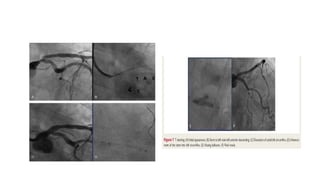
1. Significant unprotected left main coronary artery (ULMCA) disease occurs in 5–7% of patients undergoing CAG and is treated medically has a 3-year mortality rate of 50%.
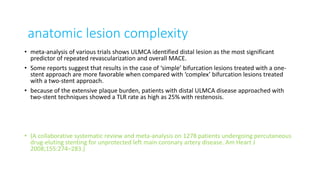
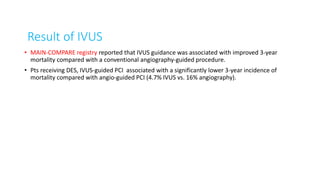
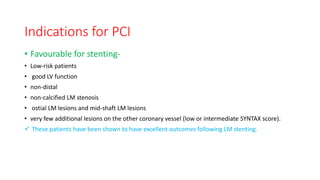
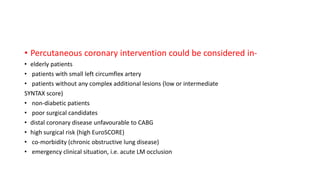
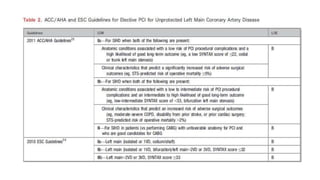
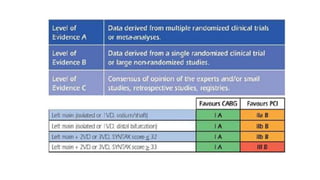
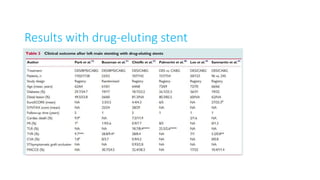
2. Studies have shown PCI with drug-eluting stents for ULMCA disease can achieve low rates of death, MI, and TLR at 12 months compared to bare-metal stents which had high rates of restenosis and mortality.
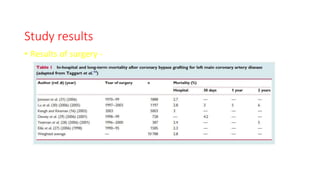
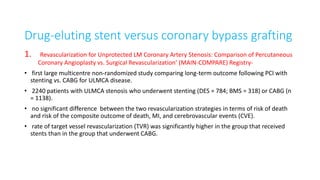
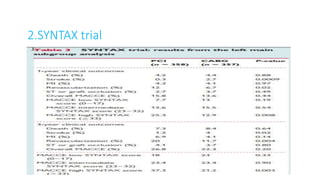
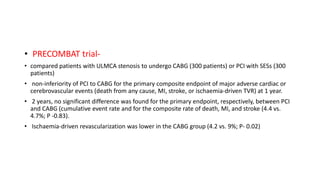
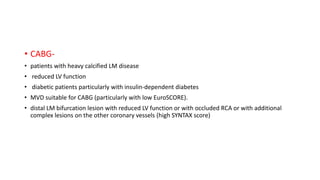
3. While CABG remains the standard of care for many patients, randomized trials found PCI with DES to have non-inferior outcomes to CABG at 1-2 years for death, MI, and stroke in selected patients with low complexity lesions. Rates