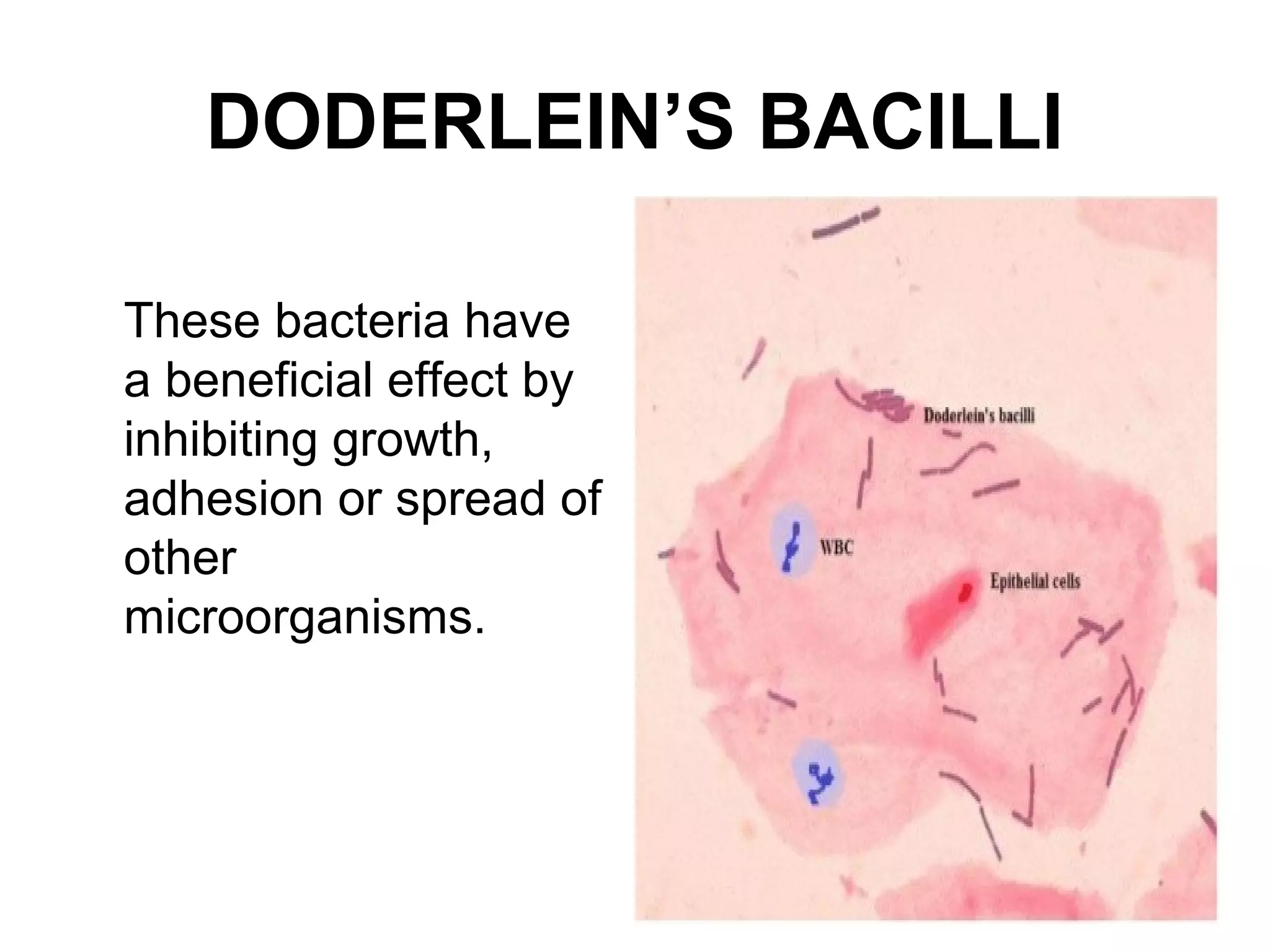
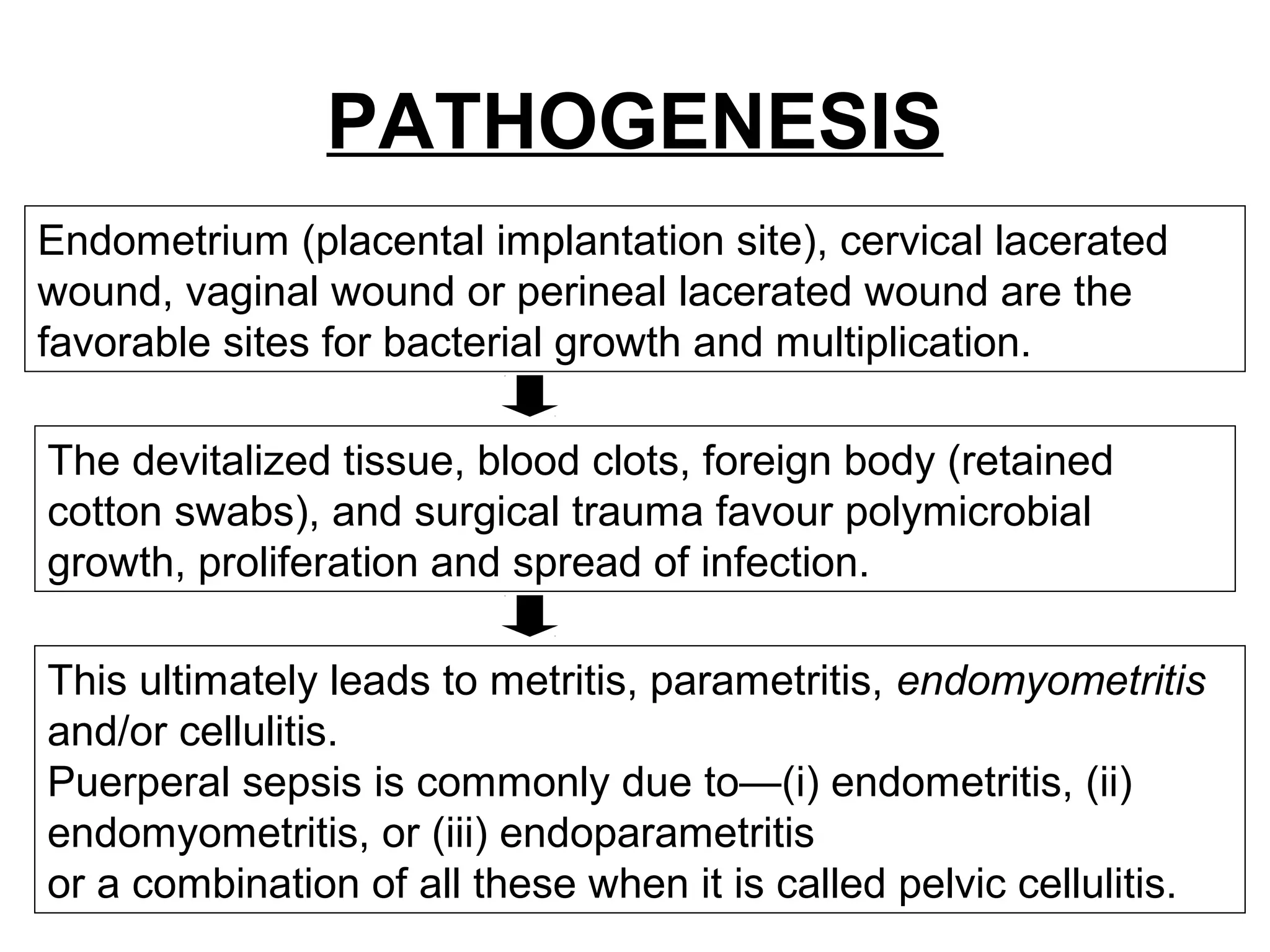
Puerperal sepsis is a serious infection of the genital tract occurring during childbirth or within 42 days postpartum. It is usually caused by bacteria that normally inhabit the vagina, such as Group A streptococcus or E. coli, entering the uterus and surrounding tissues through lacerations or surgical incisions during delivery. Signs include fever, abdominal pain, foul-smelling discharge. Diagnosis involves cultures of vaginal discharge and blood. Treatment consists of intravenous antibiotics, with sometimes surgery to drain abscesses. Nursing care focuses on isolation, hygiene, monitoring for complications like septic shock. Prophylaxis includes good nutrition, infection screening and surgical asepsis during delivery.