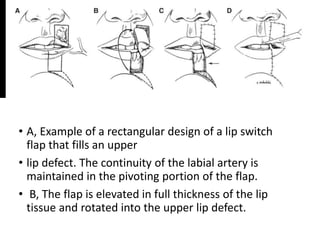
Dr. Akshai George Paul discusses various techniques for lip reconstruction after defects or loss of tissue. Primary closure is used for small defects less than one third of the lip. The Abbe flap and Eslander flap are indicated for defects between one third to half the lip, with the Abbe flap preserving muscular continuity but requiring two stages, and the Eslander flap allowing single-stage reconstruction but resulting in an insensate lip. The Karpandzic flap can reconstruct over half the lip in a single stage while maintaining sensation and function. Larger defects may use the Bernard-Burow cheiloplasty or a free radial forearm flap with palmaris longus for total reconstruction. Post-