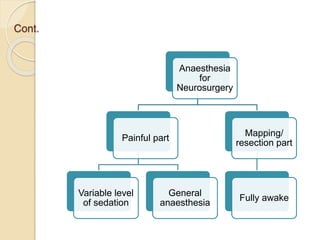
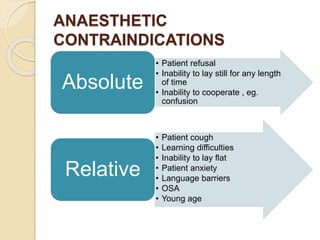
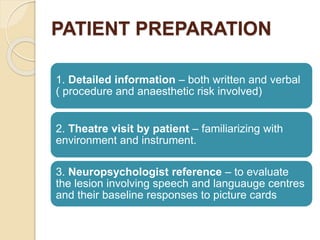
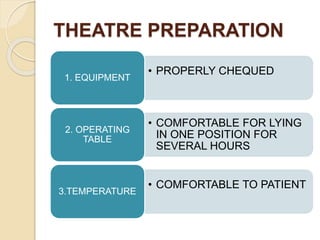
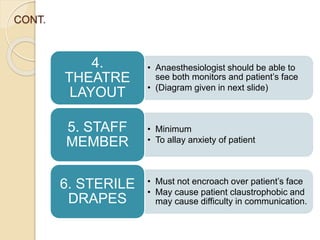
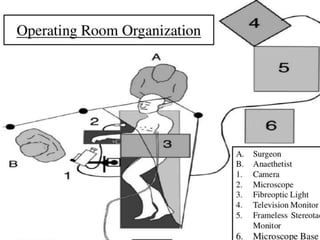
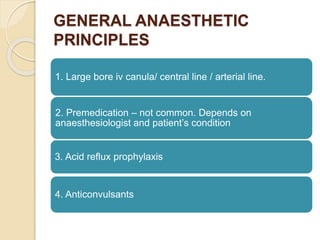
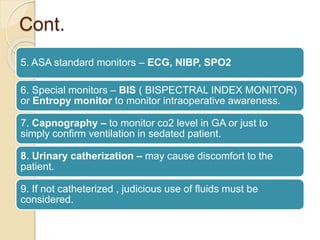
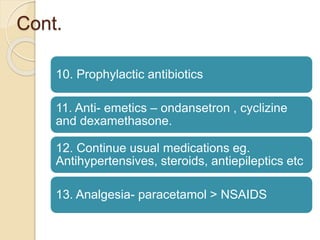
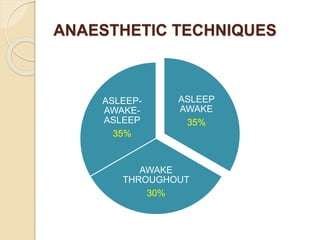
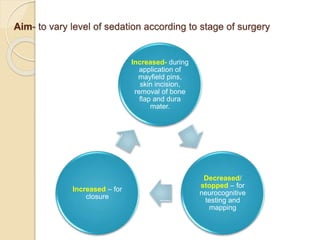
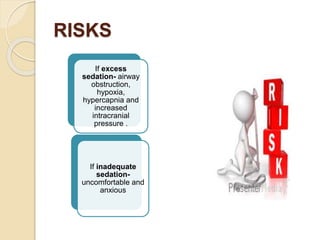
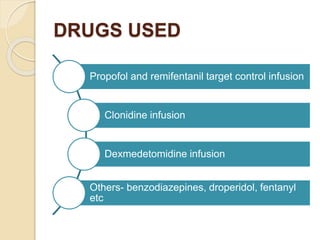
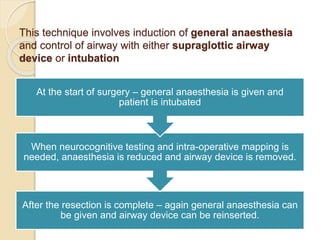
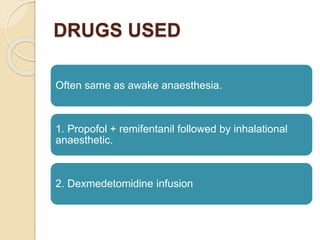
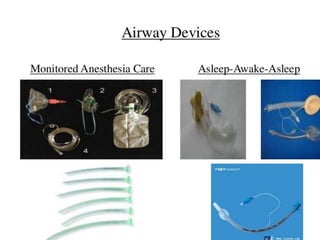
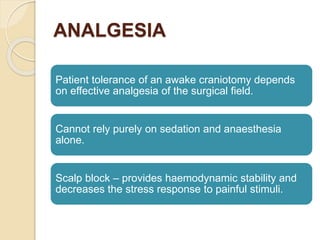
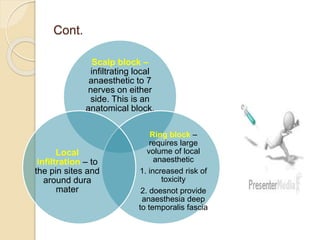
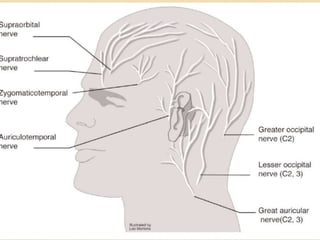
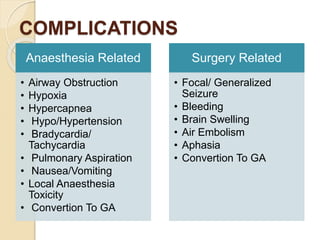
The document discusses the use of awake craniotomy in neurosurgery, highlighting the technique's significance, indications, and anaesthetic management. It outlines patient preparation, anaesthetic principles, techniques, and potential complications, emphasizing the importance of effective analgesia and proper monitoring. The conclusion suggests that awake craniotomy enhances tumor resection and may improve patient outcomes, while noting advancements in technology and anaesthesia practices.