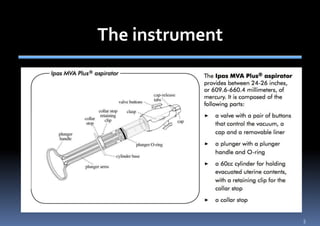
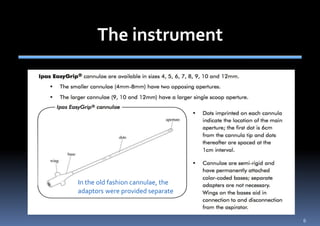
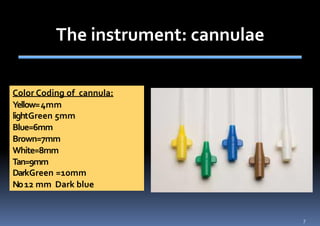
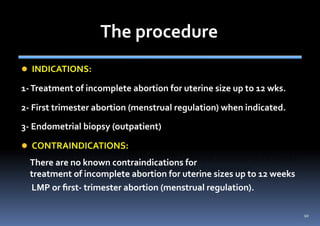
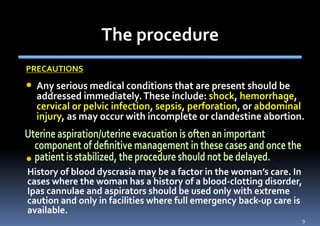
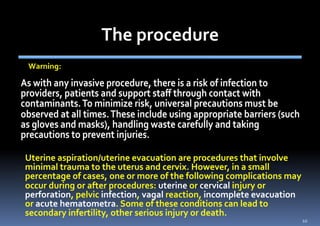
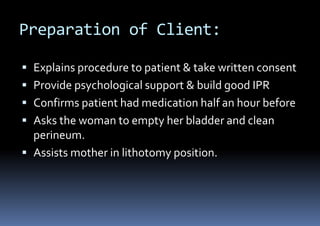
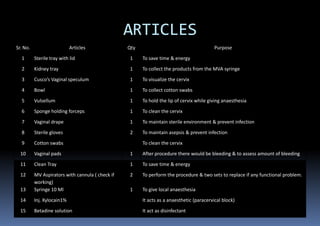
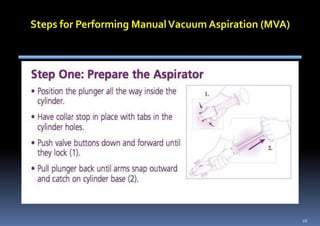
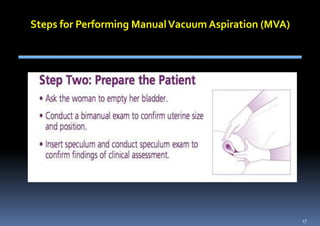
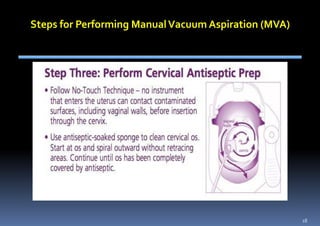
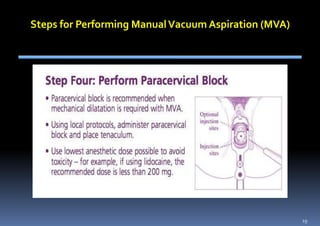
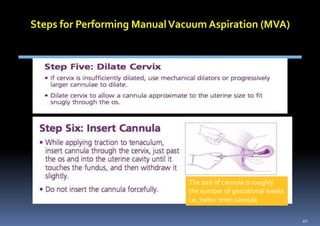
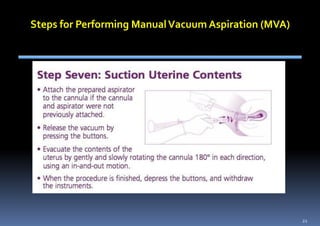
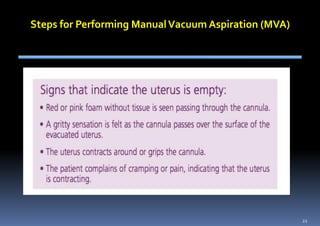
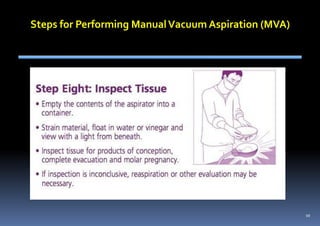
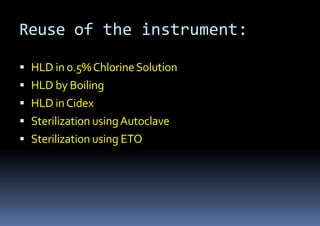
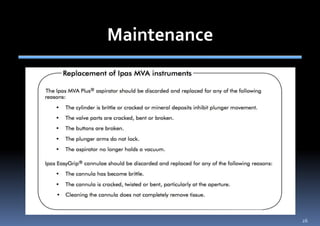
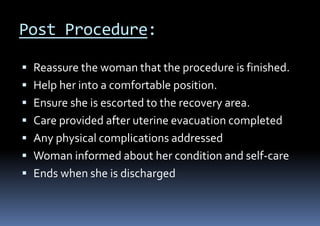
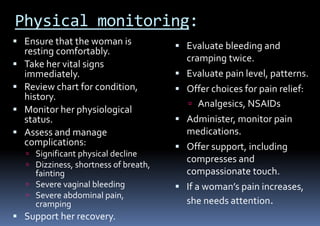
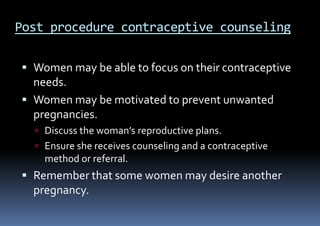
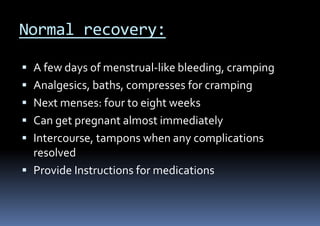
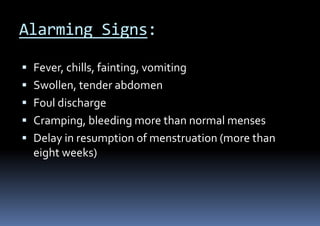
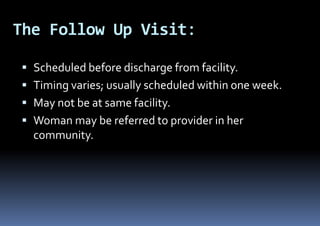
The document provides guidance on performing manual vacuum aspiration (MVA) for abortion, including preparing the client, administering pain management, performing the procedure, monitoring the client's recovery, providing contraceptive counseling, and following up after the procedure. Instructions are given on using appropriate instruments, maintaining aseptic technique, managing complications, and educating the client on what to expect during the recovery process.