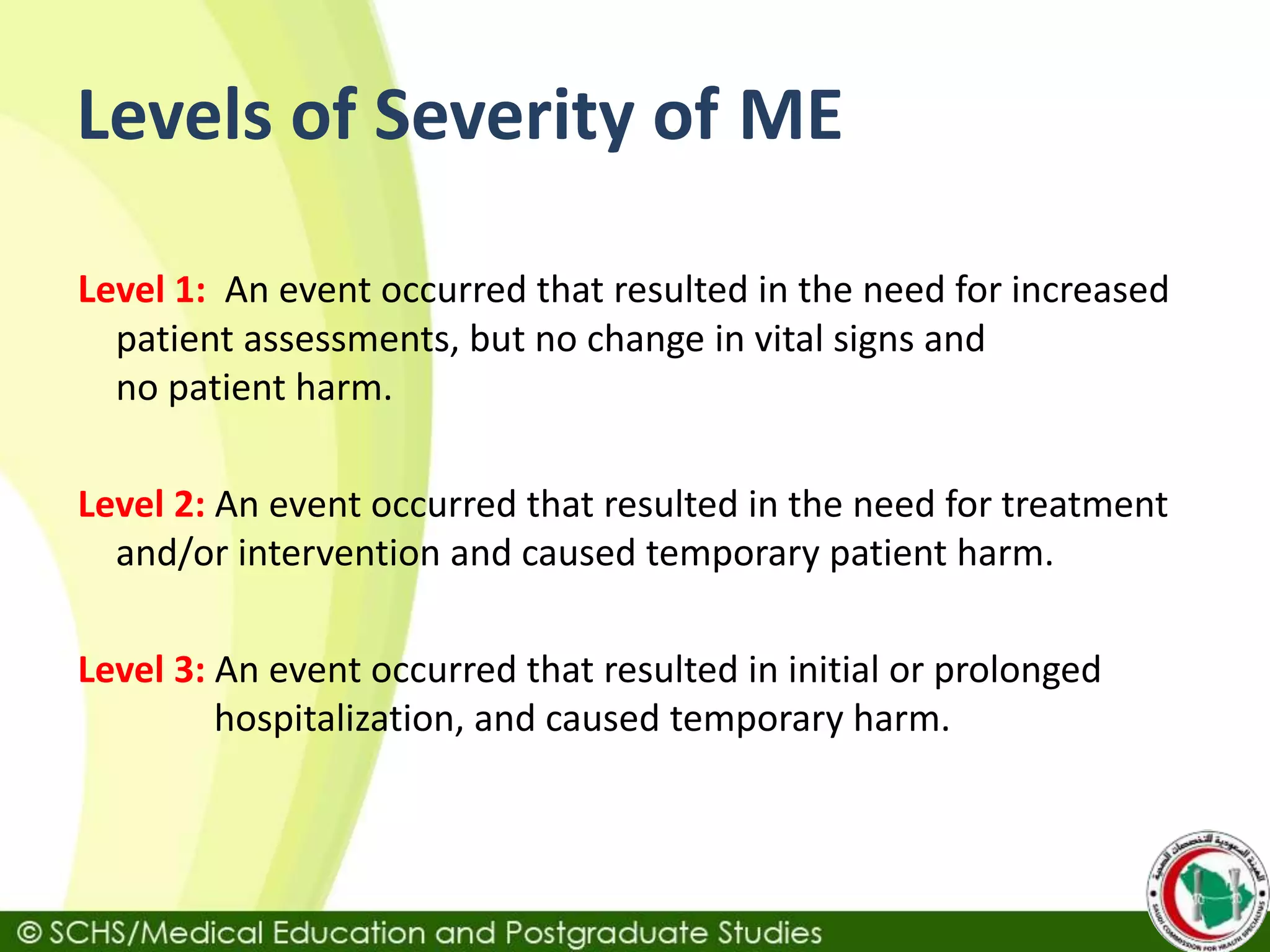
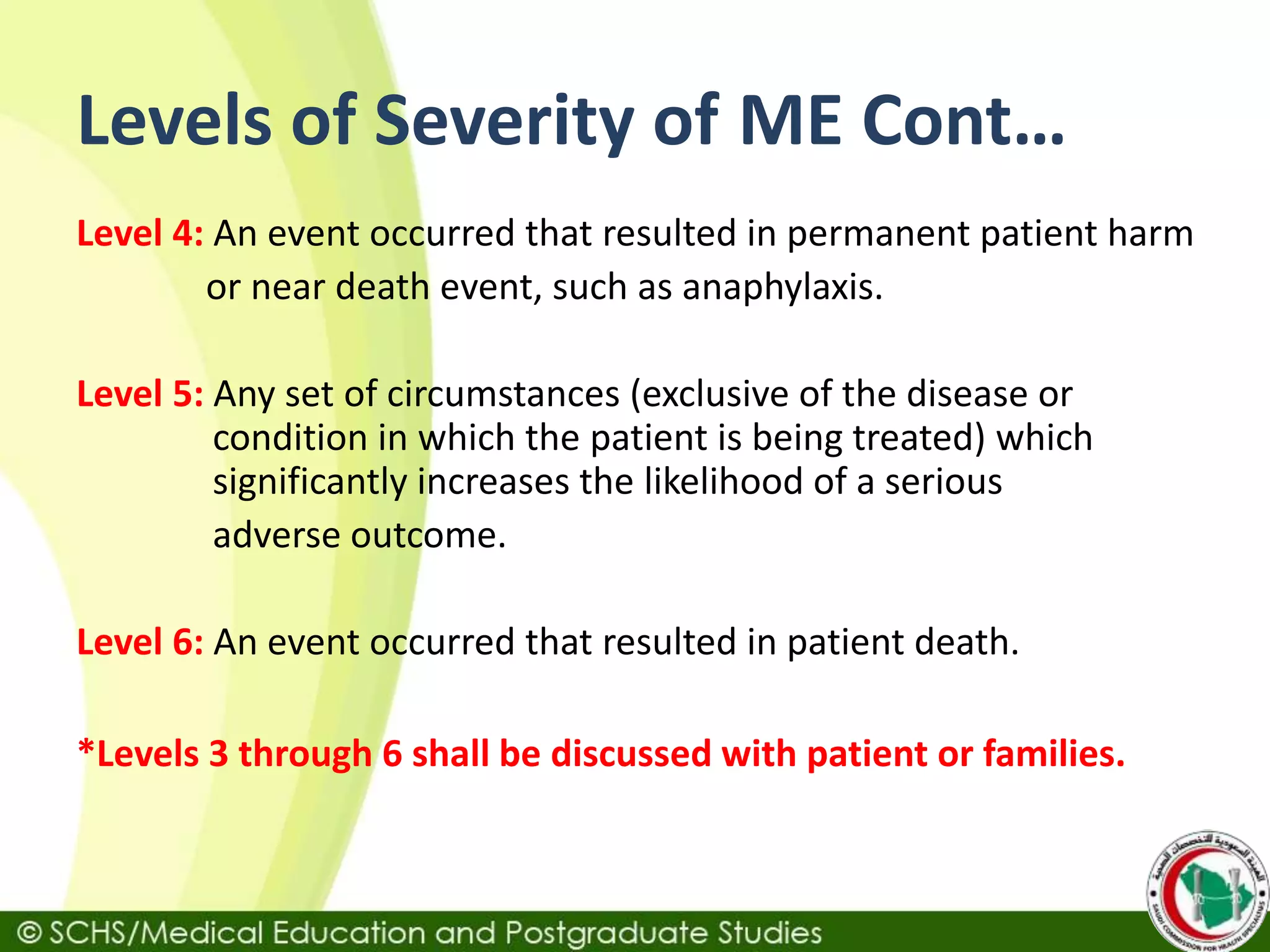
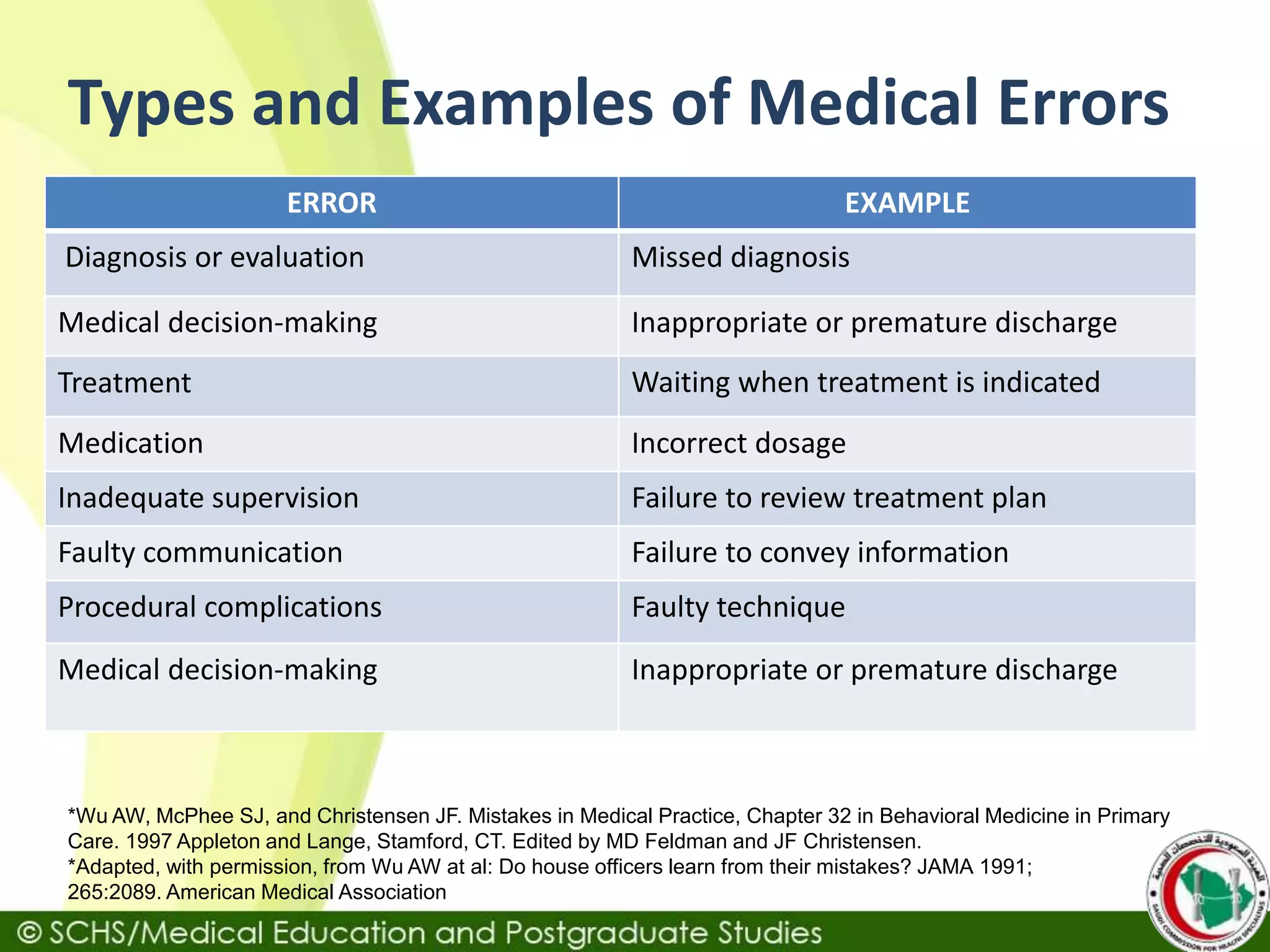
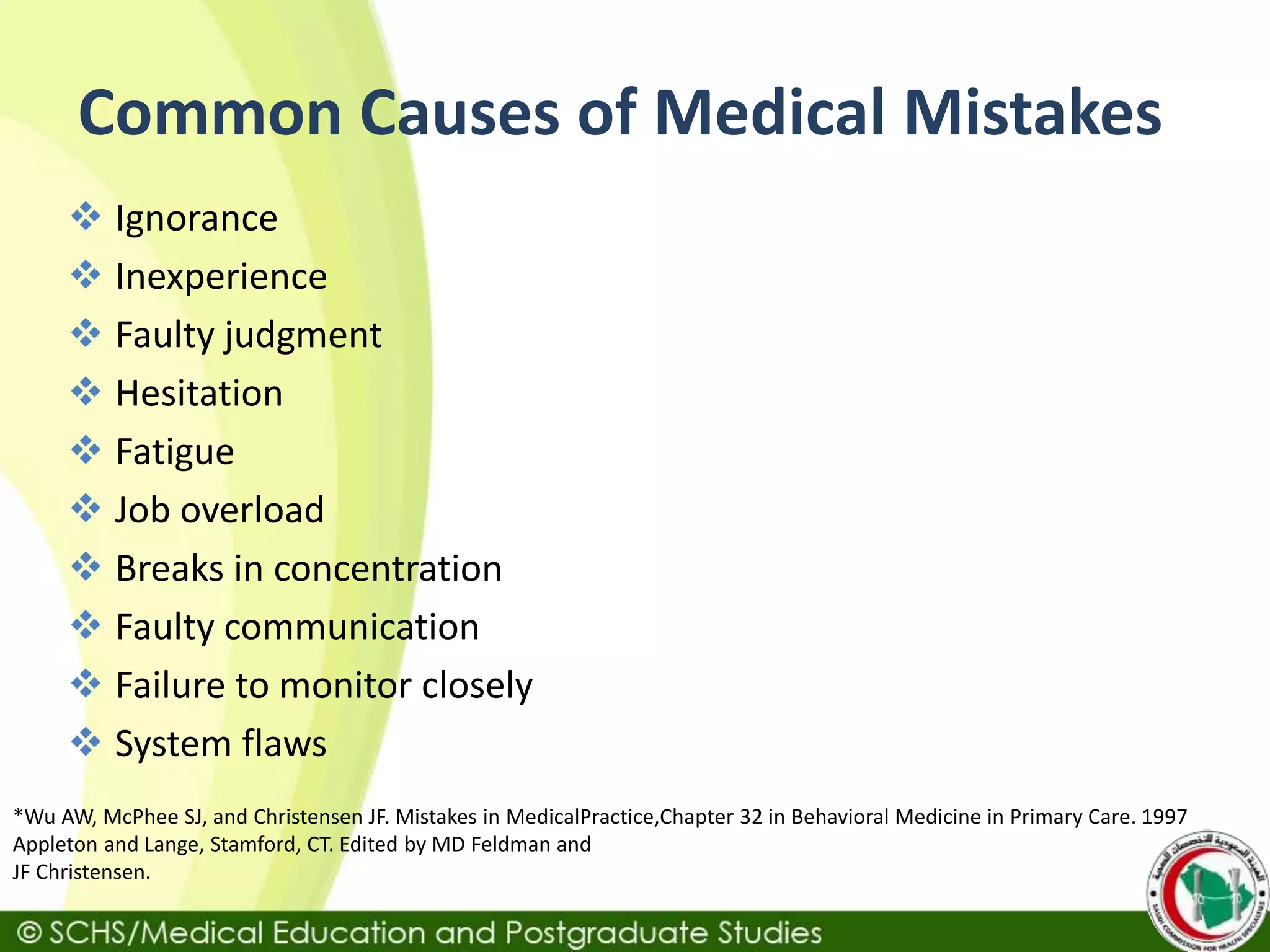
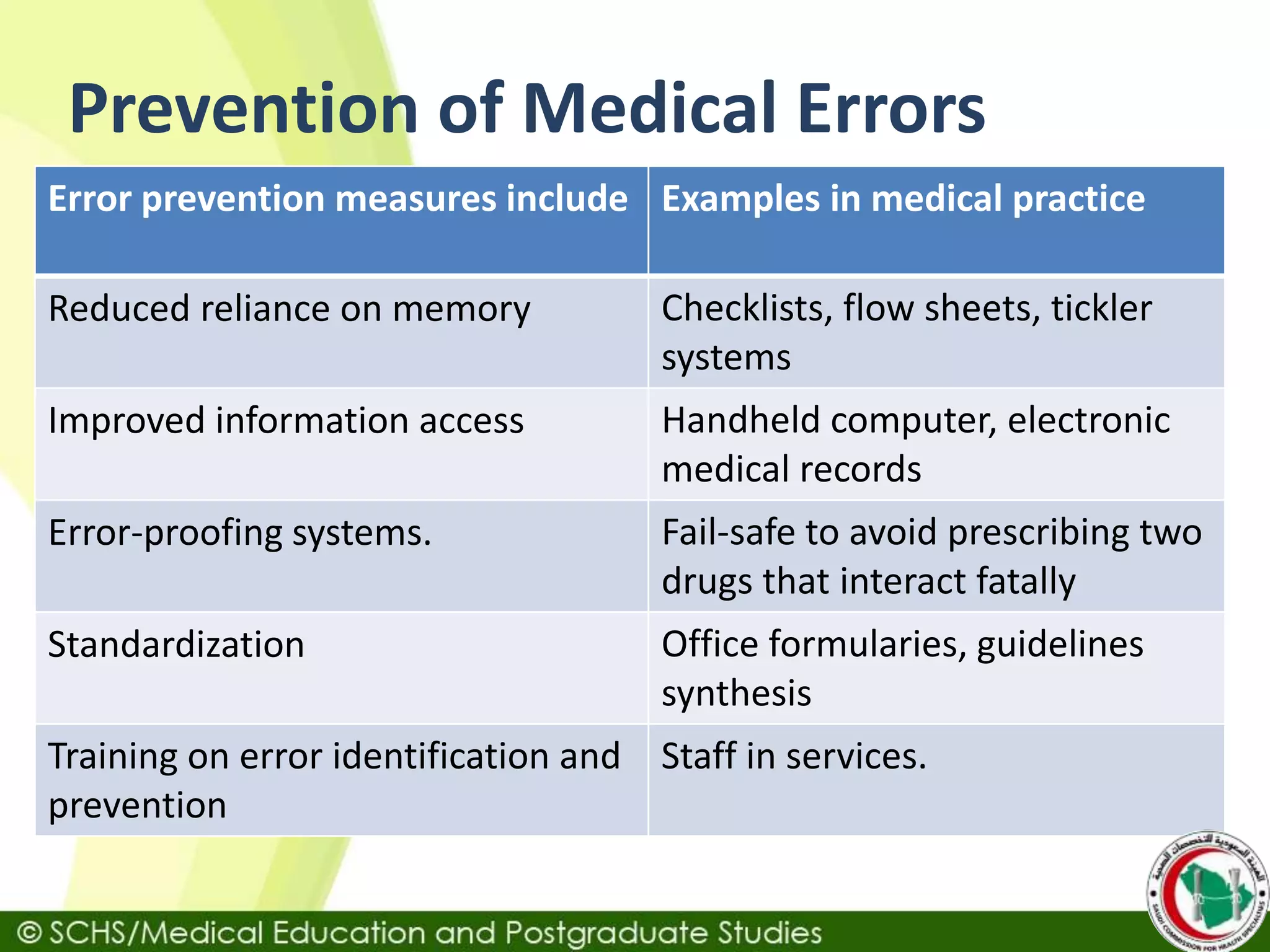
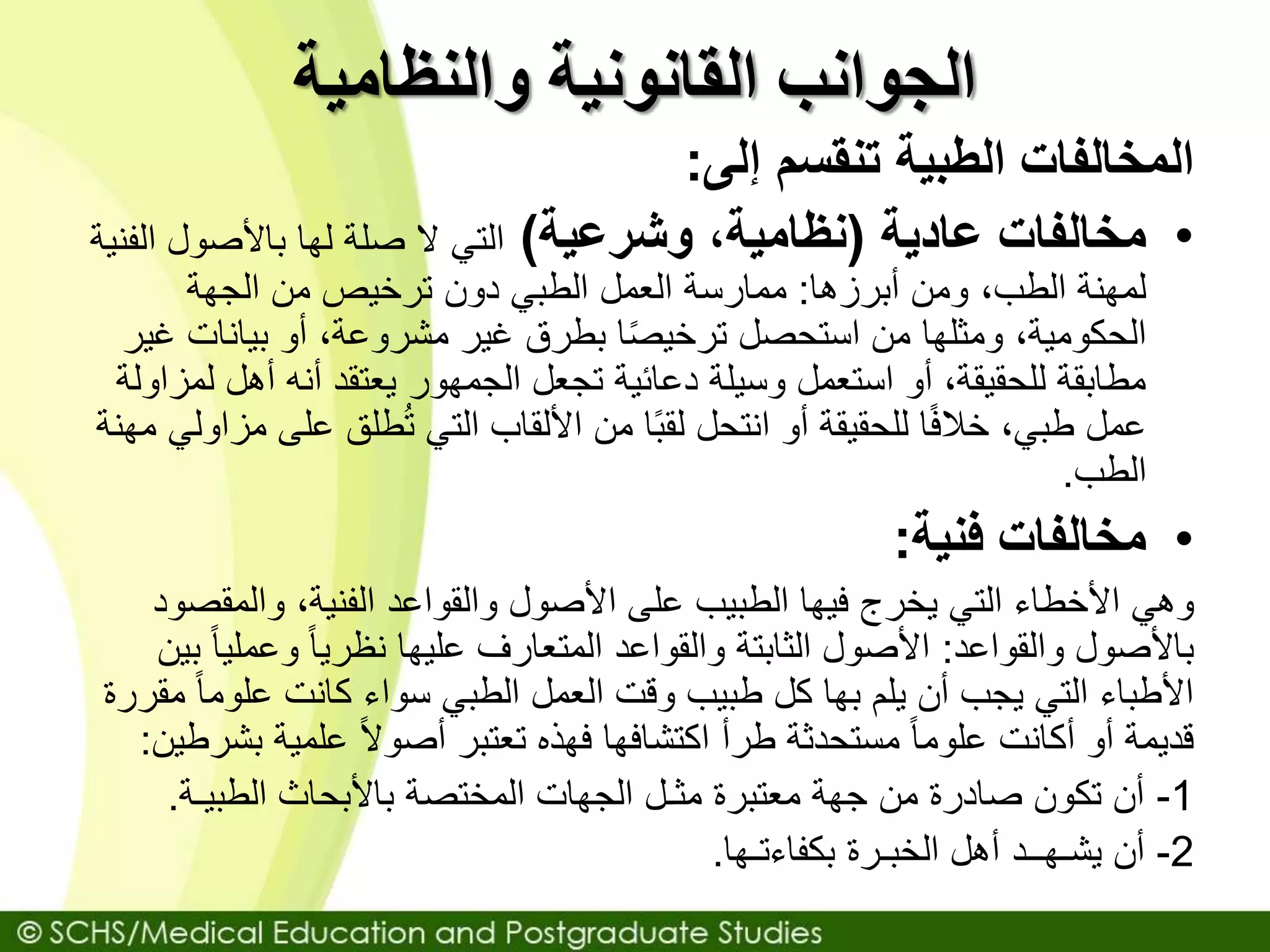
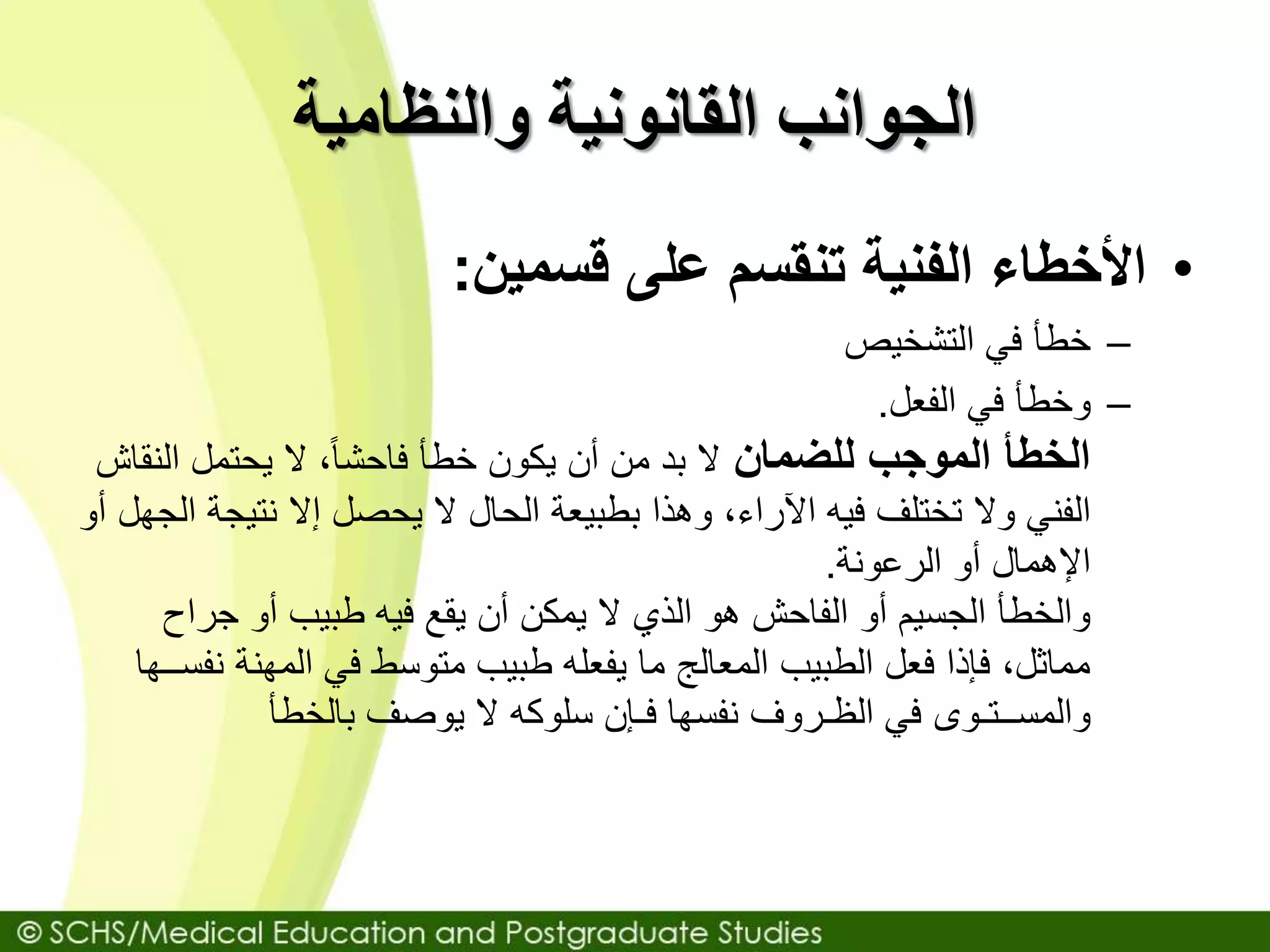
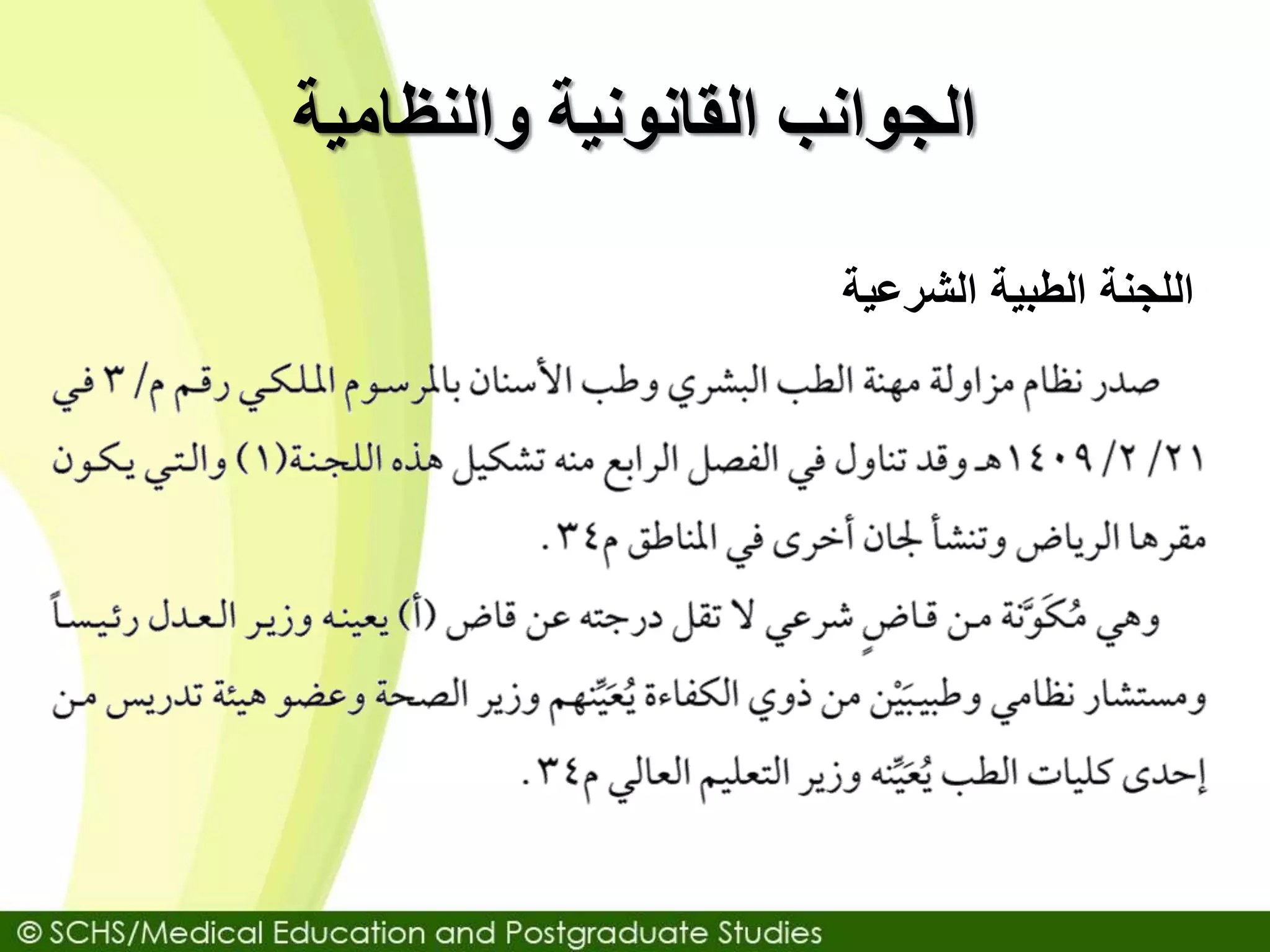
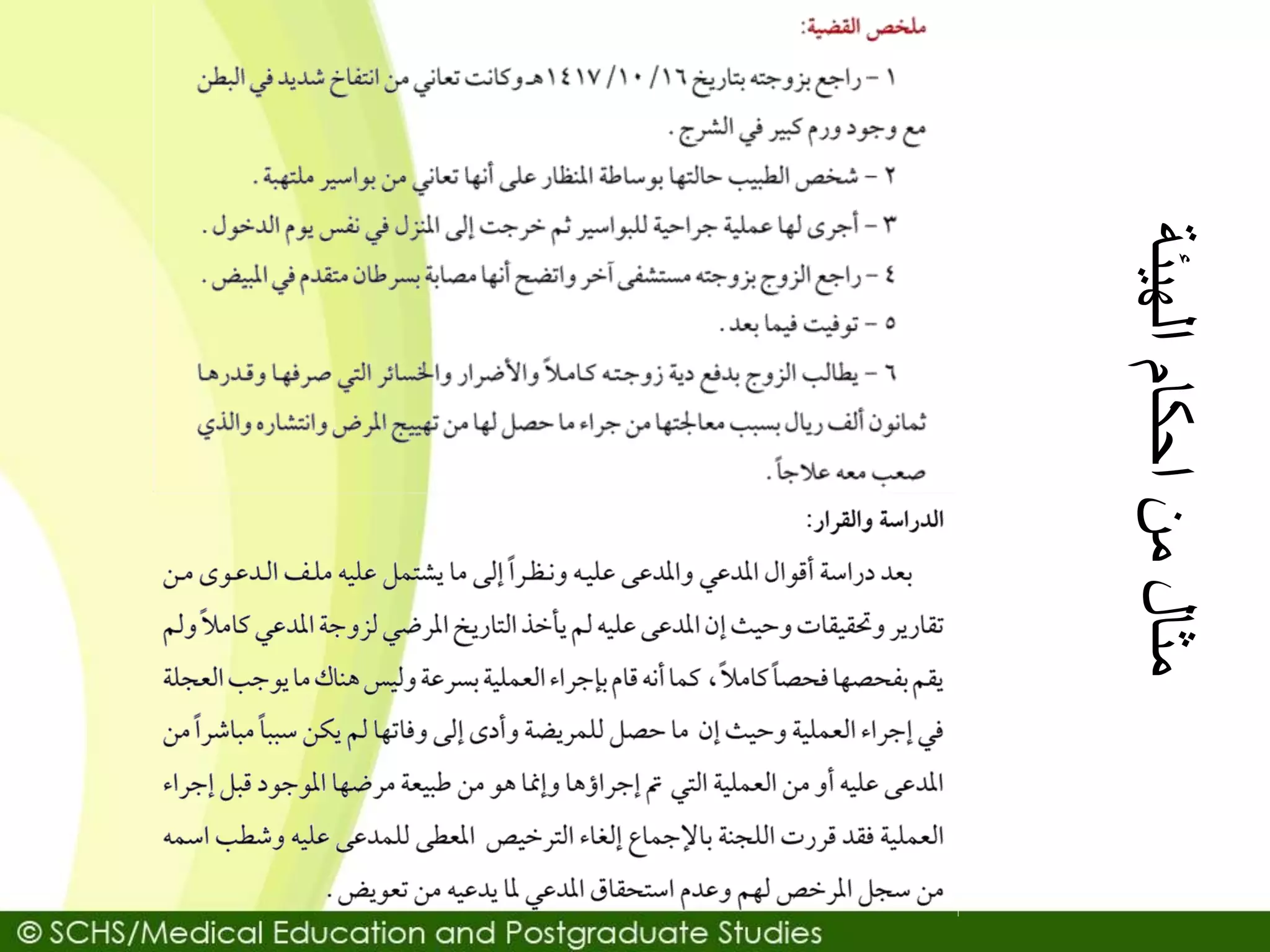
The document provides an overview of medical errors, including definitions, severity levels, types, causes, and prevention strategies. It emphasizes the importance of a culture that supports error reporting and transparency in disclosing mistakes to patients. Additionally, the document discusses ethical considerations and questions related to medical errors faced by healthcare professionals.