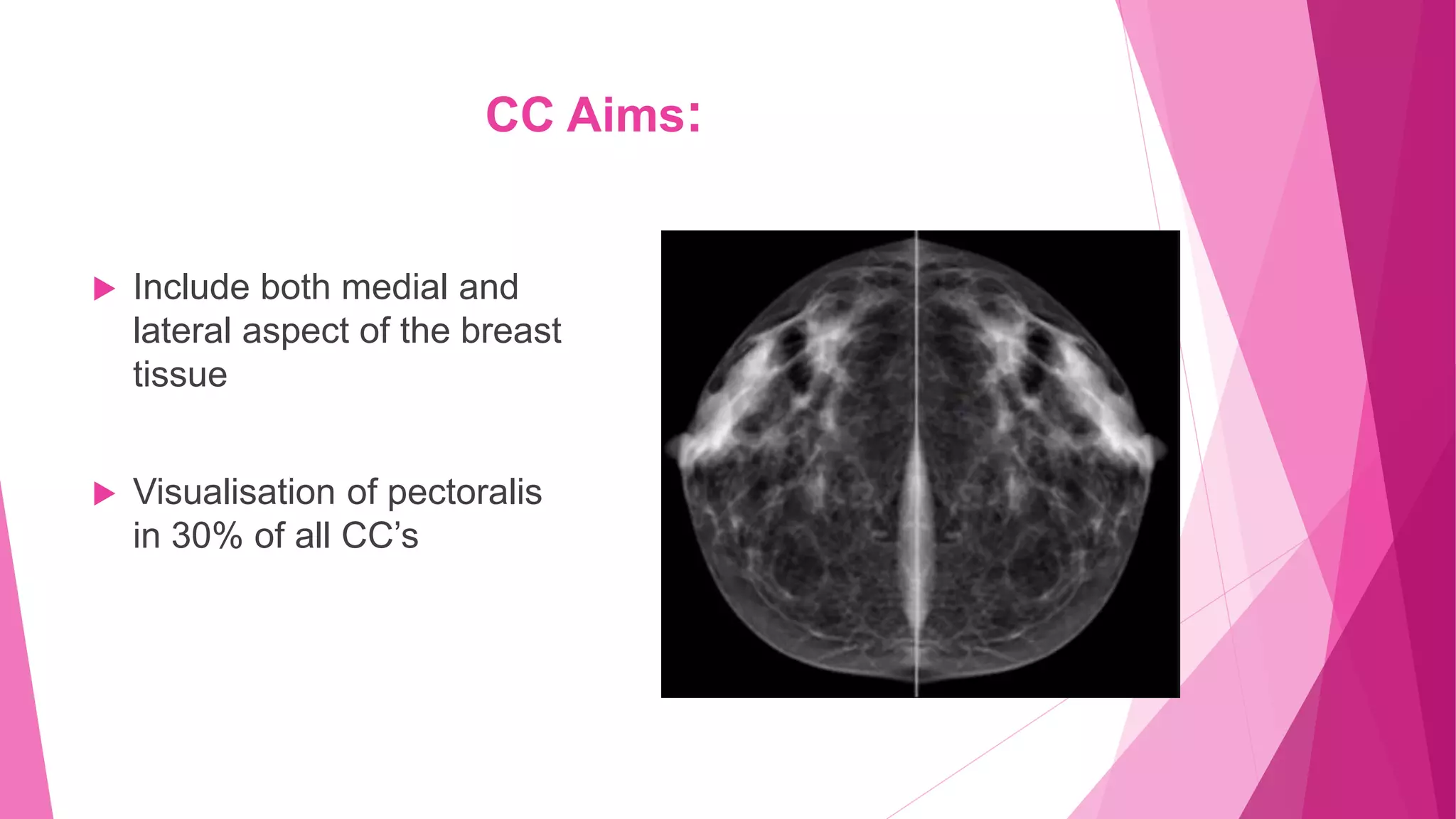
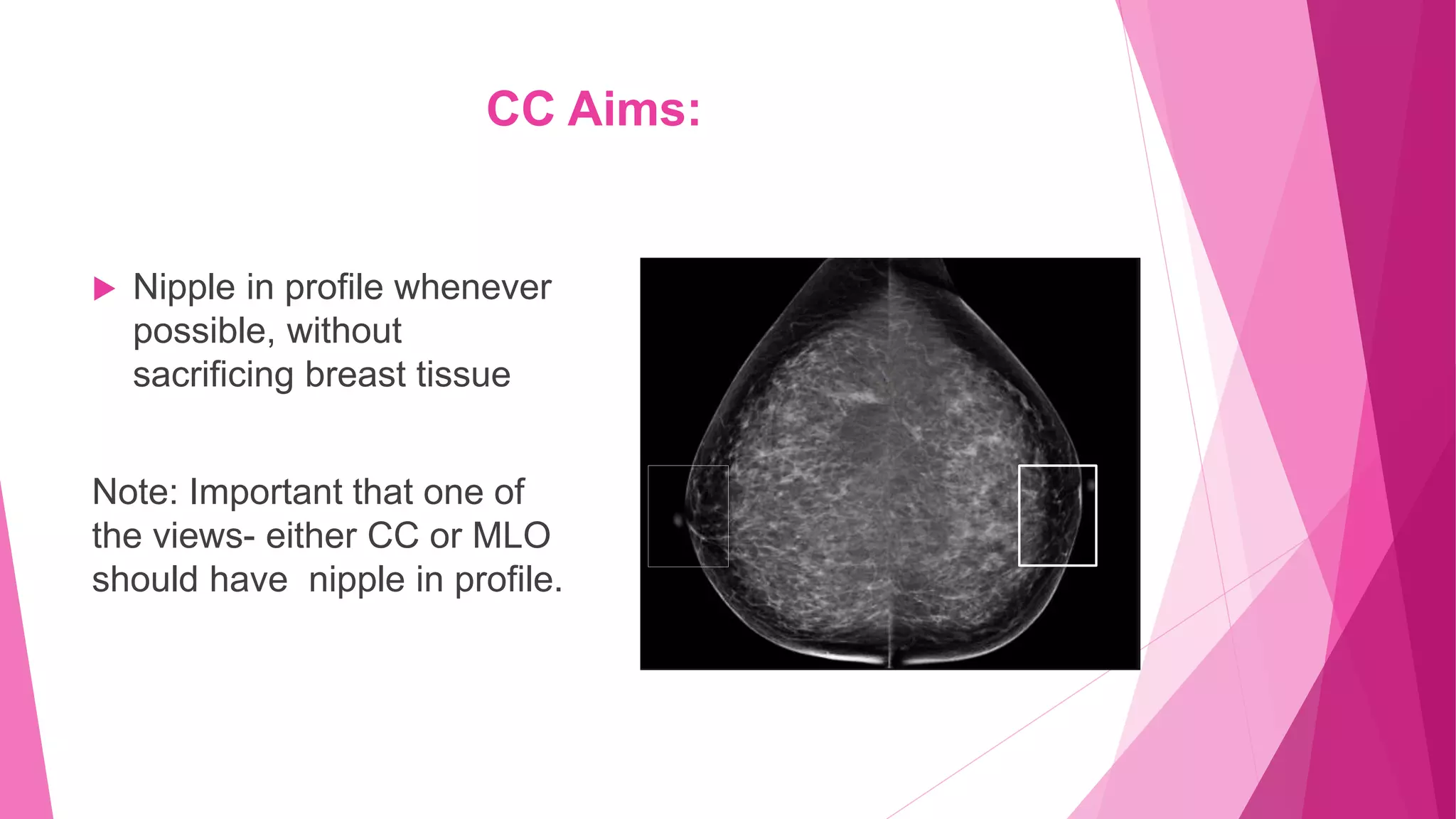
1. The CC view visualizes the sub-areolar, central, medial, and posteromedial breast tissue. Proper positioning brings the breast into its natural anatomical position with the nipple perpendicular to the chest wall.
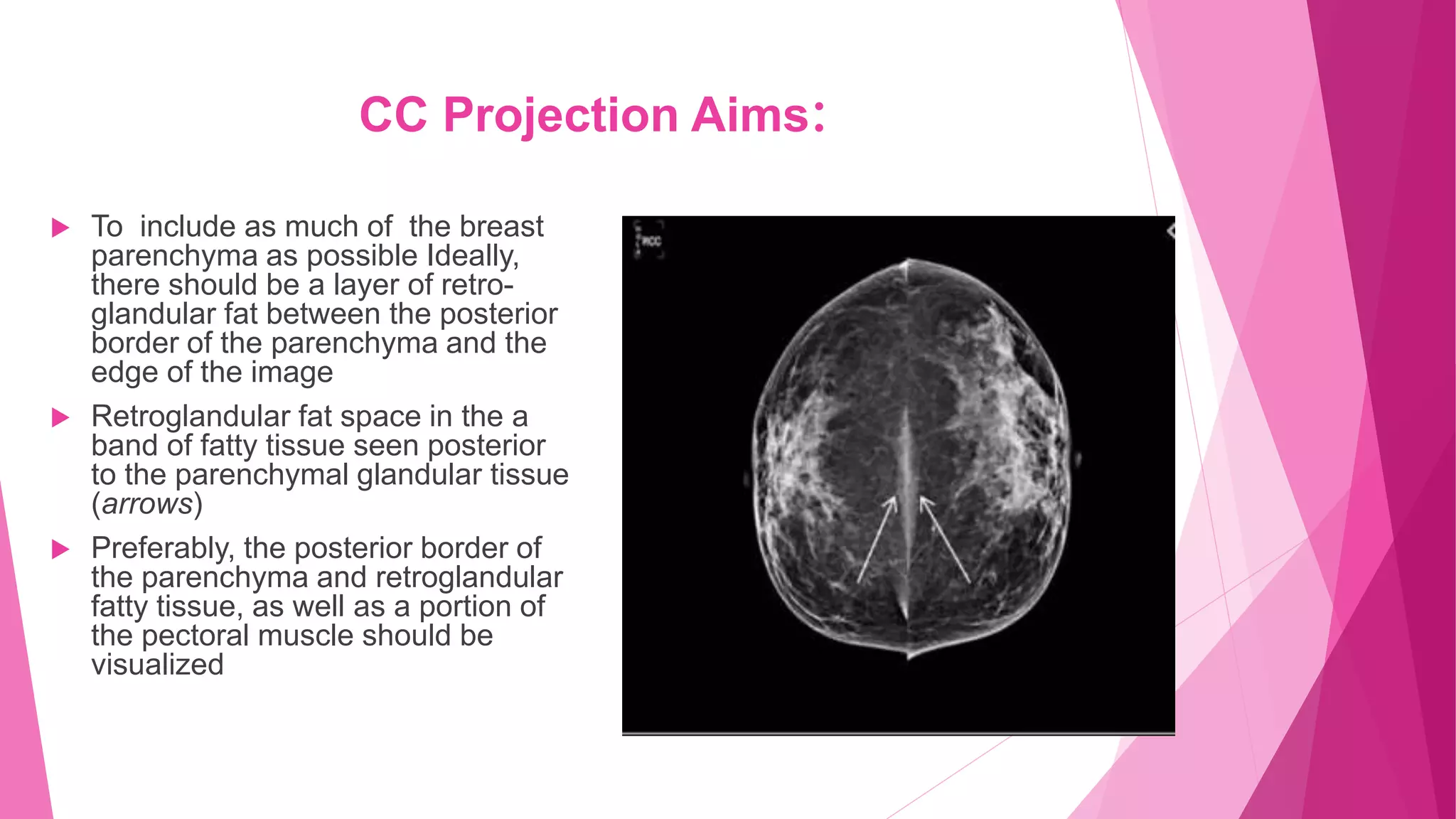
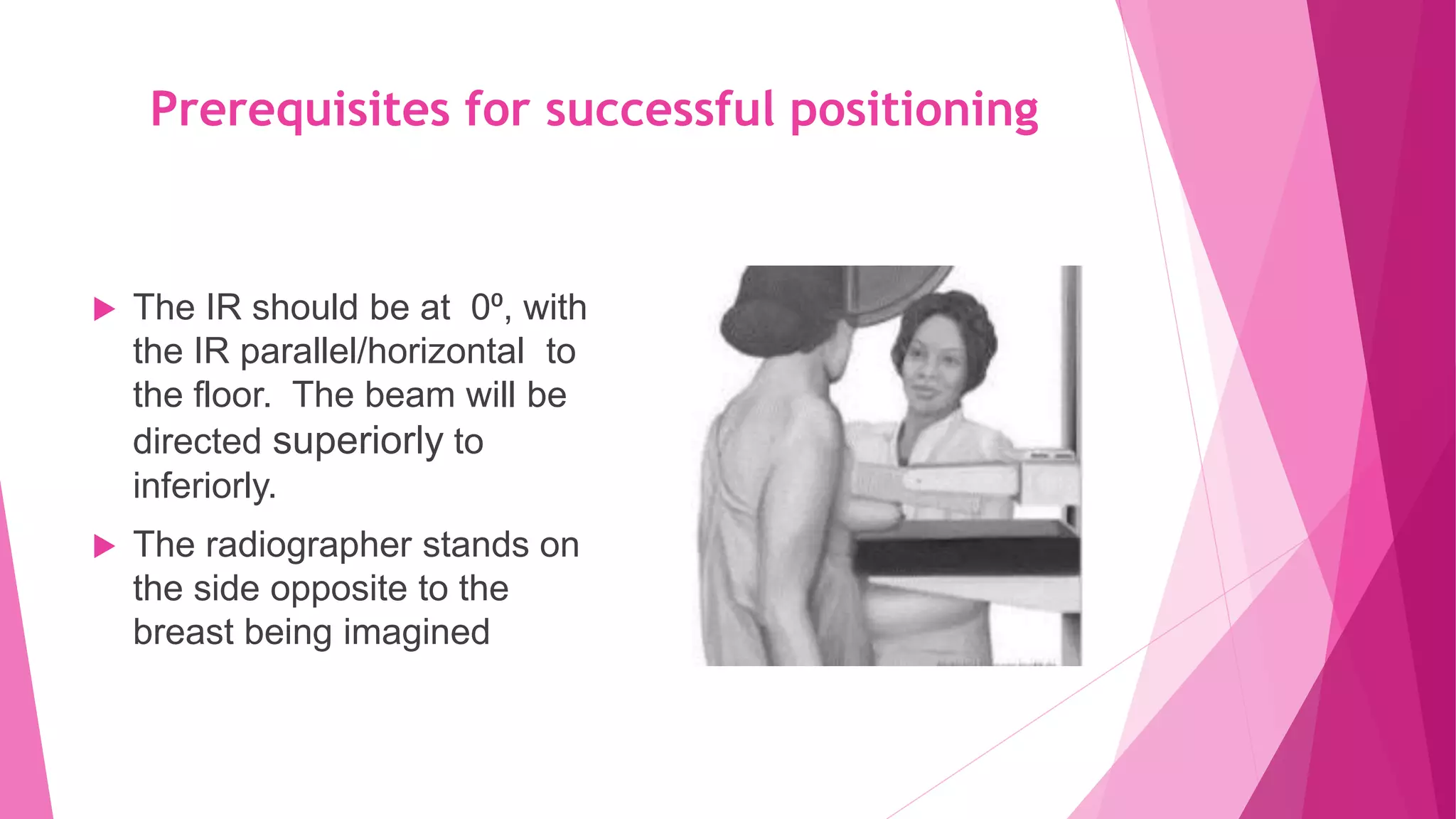
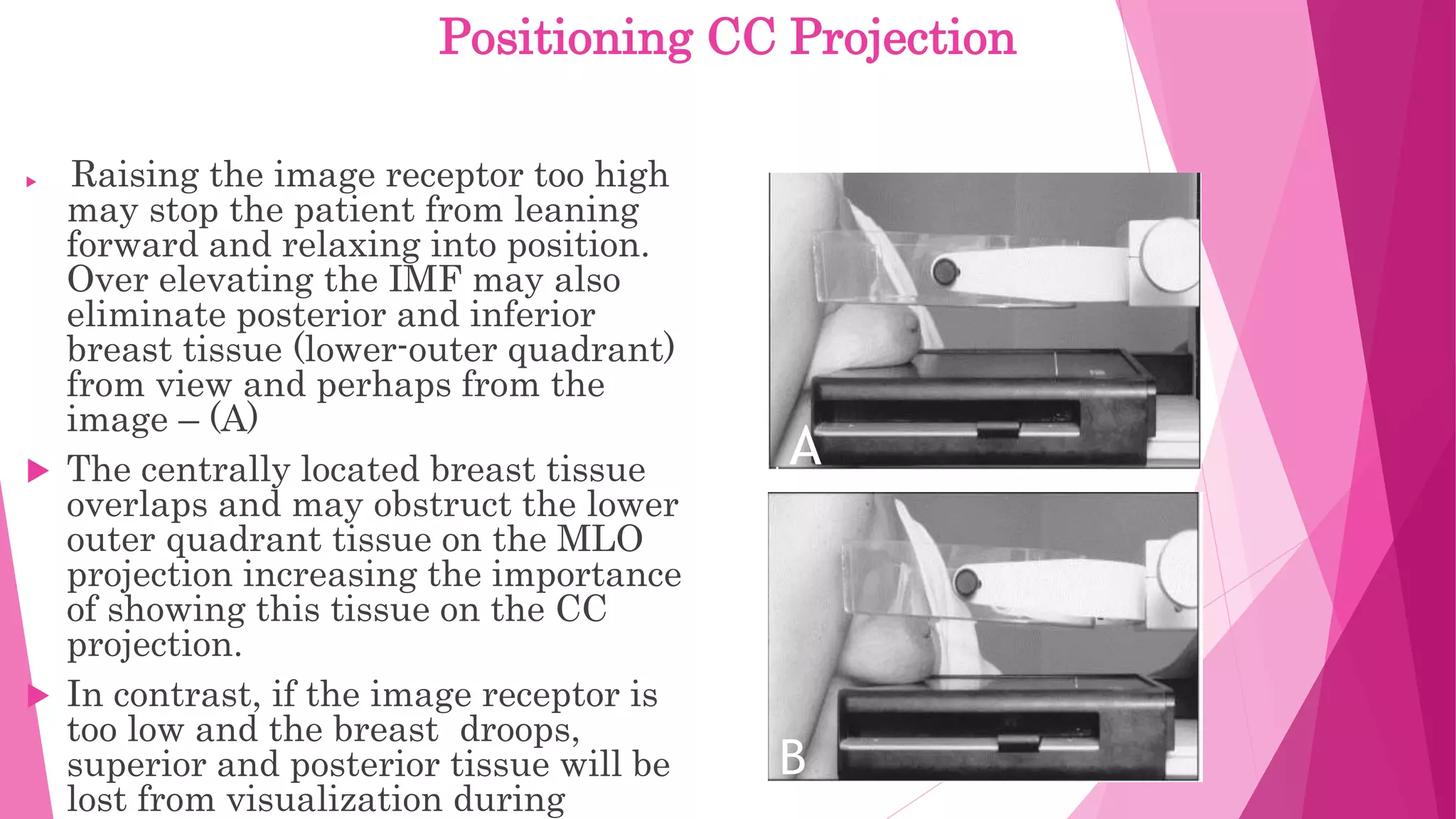
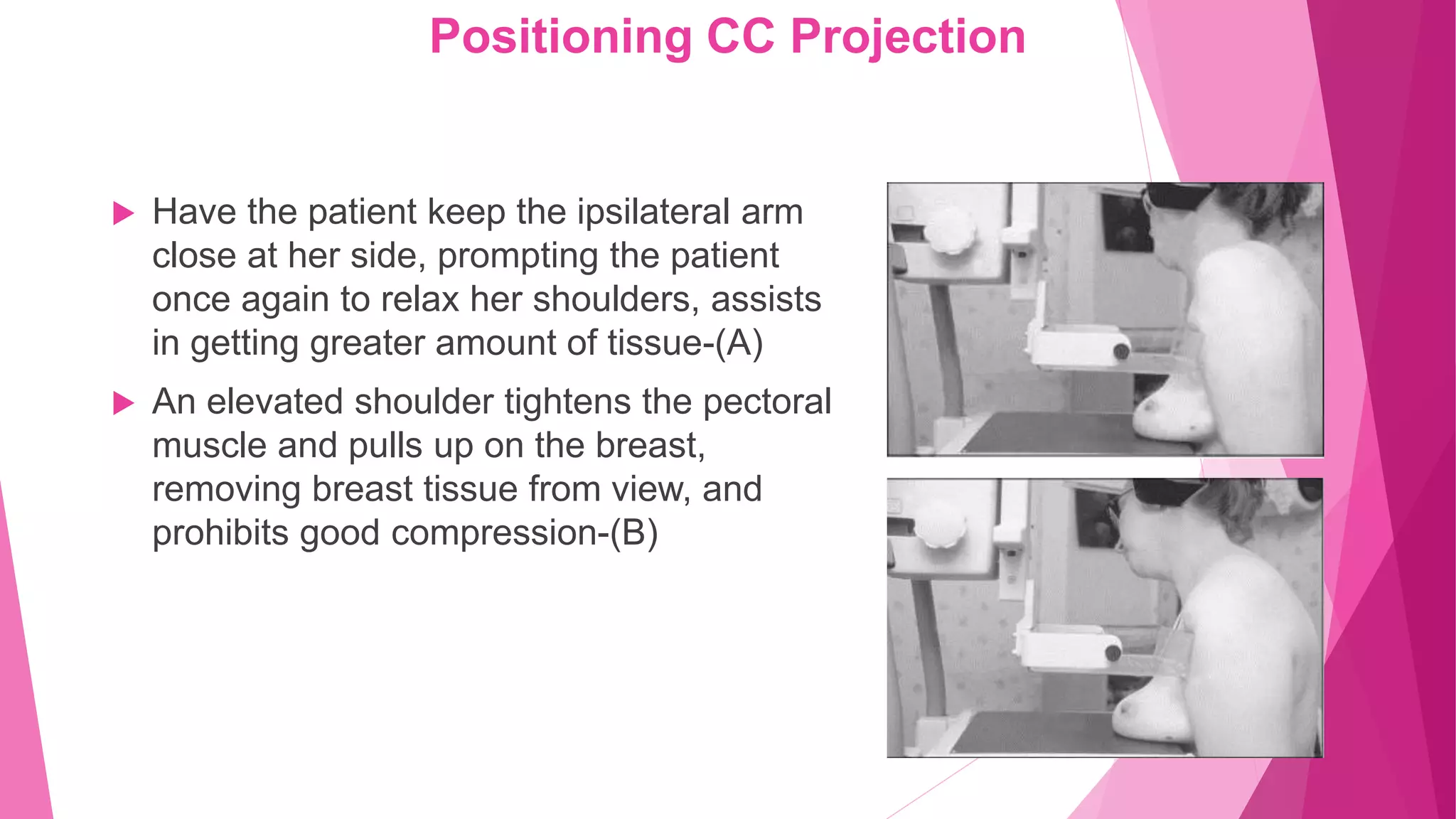
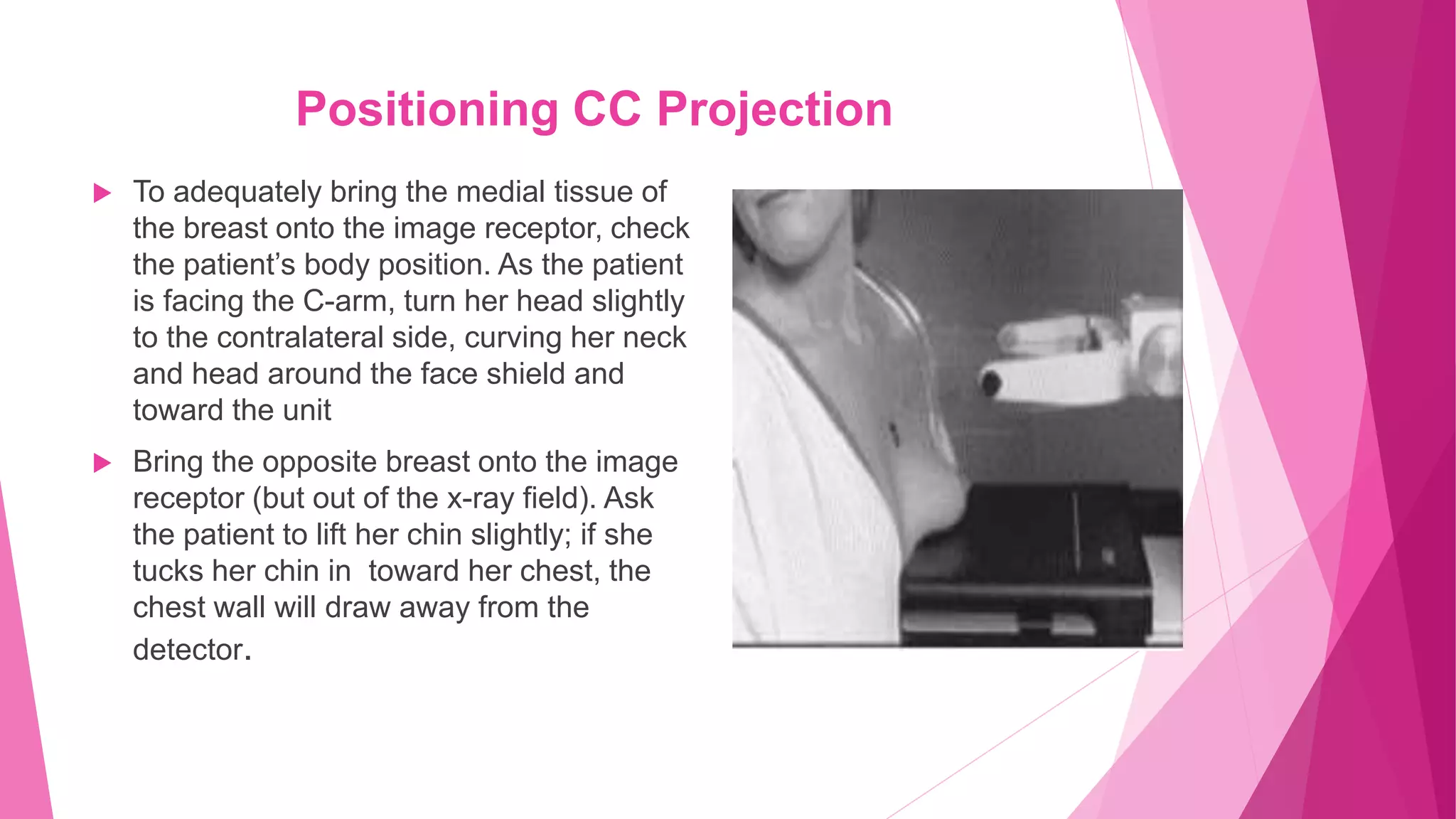
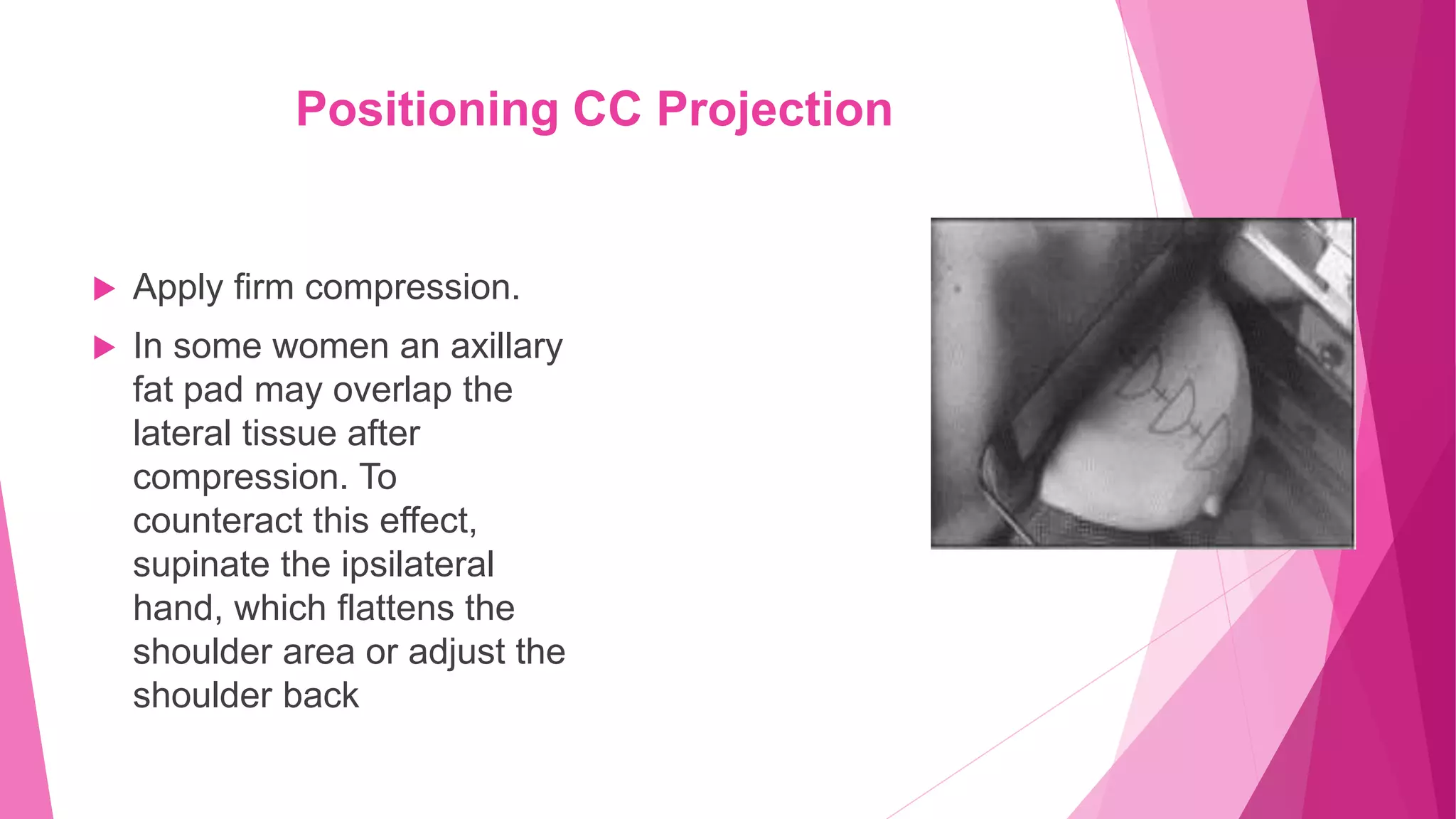
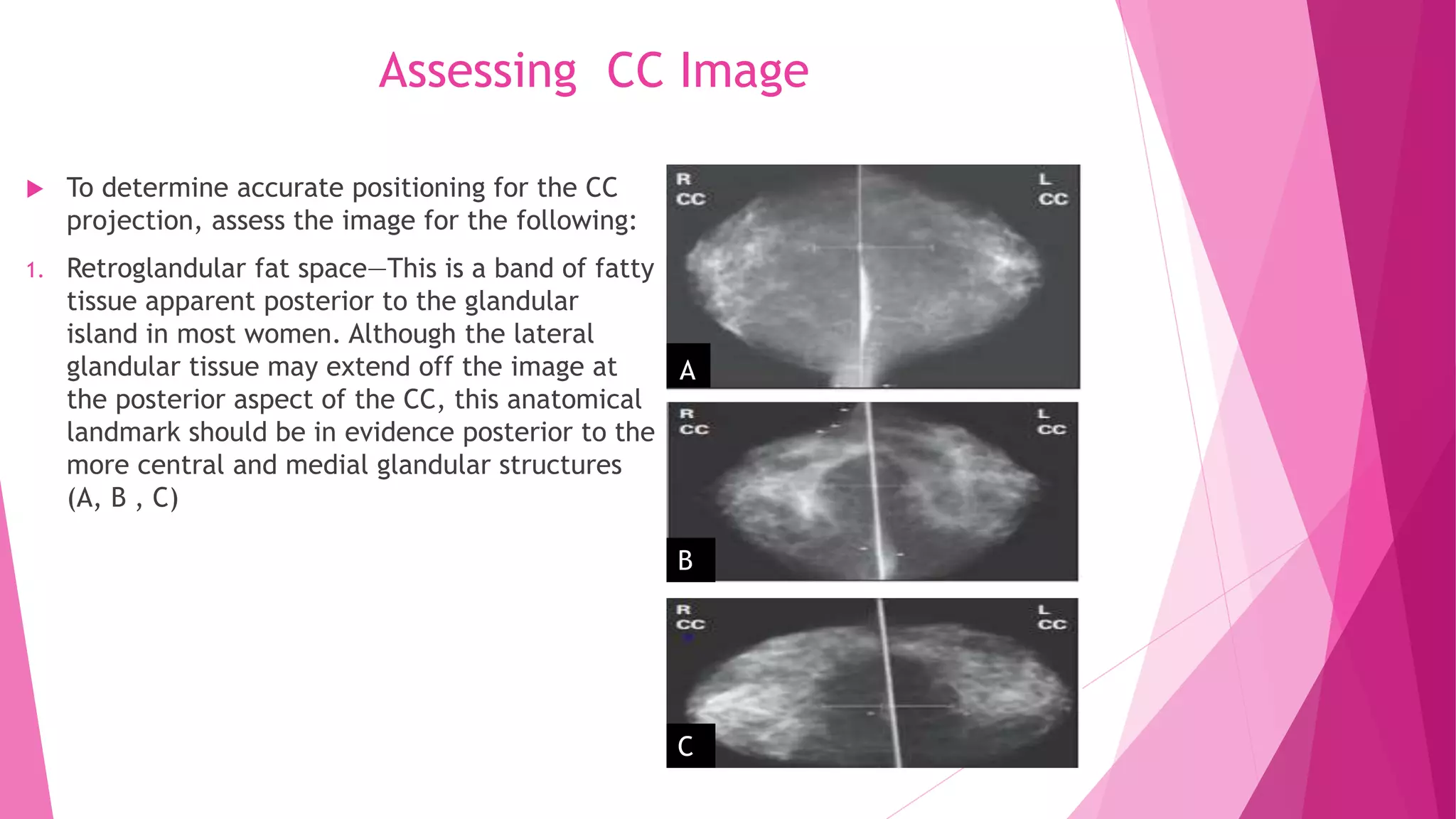
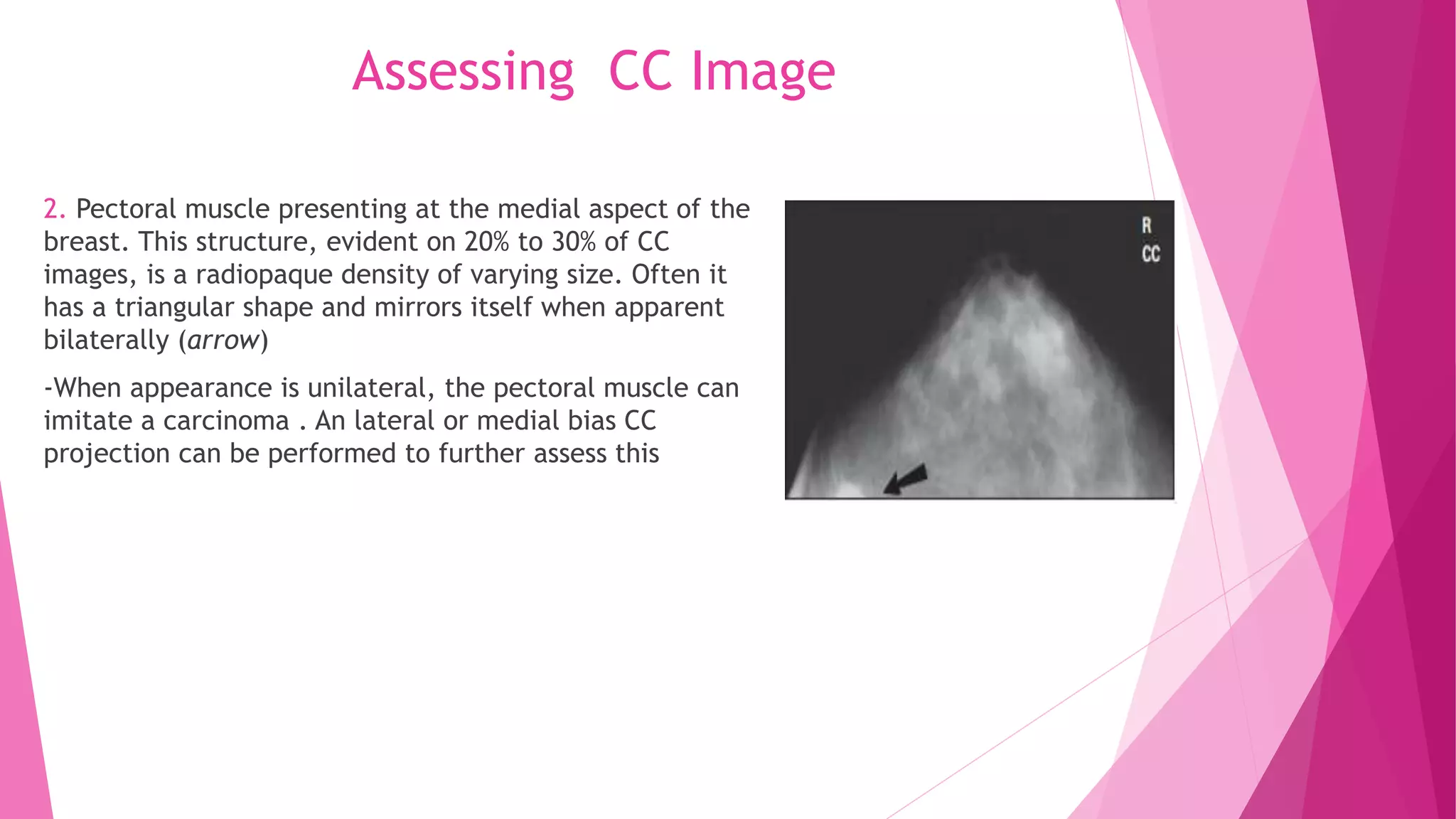
2. Landmarks like the retroglandular fat space and pectoral muscle should be included when possible. The patient is positioned by leaning slightly forward at the waist with shoulders relaxed to allow medial breast tissue to fall onto the image receptor.
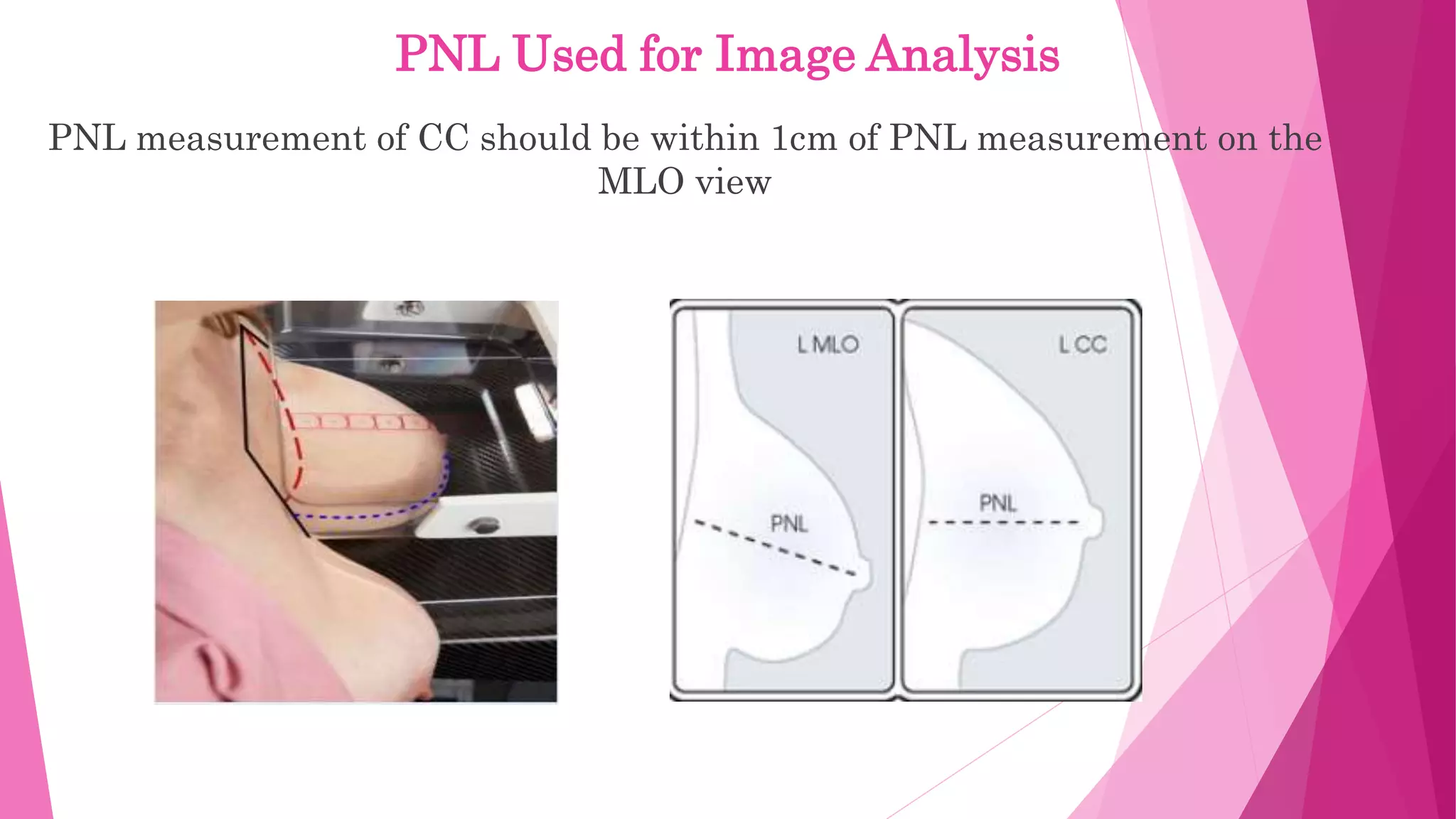
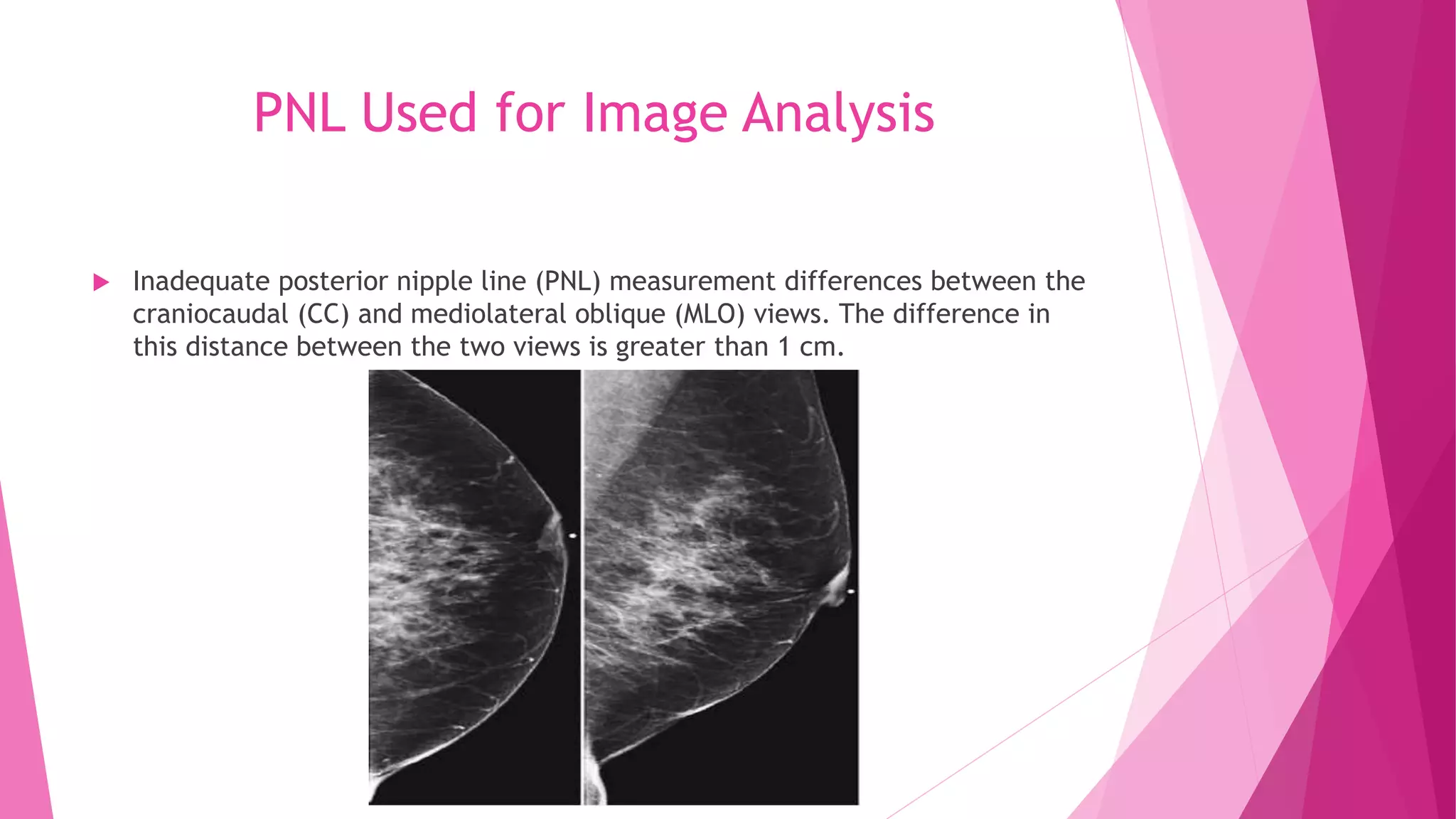
3. The image is assessed to ensure inclusion of key anatomical structures and adequate visualization of breast paren