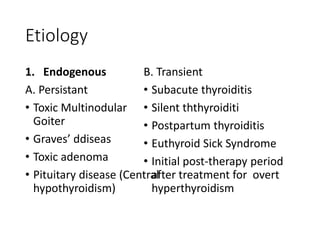
This document provides an overview of subclinical hyperthyroidism (SH), including its classification, prevalence, etiology, natural history, clinical significance, diagnosis, and treatment. SH is defined by low or undetectable thyroid stimulating hormone (TSH) levels with normal free thyroxine and triiodothyronine levels. It is classified based on TSH levels and divided into prevalence depending on factors like age and iodine intake. Causes include persistent or transient endogenous thyroid issues as well as exogenous factors like medication. While its natural history is variable, progression to overt hyperthyroidism occurs in 5% of cases. Treatment aims to restore the euthyroid state and involves confirming the diagnosis, assessing