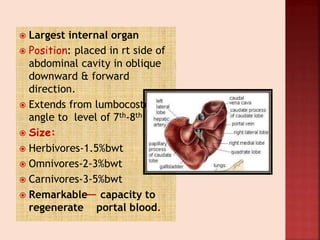
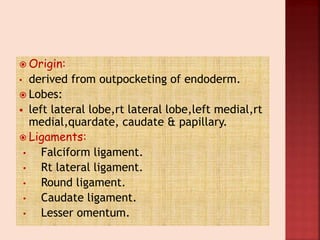
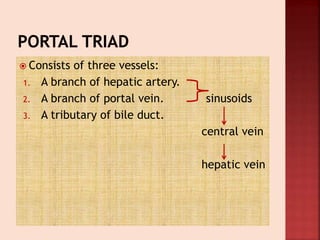
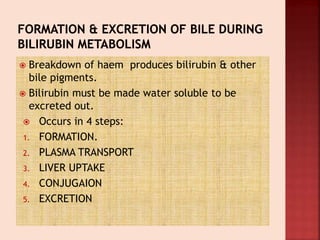
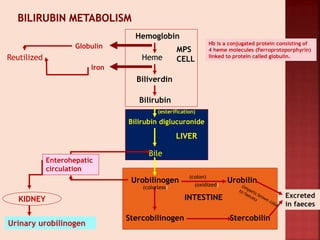
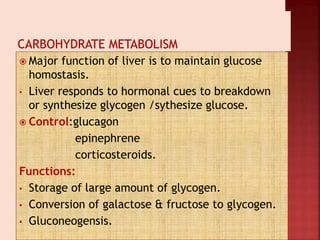
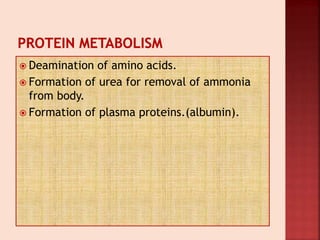
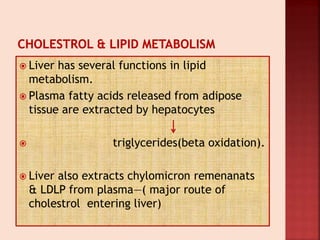
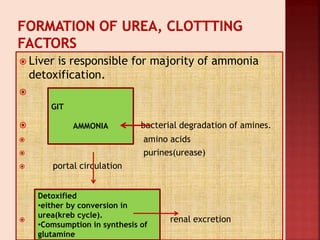
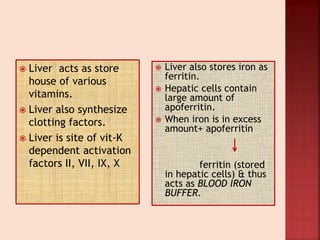
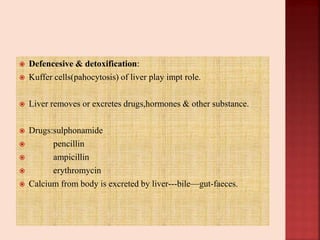
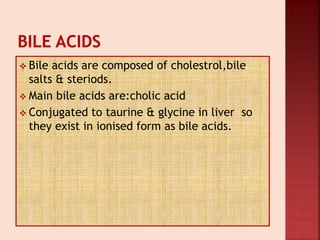
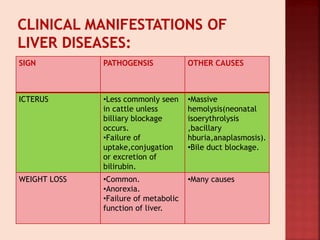
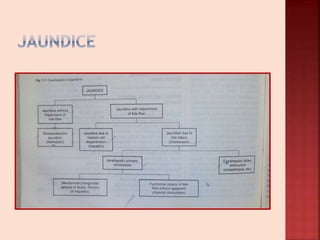
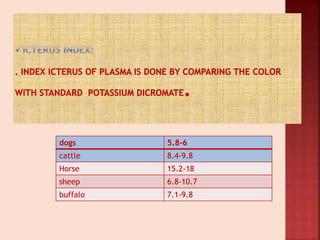
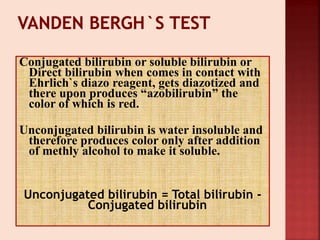
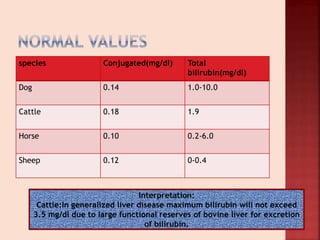
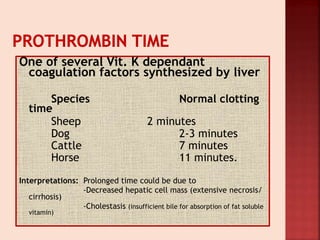
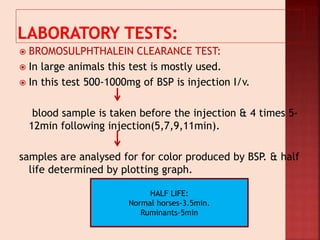
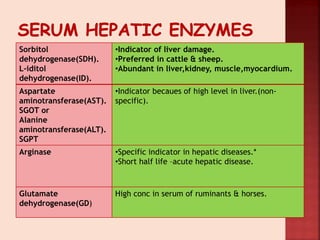
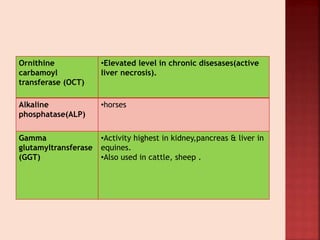
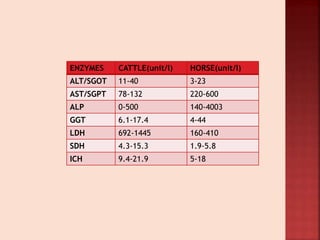
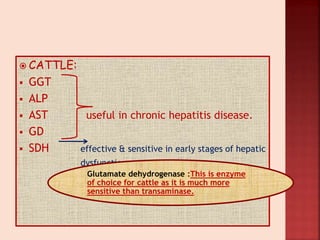
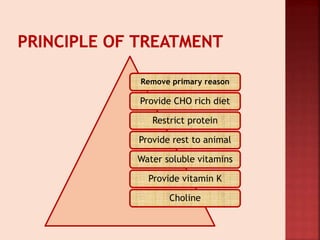
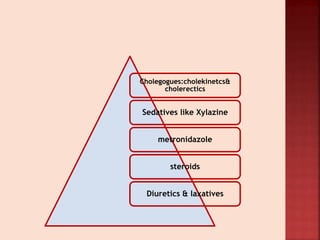
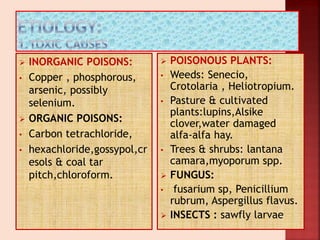
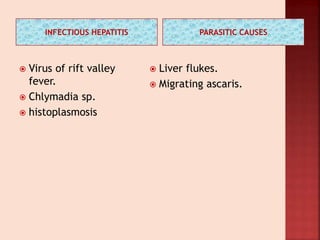
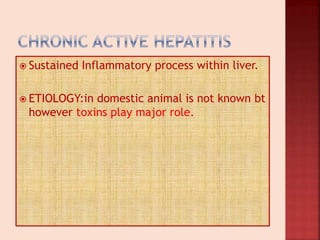
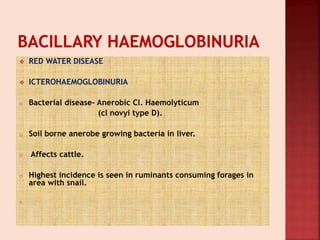
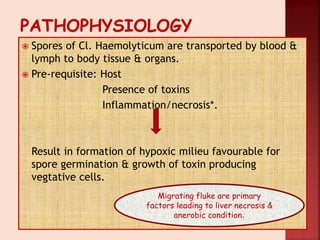
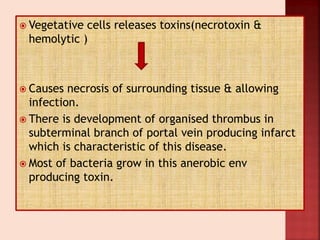
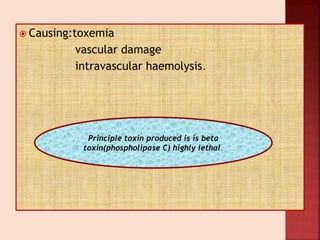
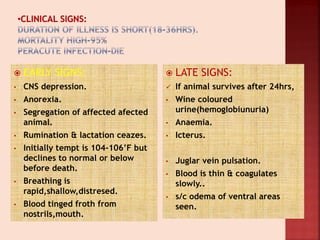
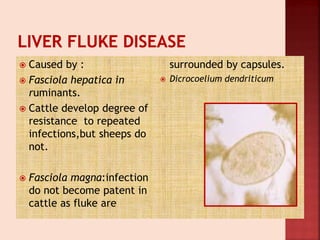
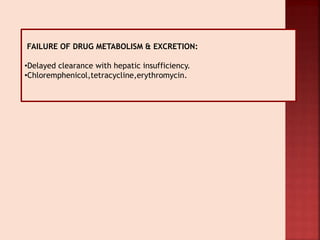
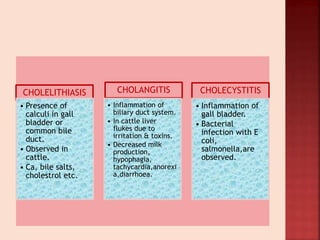
The document provides information about the liver anatomy and functions in various animal species. It discusses the liver's role in metabolizing hemoglobin and bilirubin, maintaining glucose homeostasis, processing amino acids and lipids, detoxifying ammonia, storing vitamins and producing clotting factors. Common liver diseases mentioned include infectious hepatitis, cirrhosis, and red water disease caused by Clostridium haemolyticum bacteria. A number of liver function tests and their reference ranges in different animals are also outlined.